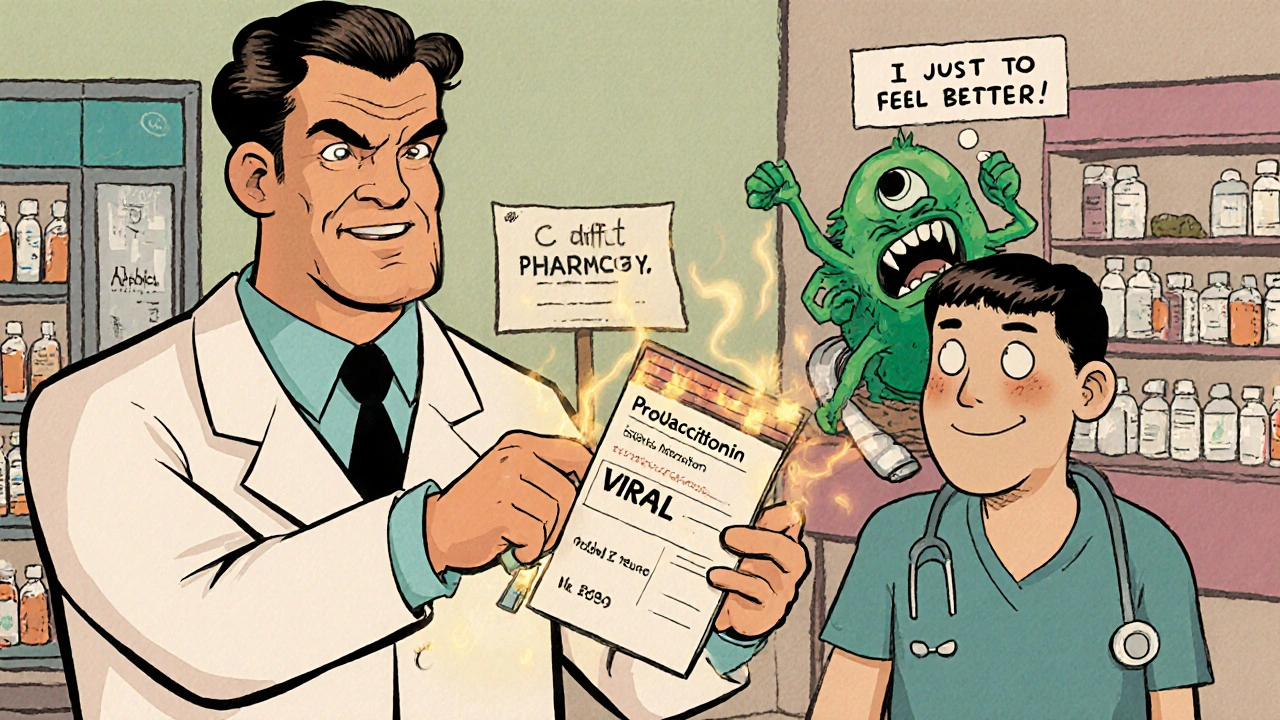
Every year in the U.S., antibiotic stewardship saves thousands from avoidable harm-not because it stops antibiotics, but because it makes sure they’re used only when needed, and used correctly. Too often, antibiotics are prescribed for viral infections like colds or flu, or given too long, too strong, or too broadly. The result? Not just antibiotic resistance, but real, dangerous side effects that can land patients back in the hospital-or worse.
What Antibiotic Stewardship Actually Means
Antibiotic stewardship isn’t a buzzword. It’s a set of proven practices designed to make sure the right antibiotic is given at the right dose, for the right bug, and for the right length of time. The CDC calls it the backbone of patient safety in modern medicine. It’s not about being cautious-it’s about being precise. Think of it like this: antibiotics are powerful tools, but they’re not magic bullets. When you use them unnecessarily, you’re not just treating one person-you’re putting everyone at risk. The gut microbiome, which keeps your immune system balanced, gets wiped out. Harmful bacteria like Clostridioides difficile (C. diff) take over, causing severe diarrhea, colitis, and sometimes death. In fact, inappropriate antibiotic use increases the risk of C. diff by 7 to 10 times. Stewardship programs work by asking four key questions before prescribing:- Do we even need antibiotics?
