Respiratory Depression: Causes, Risks, and What You Need to Know
When your breathing slows down too much, it’s called respiratory depression, a condition where breathing becomes dangerously slow or shallow, reducing oxygen intake and increasing carbon dioxide levels in the blood. Also known as hypoventilation, it’s not just a side effect—it can be life-threatening if not caught early. This isn’t something that happens out of nowhere. It’s often tied to drugs that calm the nervous system, like opioids, benzodiazepines, or alcohol. Even sleep aids and muscle relaxants can trigger it, especially when mixed. The brain’s breathing center gets suppressed, and suddenly, each breath becomes too weak to keep you alive.
People on long-term pain meds, especially after surgery or for chronic conditions, are at higher risk. But it’s not just about prescription drugs. Mixing opioids with alcohol or anti-anxiety meds like Xanax can turn a routine dose into a medical emergency. Older adults, people with sleep apnea, or those with lung diseases like COPD are more vulnerable too. You don’t need to be a drug user to be at risk—sometimes, just taking a higher-than-recommended dose of a common pill is enough. And here’s the scary part: many don’t realize it’s happening until it’s too late. There’s no burning pain or obvious scream. It’s quiet. Slow. Silent.
That’s why knowing the signs matters. Slowed breathing—less than 10 breaths per minute—is the biggest red flag. Bluish lips or fingertips, extreme drowsiness, confusion, or being hard to wake up are all warning signs. If someone’s on opioids and starts nodding off more than usual, or their breathing sounds like shallow whispers, don’t wait. Call for help. Naloxone can reverse opioid-induced respiratory depression, but only if used fast. For non-opioid causes, stopping the drug and getting oxygen fast is key.
What you’ll find in the articles below are real, practical guides on medications that can cause this, how to spot trouble early, and what alternatives exist for managing pain or sleep without putting your breathing at risk. From comparing inhalers for asthma to understanding how sedatives interact with other drugs, these posts give you the tools to make smarter choices. No fluff. No jargon. Just clear info to help you or someone you care about stay safe.
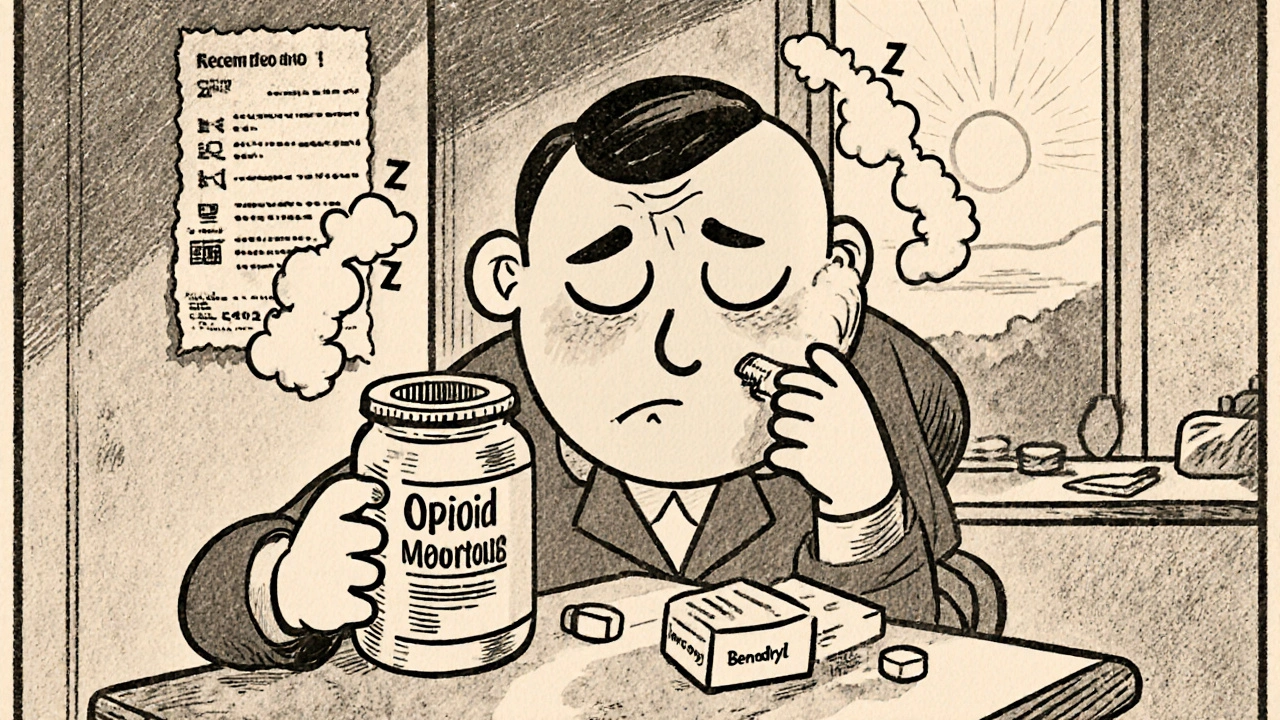
Opioids + Antihistamines: How Excess Sedation Sparks Respiratory Danger
Learn why mixing opioids with first‑generation antihistamines can cause extreme sedation and dangerous breathing slowdown, and how to prevent it.