When your child is sick and needs antibiotics, getting the dose right is only half the battle. The other half? Storing it correctly. Many parents don’t realize that how they keep their child’s liquid antibiotic can make the difference between a quick recovery and a treatment that fails-sometimes dangerously so. The CDC found that improper storage contributes to 15% of pediatric antibiotic treatment failures. That’s not just a number. It’s a child who doesn’t get better, who might need another round of meds, or worse, develop resistance to antibiotics because the dose wasn’t strong enough.
Why Storage Matters More Than You Think
Liquid antibiotics for kids aren’t like pills. They’re suspensions-powder mixed with water right before you give them to your child. Once mixed, they start breaking down. Heat, light, and time all chip away at the medicine’s strength. If it gets too warm, too old, or is stored the wrong way, the antibiotic may not kill the bacteria it’s supposed to. That means the infection lingers, spreads, or comes back stronger. And when that happens, doctors have to reach for stronger drugs, which can lead to more side effects and even antibiotic resistance.It’s not just about effectiveness. Some antibiotics get thick and gross when refrigerated. Kids refuse to take them. Parents think the medicine isn’t working, so they give more. Or they keep using it past its date because they don’t want to waste it. Both are risky moves.
Amoxicillin: The Most Common-and Most Confusing
Amoxicillin is the #1 antibiotic prescribed to kids. About 1 in 3 pediatric antibiotic prescriptions is for this one. And it’s also the most misunderstood when it comes to storage.You might hear conflicting advice: "Refrigerate it." "Keep it at room temperature." "It’s fine either way." All of those can be true-but only if you know the details.
Reconstituted amoxicillin is stable for 14 days whether you keep it in the fridge or on the counter. That’s the official rule from the FDA and major pediatric guidelines. But here’s the catch: refrigerating it makes it taste better. Cold amoxicillin is less sweet, less chalky, and easier for kids to swallow. Room temperature? It can taste like medicine you’d rather not even open. So while both options are safe, most pharmacists and pediatricians recommend refrigeration-not because it’s required, but because it helps your child take it.
Don’t overthink it. If your child tolerates cold medicine, pop it in the fridge. If they gag at the thought of it, leave it on the counter. Just make sure you toss it after 14 days, no exceptions.
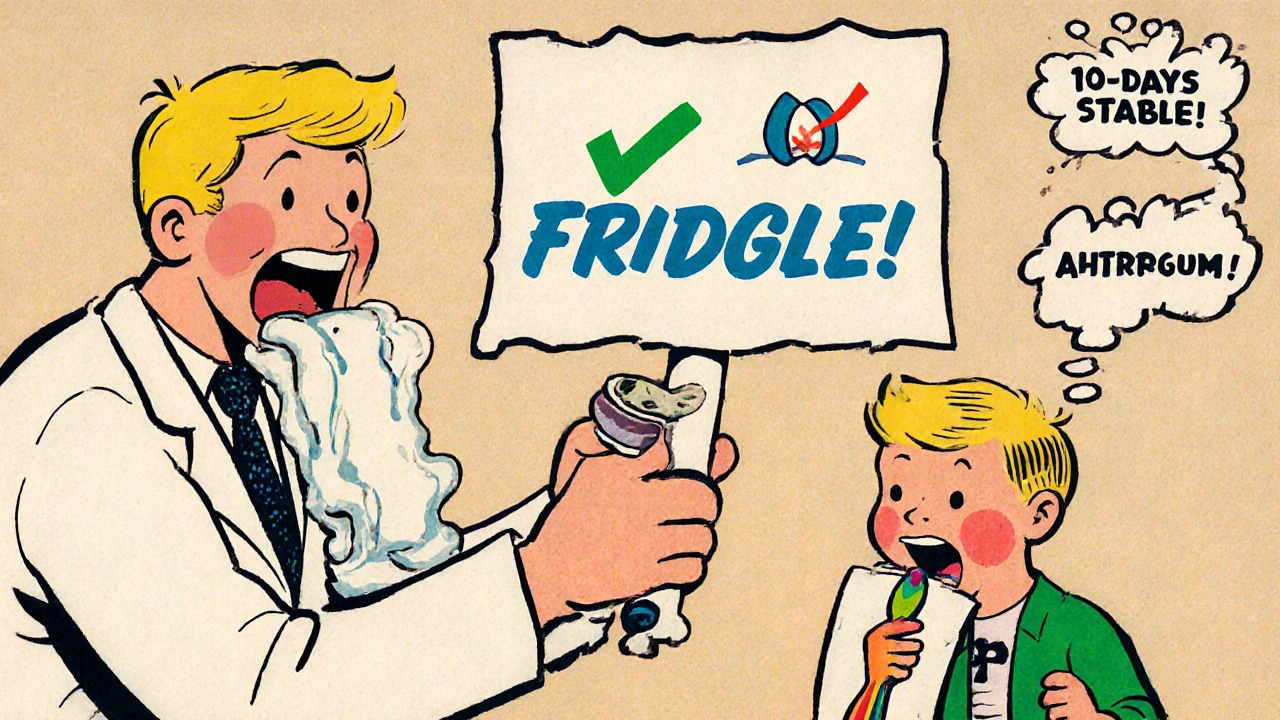
Amoxicillin/Clavulanate (Augmentin): No Room for Mistakes
If your child was prescribed Augmentin, you have less flexibility. This combo drug includes clavulanate, which fights bacteria that resist amoxicillin alone. But clavulanate is fragile. It breaks down fast if it gets too warm.Augmentin must be refrigerated at 2-8°C (36-46°F). No exceptions. Even if your house is cool, don’t leave it on the kitchen counter. The moment it goes above 25°C (77°F), the clavulanate starts losing strength. After just 5 days at room temperature, it can lose nearly 10% of its effectiveness. By day 10, it’s down by more than 15%.