- Which one is best for this infection?
- What’s the right dose and route?
- How long should the patient take it?
How Inappropriate Use Leads to Side Effects
Most people think antibiotics only kill bad bacteria. But they don’t discriminate. They wipe out the good bacteria in your gut, mouth, and skin too. That disruption is what leads to the most common side effects:- C. diff infection: Causes severe, recurring diarrhea. In hospitals, it’s one of the top causes of preventable harm.
- Antibiotic-associated diarrhea: Not always life-threatening, but enough to make patients miss work, cancel plans, and lose trust in their care.
- Allergic reactions: Rashes, swelling, anaphylaxis-some of these are deadly and often linked to overuse of penicillin or sulfa drugs.
- Secondary infections: Yeast infections, urinary tract infections, and even fungal infections can flare up after antibiotics disrupt natural defenses.
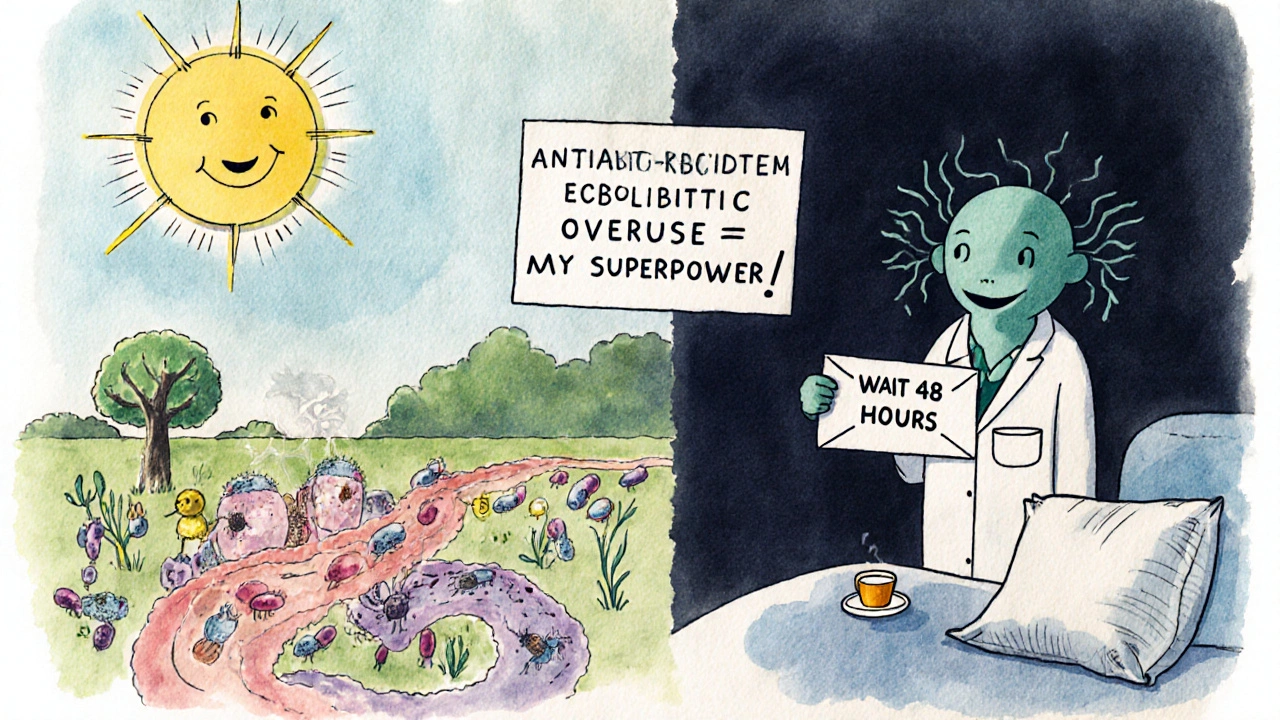
How Stewardship Programs Cut Side Effects
Hospitals with strong stewardship programs don’t just reduce resistance-they reduce hospital stays, readmissions, and deaths. Here’s how they do it:- Prospective audit and feedback: Pharmacists review every antibiotic order and talk to doctors if it looks wrong. In one Nebraska hospital, this cut C. diff rates by 32% in two years.
