Bridging Therapy: What It Is, How It Works, and When It's Used
When you need to stop one medication and start another, your body doesn’t always adjust overnight. That’s where bridging therapy, a temporary treatment used to maintain stability during a switch between drugs or therapies. Also known as transition therapy, it helps prevent withdrawal, relapse, or dangerous spikes in symptoms while your system adapts. Think of it like putting on a safety net before you climb down from a tall ladder—you don’t jump straight to the ground. Bridging therapy keeps you steady.
This isn’t just for mental health or chronic pain. It shows up in thyroid care, when switching from one hormone replacement to another. It’s used in addiction recovery, where someone moves from an opioid to a longer-acting medication like buprenorphine. Even in antibiotics, like when switching from IV to oral treatment, doctors sometimes use overlapping doses to avoid a rebound infection. You’ll see it in asthma too—like when someone moves from a strong inhaler to a milder one, and needs a short-term boost to avoid flare-ups. It’s not a long-term fix. It’s a bridge. And bridges are built for one reason: to get you safely from one side to the other.
What makes bridging therapy work? Timing. Dosage. And knowing what your body can handle. If you jump too fast, you risk crashes—like sudden anxiety, high blood pressure, or even seizures. Go too slow, and you’re stuck on extra meds longer than needed. That’s why it’s never random. Doctors use lab results, symptom logs, and patient feedback to adjust the bridge. For example, someone on long-term steroids might need a gradual taper with a lower-dose version before stopping completely. Or a patient switching antidepressants might take both for a week to avoid serotonin withdrawal. The goal? Smooth transitions. Fewer side effects. Better outcomes.
You’ll find real-world examples in posts about levothyroxine, a thyroid hormone replacement often adjusted with temporary dosing strategies, or how moxifloxacin, an antibiotic sometimes used as a bridge during infection treatment changes fits into broader antibiotic plans. Even benicar, a blood pressure med sometimes replaced with another ARB using a transitional approach, shows how bridging applies beyond just mental health. These aren’t random cases—they’re patterns. People need stability. And bridging therapy delivers it.
There’s no one-size-fits-all bridge. What works for one person might be dangerous for another. That’s why it’s always personalized. If you’re being asked to start a bridging plan, ask: How long? What’s the goal? What if I feel worse? Don’t guess. Know. The posts below cover real cases where bridging made the difference—whether it was easing off opioids, switching antidepressants, or managing chronic conditions without a single setback. You’ll see how timing, dosage, and communication with your doctor turn a risky transition into a controlled, safe step forward.
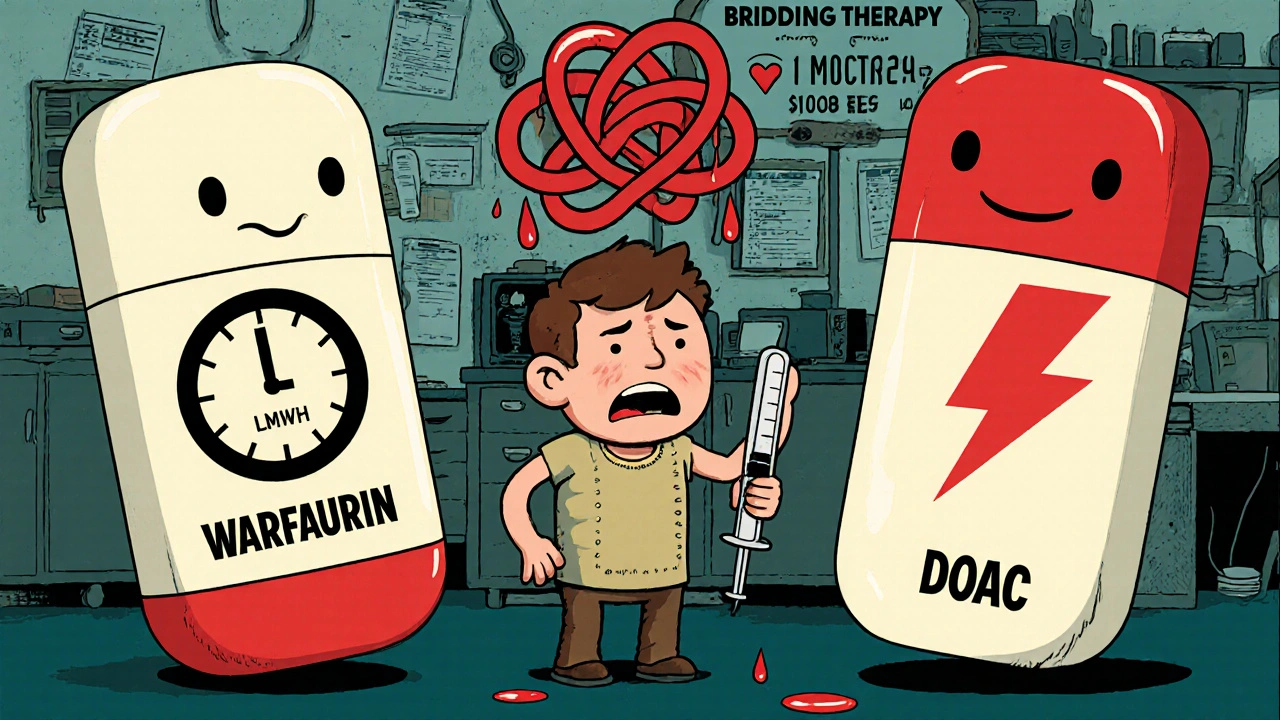
Bridging Therapy: How to Safely Switch Between Blood Thinners
Learn when and how to safely transition between blood thinners like warfarin and DOACs. Bridging therapy isn't always needed-and for most people, it increases bleeding risk without preventing clots.