Hypernatremia: Causes, Risks, and What You Need to Know
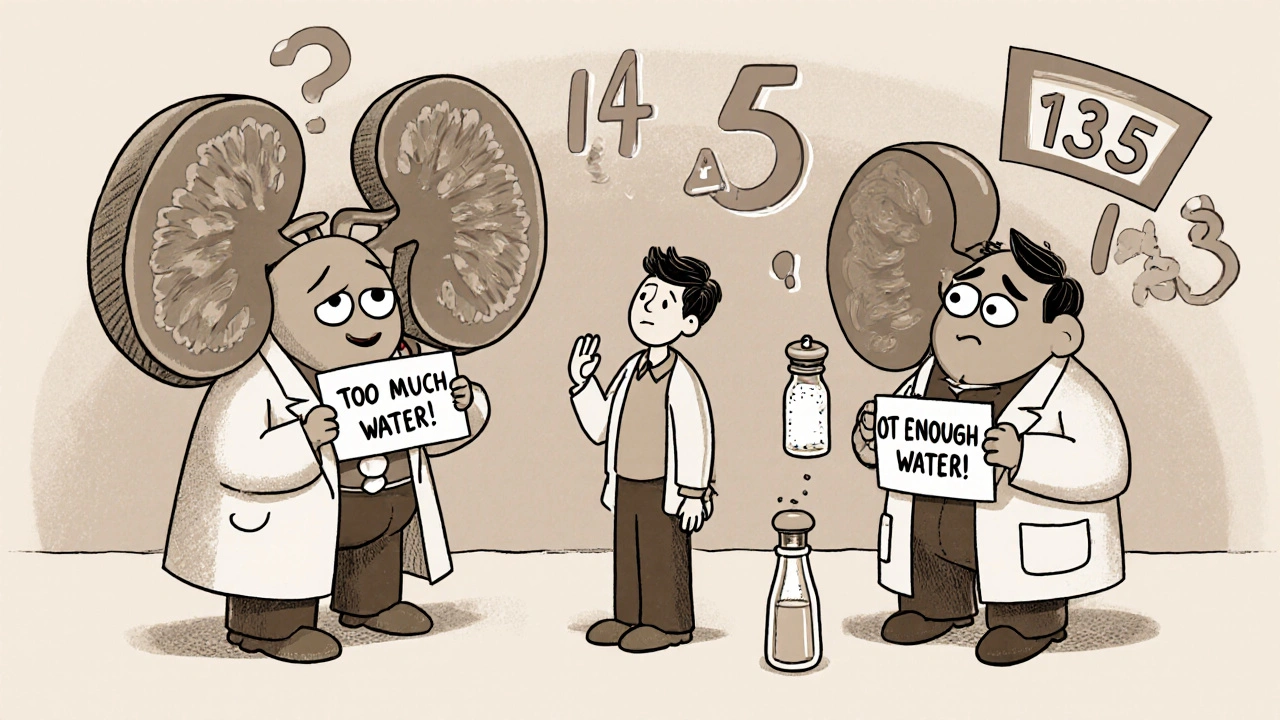
When your blood sodium levels rise too high, you’re dealing with hypernatremia, a condition where the concentration of sodium in the blood exceeds normal levels, typically above 145 mEq/L. It’s not just a lab number—it’s a sign your body is struggling to balance fluids, often because you’re not drinking enough or losing too much water. This isn’t rare. It’s one of the most common electrolyte problems in hospitals, especially among older adults, people with dementia, or those who can’t get to water on their own.
dehydration, the loss of body water that leads to concentrated sodium in the bloodstream is the main driver of hypernatremia. But it’s not always from skipping water. Think fever, vomiting, diarrhea, or even certain meds like diuretics. Even sweating hard without replacing fluids can push sodium up. And electrolyte disorders, imbalances in minerals like sodium, potassium, and chloride that affect nerve and muscle function don’t always show up as obvious symptoms until it’s too late. Confusion, muscle twitching, or extreme thirst? Those are red flags. But sometimes, people just seem "off"—lethargic, irritable, or unresponsive—and that’s when hypernatremia slips through.
What makes this tricky is that many people don’t realize how fast sodium can climb. A person with limited mobility might not feel thirsty, or someone on multiple medications might not connect their dry mouth to a dangerous spike in sodium. Even kids and athletes can develop it if they’re losing fluids and only replacing them with plain water, diluting other electrolytes and triggering a rebound effect. And if left unchecked, hypernatremia can lead to seizures, brain damage, or worse.
You won’t find hypernatremia in every post below, but you’ll see its cousins: how medications like diuretics affect fluid balance, how aging changes your body’s thirst signal, how kidney function ties into sodium control, and why safe medication disposal matters if you’re on long-term treatments that alter your electrolytes. These aren’t random articles—they’re pieces of the same puzzle. If you’re managing a chronic condition, caring for an elderly relative, or just trying to understand why your body feels off, this collection gives you the real-world context you need—not just the textbook definition.
Hyponatremia and Hypernatremia in Kidney Disease: What You Need to Know
Hyponatremia and hypernatremia are common, dangerous complications in kidney disease. Learn how fluid balance, diet, and medications affect sodium levels-and what you can do to stay safe.