- Shorter courses: Many infections-like pneumonia or urinary tract infections-can be treated in 5 to 7 days, not 10 to 14. Studies show reducing duration by just 1.6 to 3.5 days doesn’t hurt outcomes, but cuts side effects dramatically.
- Biomarker testing: Tests like procalcitonin help doctors tell if an infection is bacterial (needs antibiotics) or viral (doesn’t). In one study, using this test reduced antibiotic use by 2.1 days for pneumonia patients.
- Formulary restrictions: Limiting access to broad-spectrum antibiotics like vancomycin or carbapenems means they’re only used when absolutely necessary, reducing collateral damage to the microbiome.
Why Outpatient Settings Are Still a Problem
While hospitals have made big progress-88% of U.S. hospitals with over 200 beds now have formal stewardship programs-outpatient care is lagging. Emergency rooms and doctor’s offices still prescribe antibiotics for sore throats, ear infections, and bronchitis, even when tests show they’re viral. Why? Time pressure. Patient expectations. Fear of being sued. Doctors often feel they have to prescribe something, even if they know it won’t help. But stewardship isn’t about saying no-it’s about saying right now. New tools are helping:- Electronic alerts in EHRs that pop up when a doctor tries to prescribe an antibiotic for a viral illness.
- Delayed prescriptions: Giving patients a script to fill only if symptoms worsen after 48 hours.
- Public education: Posters in waiting rooms, handouts explaining why antibiotics don’t work for colds.
What It Takes to Run a Successful Program
A good stewardship program doesn’t happen by accident. It needs:- Leadership commitment: Hospital administrators must fund it and make it a priority.
- Dedicated experts: At least one infectious disease physician (0.5 FTE) and one clinical pharmacist (1.0 FTE) are required by CDC guidelines.
- Tracking systems: Monitoring which antibiotics are used, how long they’re given, and what side effects follow.
- Education: Regular training for doctors, nurses, and pharmacists. The Society of Infectious Diseases Pharmacists recommends 40 hours of specialized training.
The Bigger Picture: Why This Matters Beyond Side Effects
Antibiotic stewardship isn’t just about protecting individual patients. It’s about preserving medicine itself. Every time we misuse an antibiotic, we help superbugs evolve. The World Health Organization warns that by 2050, antimicrobial resistance could cause 10 million deaths a year globally. That’s more than cancer. And it’s not some distant threat-it’s happening now. In the U.S. alone, 35,000 people die each year from antibiotic-resistant infections. Stewardship is one of the three pillars the WHO says we need to survive this crisis: infection prevention, patient safety, and appropriate antibiotic use. Without it, we risk returning to a time when a simple cut or childbirth could be deadly.What Patients Can Do
You don’t need to be a doctor to help. Here’s how you can protect yourself:- Ask: “Do I really need antibiotics?” If your doctor says yes, ask why.
- Ask: “Is there a test to confirm this is bacterial?”
- Never take leftover antibiotics from a previous illness.
- Don’t pressure your doctor for antibiotics if you have a cold or flu.
- Finish the full course if antibiotics are prescribed-unless your doctor says otherwise.
What’s Next for Antibiotic Stewardship
The future is getting smarter. AI tools are being tested to analyze patient data in real time and suggest the best antibiotic options. Rapid molecular tests can now identify pathogens and resistance genes in hours, not days. Some hospitals are using machine learning to predict which patients are most likely to develop C. diff after antibiotic exposure. But technology alone won’t fix this. Culture change will. Doctors need to feel supported when they choose not to prescribe. Patients need to understand that not treating is sometimes the best treatment. The goal isn’t to eliminate antibiotics. It’s to use them like a scalpel-not a sledgehammer.Can antibiotics cause long-term gut damage?
Yes. Repeated or unnecessary antibiotic use can alter the gut microbiome for months or even years. Studies show that some people never fully recover their original bacterial diversity, which may increase the risk of obesity, autoimmune diseases, and chronic inflammation. Stewardship helps by minimizing exposure to these drugs in the first place.
Are there alternatives to antibiotics for minor infections?