And here’s the hard truth: you have to throw it out after 10 days-even if it still looks fine. No lingering. No "just one more dose." That 15% drop in potency might not sound like much, but in a child’s small body, it’s enough to let bacteria survive and multiply. That’s how resistant infections start.
Azithromycin (Zithromax): Don’t Put It in the Fridge
Azithromycin is another common one, especially for ear infections and respiratory bugs. But here’s the twist: never refrigerate it.When cold, azithromycin turns into a thick, goopy mess. It’s hard to pour, hard to measure, and nearly impossible for a child to swallow. A 2023 taste study found that 37% of kids refused it when refrigerated. That’s not a small number-it’s nearly 4 in 10 children who won’t take their medicine because of how it’s stored.
Keep azithromycin at room temperature (20-25°C / 68-77°F). It stays stable for 10 days. It tastes better. It flows better. And your child is more likely to take it without a fight.

Other Antibiotics That Hate the Fridge
Azithromycin isn’t the only one. Several other common pediatric suspensions should never be chilled:- Clarithromycin - Thickens and becomes gritty
- Clindamycin - Loses taste and texture
- Sulfamethoxazole/trimethoprim (Bactrim) - Forms clumps
- Cefdinir - Changes color and taste
These aren’t guesses. These are documented effects from studies published in peer-reviewed journals. If you’re unsure, check the pharmacy label or ask the pharmacist. If it says "Do not refrigerate," trust it.
When in Doubt, Ask the Pharmacist
Pharmacists are your secret weapon. They see hundreds of these bottles every week. They know which ones need refrigeration, which ones don’t, and which ones have tricky storage rules.Before you leave the pharmacy, ask: "Should this be refrigerated? And how long can we keep it?" Most pharmacies now put a sticky note on the bottle with the discard date and storage instructions. If they don’t, ask them to write it on there. Don’t assume the label on the bottle says it all-many don’t.
The Infectious Diseases Society of America says it plainly: "When in doubt, check the pharmacy label. Most of the time, an extra sticker will be on the bottle that says something like 'Keep in Refrigerator' or 'Refrigerate.' You can also ask the pharmacist to be sure."
Discard Dates Are Not Suggestions
This is the #1 mistake parents make. They keep the bottle around because it’s expensive. Or they think, "It still looks fine." Or worse-"My child still has a cough, maybe this will help."Here’s what happens when you use expired suspension:
- Antibiotic strength drops by 15-20% after the discard date
- It doesn’t kill the bacteria
- The infection comes back
- Bacteria become resistant
- Next time, your child might need a stronger, more expensive antibiotic-or even hospital care
Dr. Jessica Smith, a pediatric pharmacist at Children’s Hospital of Philadelphia, says: "The single most common error I see is parents continuing to use antibiotics beyond the designated discard timeframe. That’s 27% of treatment failures we observe."
Set a reminder on your phone. Write the discard date on the bottle with a Sharpie. Put a sticker on the fridge. Do whatever it takes. Once the clock hits zero, throw it out. No exceptions.
Where to Store It (and Where Not To)
Your kitchen counter? Fine-if it’s cool and away from the stove. The bathroom cabinet? No. Humidity and heat from showers ruin medicine. The car? Never. Even in winter, the inside of a car can hit 40°C (104°F) in minutes.Best spots:
- Back of the refrigerator (not the door-temperatures fluctuate there)
- A cool, dark cupboard away from sunlight and appliances
- A dedicated mini-fridge just for meds (yes, some parents do this-and they report fewer treatment failures)
Avoid:
- Windowsills
- On top of the TV or microwave
- Under the sink
- Anywhere kids can reach
The American Association of Poison Control Centers reports 60,000 U.S. children under 5 are treated every year for accidental medicine poisoning. Store everything up and away-even if it’s just a half-full bottle.
