Every year, thousands of infants end up in emergency rooms because someone gave them the wrong amount of medicine. Not because they meant to harm their child - but because they didn’t know how to measure it right. A drop isn’t always a drop. A milliliter isn’t always clear. And confusing infant and children’s concentrations can be deadly.
In 2022, nearly 12,000 infants under one year old were treated in U.S. emergency rooms for medication errors. Most of these weren’t accidents with pills or bottles left within reach. They were mistakes made while trying to give a simple dose of Tylenol or Motrin. The problem? Misunderstanding concentrations, using kitchen spoons, and trusting droppers that don’t measure accurately.
Why Infant Medication Is Different
Babies aren’t small adults. Their bodies process medicine differently. A dose that’s safe for a 2-year-old could be toxic for a 3-month-old. That’s why infant medications come in specific strengths - and why you can’t just guess.
Take acetaminophen. Before 2011, you could buy infant acetaminophen in two forms: one at 80 mg per mL (concentrated drops), and another at 160 mg per 5 mL (less concentrated). Parents mixed them up. One mom gave her 4-month-old the concentrated drops thinking it was the regular kind. The baby went into liver failure. That’s why the FDA stepped in. Today, all infant acetaminophen must be labeled 160 mg per 5 mL. The old 80 mg/mL drops are gone. But the confusion hasn’t fully disappeared.
Many parents still buy children’s acetaminophen - which is also 160 mg per 5 mL - and assume it’s the same. It is, chemically. But the packaging looks different. Labels say “for children 2-11 years.” That makes parents think it’s not for babies. So they reach for the old bottle in the cabinet - the one labeled “infant” - and accidentally use the wrong concentration.
Concentrations You Need to Know
Here’s what you need to remember:
- Infant acetaminophen: 160 mg per 5 mL (only form sold today)
- Children’s acetaminophen: 160 mg per 5 mL (same strength, different label)
- Infant ibuprofen: 50 mg per 1.25 mL (concentrated)
- Children’s ibuprofen: 100 mg per 5 mL (less concentrated)
Notice the difference? Infant ibuprofen is more than twice as strong as the children’s version. Giving a child’s dose to an infant might not help. Giving an infant dose to a toddler could overdose them.
Always check the label. Not the bottle. Not the box. The actual label on the medicine. Look for “mg per mL” or “mg per 5 mL.” If it says “160 mg/5 mL,” that’s the standard. If it says “80 mg/mL,” stop. That’s outdated. Call your pharmacist if you’re unsure.
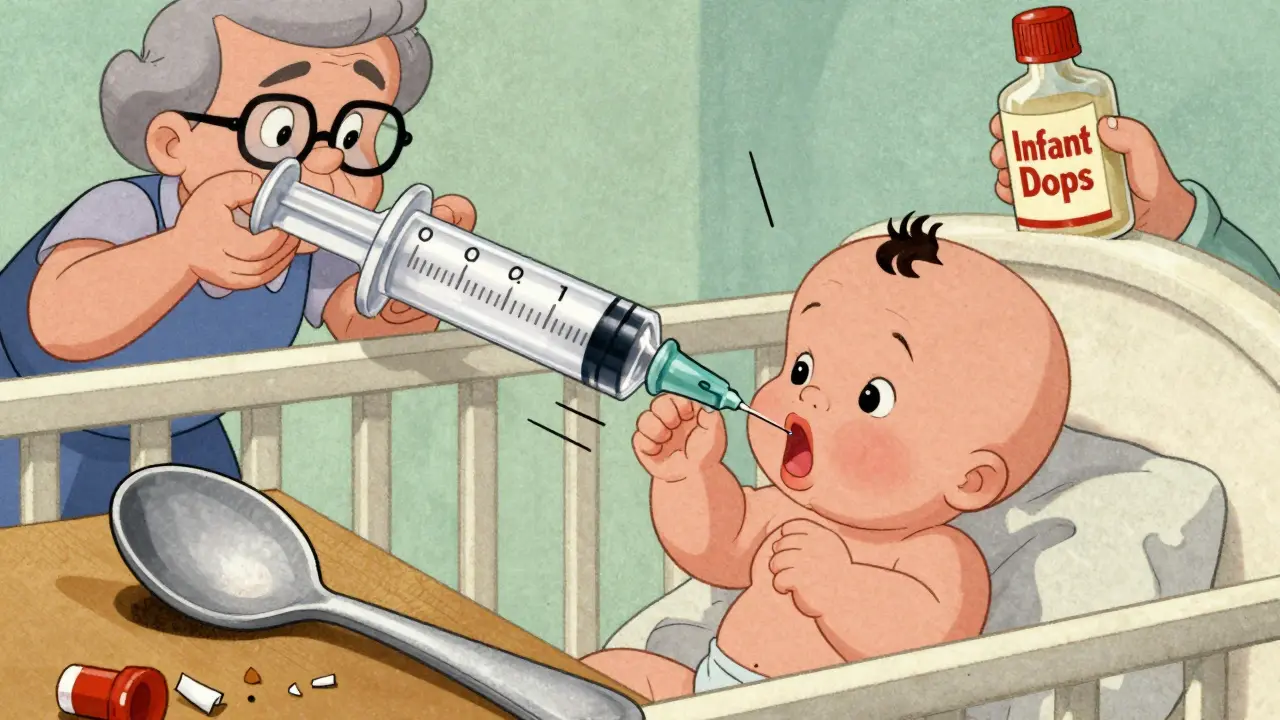
Measuring Devices: Why Your Spoon Is Dangerous
Kitchen teaspoons? They’re not accurate. A tablespoon from your kitchen might hold 10 mL. Or 15. Or 5. It depends on the spoon. A 2021 survey found that 43.6% of parents used spoons to measure infant medicine. Over half of those doses were off by more than 20%.
Medicine cups? They’re better, but still risky. The markings are often too big. A 0.5 mL dose? Hard to see. A 1 mL dose? Easy to misread.
The gold standard? An oral syringe with 0.1 mL markings. These are sold at pharmacies for under $2. They’re plastic, easy to clean, and precise. For babies under 6 months, use one with 0.1 mL graduations. For older infants, 0.2 mL is fine.
Here’s why it matters: A 2020 study at Cincinnati Children’s Hospital found that parents using oral syringes got the dose right 89% of the time. With medicine cups? Only 62%.
And never, ever use a dropper that comes with the medicine. Droppers vary in drop size. One brand’s “drop” might be 0.05 mL. Another’s might be 0.1 mL. That’s a 100% difference. You can’t trust them.
How to Calculate the Right Dose
Dosing isn’t based on age. It’s based on weight.
For acetaminophen: 10-15 mg per kilogram of body weight, every 4-6 hours. No more than 5 doses in 24 hours.
For ibuprofen: 5-10 mg per kilogram, every 6-8 hours. No more than 4 doses in 24 hours.
So if your baby weighs 8 kg (about 17.6 pounds), here’s the math:
- Acetaminophen: 8 kg × 10 mg = 80 mg minimum
- 8 kg × 15 mg = 120 mg maximum
Since the concentration is 160 mg per 5 mL, you divide:
- 80 mg ÷ 160 mg = 0.5
- 0.5 × 5 mL = 2.5 mL
So your dose is 2.5 mL. Not 3. Not 2. 2.5.
Use your oral syringe. Draw up 2.5 mL. Give it slowly into the side of the mouth. Don’t squirt it down the throat.
Write it down. Or take a picture of the calculation. Do this every time. Even if you’ve done it before. Babies grow fast. Their weight changes. Their dose changes.
Who’s Most at Risk?
Grandparents. That’s right. A 2023 study found caregivers over 65 made over three times as many dosing errors as parents under 30. Why? Outdated knowledge. Vision problems. Using old bottles labeled “infant” with 80 mg/mL concentrations that haven’t been sold in over a decade.
Also at risk? People giving medicine while tired. Or in a rush. Or when multiple caregivers are involved. One person gives 3 mL. Another thinks it was 2 mL and gives another 3. That’s 6 mL. That’s 192 mg. For a 5 kg baby? That’s over 38 mg/kg - more than double the safe max.
That’s why the CDC recommends a five-step check:
- Confirm your baby’s current weight in kilograms (not pounds).
- Calculate the dose using 10-15 mg/kg for acetaminophen.
- Check the concentration on the label (160 mg/5 mL).
- Use only an oral syringe with metric markings.
- Double-check with another adult before giving the dose.
Parents who follow all five steps reduce errors by 82%.