Signs Your Antibiotic Has Gone Bad
You don’t need a lab test to tell if your suspension is spoiled. Look for these red flags:- Discoloration: It was clear, now it’s cloudy or has dark specks
- Change in smell: It smells sour, fermented, or off
- Change in taste: It tastes bitter, metallic, or strange
- Excessive sediment: You shake it and it doesn’t mix back in
- Separation: Layers form even after shaking
If you see any of these, throw it out. Don’t risk it. Even if it’s before the discard date, if it looks or tastes wrong, it’s not safe.
What to Do If You’re Still Confused
You’re not alone. A 2023 GoodRx survey found that 52% of parents store antibiotics in the wrong place. Nearly 4 in 10 keep them past the discard date. And 68% of parents say they’re unsure what to do.Here’s your simple checklist:
- Check the pharmacy label for storage instructions
- Look for a discard date sticker
- If it says "Refrigerate," put it in the fridge
- If it says "Store at room temperature," keep it cool and dry
- Write the discard date on the bottle
- Set a phone reminder
- Throw it out on the discard date-even if it looks fine
- Never reuse leftover antibiotics for a new illness
If you’re still unsure, call the pharmacy. They’re happy to help. Better yet, ask during the visit when you pick up the prescription. Don’t wait until the bottle’s half-empty and you’re staring at it wondering if it’s still good.
Final Thought: It’s Not Just About Medicine-It’s About Safety
Storing antibiotics right isn’t just about making sure the medicine works. It’s about protecting your child from resistant infections. It’s about avoiding unnecessary doctor visits, hospital stays, and stronger drugs with harsher side effects. It’s about being the kind of parent who pays attention to the details-because those details matter.And if you’re worried about wasting medicine? You’re not alone. But the cost of a failed treatment is far higher than the cost of a $20 bottle of liquid antibiotic.
When in doubt, throw it out. Your child’s health is worth more than the bottle.







Michael Fitzpatrick
Man, I wish I’d known all this when my daughter had that nasty ear infection last year. We kept the azithromycin in the fridge because the pharmacist said "keep it cool," and she refused to take it for three days straight. We ended up throwing it out and going back for a new prescription. Total waste. Now I keep a little sticky note on the fridge with the storage rules for each med. It’s crazy how much variation there is between antibiotics. I used to think all liquid meds were the same. Not anymore.
Also, the part about Augmentin losing potency after 5 days at room temp? Mind blown. We had a bottle sitting on the counter for a week because we were too lazy to put it away. Hope we didn’t make things worse.
Thanks for laying this out so clearly. I’m printing this out and taping it to the medicine cabinet.
Justin Daniel
So let me get this straight - amoxicillin’s fine on the counter, but if you chill it, your kid might actually swallow it without screaming? And Augmentin’s like a fine wine that turns to vinegar if you breathe on it wrong?
Look, I’m not a doctor, but I am a dad who’s had three kids go through antibiotics, and I’ve seen everything from the goopy azithromycin to the chalky amoxicillin that tasted like wet chalkboard. The truth? The fridge isn’t magic. It’s just a better taste test. If your kid’s gagging, don’t force it. Just keep it cool and toss it after 14 days. Simple.
Also, if your pharmacist doesn’t give you a discard sticker, ask for one like it’s your job. They’ll do it. I’ve seen them write on duct tape when the label ran out of space.
Melvina Zelee
ok so i just realized i’ve been storing my son’s clindamycin in the fridge like a total idiot 😅 i thought all meds needed to be cold. now i’m panicking because he took it for 5 days before i read this. but like… it didn’t taste gross, he took it fine, and he’s better now. sooo… did i ruin his immune system? lol
anyway, this is so helpful. i’m gonna print this and stick it next to the toothpaste. also, i’m writing the discard date on the bottle with a sharpie now. no more guessing. thanks for this. i feel like a better parent already.
Daniel Jean-Baptiste
Good info but honestly the real issue is that pharmacies don’t make this easy. I’ve had bottles with no labels, no stickers, no instructions. Just a plastic cup with liquid inside and a receipt that says "amoxicillin 5ml bid"
Parents shouldn’t have to Google this stuff. Pharmacies need to put a clear, bold sticker on every bottle. Not a tiny print footnote. A big red box that says "DO NOT REFRIGERATE" or "KEEP COLD"
Also, why is it that every time I ask, the pharmacist says "oh it’s fine either way"? No it’s not. That’s why we’re here. This isn’t rocket science. It’s medicine. Be clear.