What to Avoid Completely
Don’t give cough and cold medicines to babies under 2. The FDA banned them in 2008. They don’t work. And they’ve caused seizures, fast heart rates, and deaths.
Don’t use multi-symptom products. If your baby has a fever and a runny nose, give acetaminophen for the fever. Use a saline spray and bulb syringe for the nose. Don’t reach for “cold + fever + cough” mixtures. They often contain antihistamines like diphenhydramine - which can cause breathing problems in infants.
Don’t store medicine in the fridge unless the label says to. Cold temperatures can change the concentration. And don’t mix medicine with formula or juice. If your baby doesn’t take it all, you won’t know how much they got.
What’s Changing Now?
The FDA is working on new rules. By 2026, infant medications may have color-coded labels: blue for babies, green for toddlers. Some new bottles will have QR codes. Scan them with your phone, and the app tells you the right dose based on weight.
The first “smart syringe” was approved in January 2023. It connects to your phone. You enter your baby’s weight. The app tells you how much to draw up. The syringe won’t let you go past the right amount. Clinical trials showed 98.7% accuracy.
But you don’t need to wait for tech to keep your baby safe. Right now, you can use a $2 oral syringe. You can write down the dose. You can call poison control at 1-800-222-1222 if you’re unsure.
The National Poison Control Center handled over 14,000 infant medication calls in 2022. They helped prevent ER visits in 99.2% of cases.
Final Checklist
Before you give any medicine to your infant:
- ✅ Confirm weight in kilograms
- ✅ Check the concentration on the label (160 mg/5 mL for acetaminophen)
- ✅ Use only an oral syringe (not a spoon, cup, or dropper)
- ✅ Draw up the exact amount - no guessing
- ✅ Double-check with another adult
- ✅ Never give cough/cold medicine to babies under 2
- ✅ Keep all medicine out of reach - even if it’s “just a drop”
Medicine is powerful. A few drops too much can be dangerous. But with the right tools and habits, you can give your baby what they need - safely.
Can I use a kitchen teaspoon to measure infant medicine?
No. Kitchen teaspoons vary in size and are not accurate. A teaspoon can hold anywhere from 4 to 7 mL, while the correct dose for infants is often less than 3 mL. Always use an oral syringe with metric markings for precision.
Is infant Tylenol different from children’s Tylenol?
No - the concentration is the same: 160 mg per 5 mL. The difference is in labeling and packaging. Infant Tylenol used to come in a more concentrated form (80 mg/mL), but that was removed in 2011. Today, both are identical. Always check the label, not the bottle name.
What should I do if I give my baby too much medicine?
Call Poison Control immediately at 1-800-222-1222. Do not wait for symptoms. Even small overdoses of acetaminophen or ibuprofen can cause liver or kidney damage. Keep the medicine bottle handy - they’ll need the concentration and amount given.
Why do some bottles say “infant” and others say “children’s” if the concentration is the same?
It’s marketing and packaging. The FDA required standardization of concentration, but not packaging. “Infant” labels are meant to signal it’s safe for babies under 2, while “children’s” is for older kids. But the medicine inside is identical. Always read the active ingredient and concentration - not the label color or word.
Can I give my baby ibuprofen before 6 months?
Ibuprofen is not recommended for babies under 6 months unless directed by a doctor. Acetaminophen is the preferred option for fever and pain in infants under 6 months. Always consult your pediatrician before giving ibuprofen to a baby under 6 months.
Are there any medications I should never give my infant?
Yes. Never give aspirin, cough and cold medicines, or products with diphenhydramine (like Benadryl) to infants under 2. These can cause serious side effects including seizures, breathing problems, and even death. Also avoid adult medications, even if they seem similar. Always use products labeled for infants.


Hilary Miller
Just used an oral syringe for the first time last week. Game changer. No more guessing.
Ryan Riesterer
The data from Cincinnati Children’s is solid. Oral syringes improve accuracy by 27 percentage points over cups. That’s not marginal-it’s clinically significant. Why are we still tolerating kitchen utensils as medical tools?
Philip House
Look, I get it. But let’s be real-most parents aren’t pharmacists. The fact that we need a $2 syringe and a math degree just to give Tylenol means the system’s broken. Why isn’t the FDA requiring smart packaging that auto-calculates dose? We’re stuck in 2011 while the world moved on.
And don’t even get me started on grandparents. My mom still has that old bottle labeled ‘infant drops’-80 mg/mL. She swears it’s ‘better.’ She’s 72. She can’t read the tiny print. This isn’t negligence-it’s design failure.
Oren Prettyman
While the article presents itself as a public service, it is, in fact, a thinly veiled endorsement of pharmaceutical standardization policies that have eroded consumer autonomy. The removal of the 80 mg/mL formulation was not a safety measure-it was a corporate consolidation tactic disguised as regulation. The same companies that produced the concentrated drops now monopolize the 160 mg/5 mL market. This is not progress. It is consolidation.
Furthermore, the insistence on oral syringes ignores cultural and socioeconomic realities. In many households, especially among immigrant families, the use of calibrated spoons is traditional and, when properly understood, reliable. To pathologize these practices as ‘dangerous’ is ethnocentric and dismissive of ancestral knowledge systems.
The CDC’s five-step checklist is not a solution-it is a bureaucratic overreach. It assumes parental incompetence and institutionalizes distrust. If we want to reduce errors, we should invest in community health educators-not syringes.
Moreover, the claim that 99.2% of poison control calls prevented ER visits is statistically dubious without a control group. Where is the peer-reviewed validation? Where is the long-term longitudinal data? The article reads like a press release from a pharmaceutical lobbying group.
And why is there no mention of the role of direct-to-consumer advertising in perpetuating confusion? Why is ‘infant’ and ‘children’s’ still differentiated in packaging if the concentration is identical? This is not safety. This is marketing.
I am not opposed to safety. I am opposed to performative safety that absolves institutions of responsibility while burdening parents with impossible standards.
Finally, the suggestion that parents ‘write down’ or ‘take a picture’ of their calculations implies that memory and cognitive load are not valid factors in medical decision-making. We are treating parents like lab technicians. This is dehumanizing.
Real safety is not in syringes. It is in accessible, non-judgmental, culturally competent care.
Brenda King
My sister-in-law gave her 4-month-old ibuprofen before 6 months because the label said 'for infants' and she didn't read the fine print. Thank god she called poison control. They talked her through it. No ER. No panic. Just calm, clear advice.
That’s why I tell every new mom I know: keep 1-800-222-1222 saved in your phone. Under ‘P’ for Poison Control. Not under ‘Dr.’ Not under ‘Pharmacy.’ Just ‘P.’
And if you’re scared you messed up? Call. Don’t wait. Don’t Google. Call.
Margaret Khaemba
I used to use the dropper that came with the medicine until my pediatrician showed me how inconsistent they are. Now I only use the oral syringe. It’s a $2 investment that saved me from a nightmare. I even bought one for my mom so she can help when she babysits.
Also, I write the dose on my hand with a Sharpie when I’m tired. It sounds silly, but I’ve done it twice now and it worked. Better than trusting my memory after a 3am feeding.
Alec Amiri
So let me get this straight-you’re telling me I can’t use a teaspoon but I can use a $2 plastic syringe? That’s it? That’s the big reveal? This whole article feels like someone got paid to write a PSA for a pharmacy chain.
And don’t even get me started on the ‘smart syringe’ that connects to your phone. Next thing you know, we’ll need an app, a subscription, and a biometric scan just to give a baby aspirin.
Meanwhile, real problems like formula shortages and pediatrician wait times go ignored. This is distraction medicine.
Malik Ronquillo
My cousin gave her baby 3 mL of infant ibuprofen thinking it was children’s. Baby ended up in the ICU. She didn’t even know the concentrations were different. That’s not ignorance. That’s a failure of the system. The labels should scream the difference. Not whisper it.
And why is it still legal to sell infant and children’s versions with different names? That’s not branding. That’s a trap.
Mike P
Everyone’s talking about syringes like they’re magic. But what about the people who can’t afford them? Or who live in rural areas where pharmacies are 40 miles away? You think a $2 syringe is accessible when you’re choosing between diapers and medicine?
This whole thing feels like a rich person’s solution to a poor person’s problem. We need free syringes at WIC offices. We need pharmacist-led home visits. We need education-not guilt trips.
And for the love of God, stop blaming grandparents. My grandma gave me Tylenol with a spoon when I was a baby. I’m 34 and I’ve never had liver damage. Maybe the system’s not broken. Maybe we’re just over-medicalizing parenting.