Ravi Kumar Gupta
Bro, this is the most important post I’ve read in my entire life. In India, we have this habit - we keep leftover antibiotics in the cupboard like they’re spices. My cousin’s kid got sick last month with the same cough, and they gave him the old amoxicillin from last year. He got worse. Ended up in the hospital. Antibiotic resistance is not a joke. It’s a silent killer.
And don’t even get me started on how pharmacies here just hand out bottles without instructions. No stickers. No dates. No nothing. We’re lucky if they even tell us the name.
Thank you for this. I’m sharing this with every parent I know. We need to stop treating medicine like a buffet. It’s not food. It’s science.
Rahul Kanakarajan
Wow. Another parent blog telling us how to raise our kids. Thanks for the lecture. Did you also write a 12-page PDF on how to wipe a baby’s butt properly?
Look, I get it. You’re trying to sound smart. But here’s the truth - most parents don’t care about 15% potency loss. They care if their kid stops crying. If the medicine works, they use it. If it doesn’t, they go back to the doctor. Simple.
And let’s be real - 90% of these "discard dates" are just a way for pharmacies to sell more bottles. You think they’re worried about your kid? They’re worried about liability.
Stop fearmongering. Just give the kid the medicine. If it helps, great. If not, go back. Life isn’t a clinical trial.
New Yorkers
Oh wow. So now we’re policing how parents store antibiotics like it’s a federal crime? Next you’ll be telling us to check the humidity levels in the nursery before giving Tylenol.
I live in New York. My apartment is 90 degrees in the summer. My kid’s medicine sits on the counter next to the toaster. And guess what? He got better. Every time. So maybe the CDC’s 15% statistic is just another stat that sounds scary but doesn’t mean squat in real life.
Also, why is it always the same people writing these posts? The ones who have a color-coded calendar for their kid’s nap schedule and a spreadsheet for vitamin intake? You’re not saving lives. You’re just making other parents feel guilty.
David Cunningham
Had a similar experience with azithromycin last year. We kept it in the fridge because we thought "cool = better." Kid gagged every time. We threw it out after three days. Got a new prescription. Kept it at room temp. He drank it like juice. No drama.
Also, the bit about not storing meds in the bathroom? 100% true. Mine was sitting above the sink. Got damp. Smelled weird. Tossed it. Didn’t even finish the course. Still got better. But now I know why.
Good post. Practical. No fluff. Just facts. I’m saving this for next time.
luke young
My kid took amoxicillin last week and I refrigerated it because I thought that’s what you’re supposed to do. He didn’t complain, so I figured it was fine. But now I’m wondering - did I make it taste worse than it needed to?
Also, I didn’t know about the 14-day rule. We had half left, so I kept it for "just in case." Now I’m embarrassed.
Thanks for the clarity. I’m setting a reminder on my phone for next time. And I’m going to ask the pharmacist every single time. No more guessing.
james lucas
Okay so I’ve been reading this whole thing and I’m just sitting here thinking - why is this even a thing? Why do we have to memorize storage rules for 12 different antibiotics like it’s a college exam? Why doesn’t the system just make it easy?
Like, imagine if every bottle had a QR code. Scan it, and your phone pops up: "This med: Refrigerate. Discard in 10 days. Do NOT shake if cloudy. Avoid heat above 25°C. Child may gag. Try chilling if too sweet. Do NOT reuse. Do NOT share. Do NOT keep past expiration. Here’s a video of how to pour it without spilling."
Instead, we get a tiny label in 8-point font and a pharmacist who says "it’s fine" because they’re on their 17th bottle of the hour.
Parents aren’t lazy. We’re overwhelmed. We need better systems, not more guilt. This post is great - but it shouldn’t be necessary. We shouldn’t have to Google this stuff at 2 a.m. when our kid’s fever won’t break.
Also, I wrote the discard date on the bottle with a Sharpie. And I set a reminder. And I’m still gonna panic when it’s day 13. Because we’re all just winging it.
Melvina Zelee
^^^ this. exactly this. i just sent this to my mom group and someone said "but my cousin’s kid took amoxicillin from last year and was fine." and i was like… yeah, but what if he wasn’t? what if that’s how resistant staph started in his school?
we’re not being paranoid. we’re being the generation that actually reads the label. and yeah, it’s exhausting. but it’s also the only way we can protect our kids when the system’s broken.
also, i just threw out a bottle of cefdinir that looked "fine" but had a weird metallic smell. i cried a little. but i’m not risking it.