Akriti Jain
Did you know the FDA’s 2011 change was pushed by Johnson & Johnson? Coincidence? I think not. They owned the old concentrated drops. Now they own the new standard. Same product, new price tag. The real danger isn’t the dose-it’s the monopoly.
And those QR codes? They’re tracking your baby’s meds. Your phone’s listening. Your smart syringe’s uploading data. They’re building a pediatric health profile. You think that’s for safety? Nah. It’s for insurance premiums. Next thing you know, your baby’s ‘medication compliance score’ affects their future health insurance rates.
Wake up. This isn’t safety. It’s surveillance capitalism wrapped in baby blue.
Sarvesh CK
The ethical core of this issue lies not in the measurement tools, but in the epistemological dissonance between institutional medical authority and domestic caregiving practice. The medical establishment, in its pursuit of standardization, has pathologized the intuitive, context-sensitive knowledge that caregivers-particularly mothers and elders-have historically employed. The oral syringe is a technological fix for a cultural crisis.
What is lost in the transition from spoon to syringe is not merely accuracy, but trust: trust in the caregiver’s judgment, trust in intergenerational knowledge, trust in the body’s ability to adapt and respond. The insistence on metric precision, while scientifically sound, implicitly frames the parent as an incompetent operator rather than a loving, attentive agent.
Furthermore, the emphasis on individual responsibility-‘write it down,’ ‘double-check,’ ‘use a syringe’-obscures the structural failures: inadequate healthcare access, lack of pediatric pharmacy support, and the commodification of infant care as a consumer product.
Perhaps the true innovation lies not in a smart syringe, but in a reimagined model of care-one that integrates medical guidance with cultural humility, that honors the wisdom of grandmothers as much as the precision of pharmacists.
Medicine is not merely chemistry. It is relationship. And relationships cannot be calibrated with a 0.1 mL gradation.
Tatiana Bandurina
Let’s not pretend this is about safety. It’s about liability. Hospitals get sued when a baby gets too much acetaminophen. So they push parents to use syringes, write things down, and call poison control. That’s not care-that’s damage control. The real solution? Ban all non-prescription infant meds. Let doctors prescribe them. Then maybe we’d have real oversight.
Until then, this is performative safety. You feel better because you used a syringe. But the system didn’t change. It just moved the blame to you.
Daphne Mallari - Tolentino
The article, while well-intentioned, exhibits a troubling conflation of empirical precision with moral imperative. The valorization of the oral syringe as the sole legitimate instrument of dosage administration constitutes a form of technocratic authoritarianism, wherein the parent’s agency is subordinated to the dictates of metric orthodoxy. One is reminded of Foucault’s panopticon: the caregiver, perpetually observed, perpetually measured, perpetually inadequate.
Furthermore, the dismissal of cultural practices-such as the use of calibrated household utensils-reveals a profound ethnocentrism that privileges Western biomedical norms over global caregiving epistemologies. The infant in rural India, the infant in rural Appalachia, the infant in immigrant households: their caregivers are not deficient. They are differently informed.
The call for QR codes and smart syringes is not innovation. It is the commodification of infant care under the banner of ‘safety.’ The pharmaceutical-industrial complex thrives on anxiety. Do not mistake their marketing for medicine.
Kenji Gaerlan
my 2yr old got sick and i used a kitchen spoon cause i was tired and didnt have a syringe. she lived. also my mom did it to me and i turned out fine. maybe we dont need all this tech?
Keith Helm
Per FDA guidelines, the standardization of acetaminophen concentration to 160 mg/5 mL was enacted under 21 CFR 201.107(c) to mitigate dosing errors. The continued use of outdated formulations constitutes a violation of product labeling regulations. Oral syringes are not optional. They are the recognized standard of care per AAP and CDC. Compliance is non-negotiable.
Malik Ronquillo
Wait, so if I give my baby 2.5 mL and then my wife gives another 2.5 mL because she didn’t know I already did it… that’s 5 mL? That’s 160 mg? For a 5kg baby? That’s over 30 mg/kg? That’s lethal.
That’s why I have a whiteboard in the nursery. I write ‘DOSING DONE’ after every time. And I take a picture. And I tell my wife: ‘I did it.’ No guessing. No assumptions.