For many common infections like colds, flu, sinusitis, and bronchitis, antibiotics aren’t just unnecessary-they’re harmful. Supportive care like rest, fluids, pain relievers, and saline nasal sprays works better and safer. For ear infections in children, watchful waiting is often recommended before prescribing.
Why do doctors still overprescribe antibiotics?
Pressure from patients, time constraints, diagnostic uncertainty, and fear of missing a bacterial infection all play a role. Some doctors worry that not prescribing will lead to complaints or lawsuits. Stewardship programs help by giving providers evidence-based tools, feedback, and support to make confident, safe decisions.
Is antibiotic stewardship only for hospitals?
No. While hospitals have made the most progress, outpatient settings are where most inappropriate prescribing happens. The CDC now prioritizes stewardship in doctor’s offices, urgent care centers, and pharmacies. Tools like electronic alerts, delayed prescriptions, and patient education are making a difference in these settings too.
How can I tell if I’m getting an unnecessary antibiotic?
If you have a runny nose, sore throat without fever or pus, cough without wheezing, or green mucus alone, you likely don’t need antibiotics. Ask your provider if they’ve ruled out viral causes. If they say “it’s probably bacterial,” ask for evidence-like a rapid strep test or procalcitonin level. Don’t accept a prescription without a clear reason.






Phil Thornton
Antibiotics aren't magic. They're more like a chainsaw when you need a scalpel. I've seen people get C. diff after a simple sinus infection prescription. It's wild how much damage a 10-day course can do.
Pranab Daulagupu
From a clinical microbiology standpoint, the microbiome disruption cascade post-antibiotic exposure is non-trivial. The dysbiosis-induced immune modulation can predispose to metabolic and autoimmune sequelae. Stewardship isn't optional-it's foundational.
Barbara McClelland
Love this breakdown. I'm a nurse and I've watched families panic when their kid gets a 14-day amoxicillin course for an ear infection that could've waited. Teaching patients that 'watchful waiting' isn't neglect-it's wisdom-is huge.
Alexander Levin
Big Pharma doesn't want you to know this. Antibiotics are a cash cow. They push doctors to prescribe, then sell you probiotics to fix the damage they caused. Wake up.
Ady Young
My dad was hospitalized twice because of C. diff after a simple UTI antibiotic course. We didn't know any better. This post changed how I talk to my doctor now. Asking 'Do I really need this?' feels empowering, not rude.
Travis Freeman
As someone who grew up in a village where antibiotics were rationed, it's wild to see how freely they're handed out here. We used honey for coughs and rest for colds. Maybe we were onto something.
Sean Slevin
...and yet... we still don't know the full extent of microbiome recovery... or if it's even possible... to return to baseline... after repeated exposure... and what if... the real issue isn't just overuse... but the lack of microbial diversity in modern environments...?
...I mean... think about it... we sanitize everything... then we give antibiotics... then we wonder why allergies are through the roof...
It's not a coincidence... it's a perfect storm... of modern medicine... and modern life...
Chris Taylor
My sister took antibiotics for a sore throat and ended up with a yeast infection so bad she couldn't sit down for a week. I never realized how much collateral damage these things cause. Thanks for the eye-opener.
Melissa Michaels
It is imperative to recognize that antibiotic stewardship protocols have demonstrated statistically significant reductions in adverse drug events across multiple peer-reviewed studies. The data is unequivocal. Implementation in outpatient settings remains a critical public health priority.
Nathan Brown
It's funny how we treat antibiotics like they're candy. We don't do this with chemo or radiation. Why? Because we don't understand how delicate the microbiome is. We're not just killing bacteria-we're erasing a part of our own biology that evolved with us over millions of years.
Matthew Stanford
I work in a community clinic. We started using delayed prescriptions for bronchitis last year. Patient complaints dropped. No one filled the script unless they got worse. It’s a small change that makes a big difference.
Olivia Currie
OH MY GOSH. I JUST HAD TO GO TO THE ER BECAUSE OF C. DIFF AFTER A SIMPLE TOOTH EXTRACTION ANTIBIOTIC. I WASN'T EVEN SICK. I JUST NEEDED A TOOTH OUT. THIS IS A SCANDAL. I'M TELLING EVERYONE.
Curtis Ryan
Man I just found out my kid's ear infection didn't need antibiotics and now I feel like a bad parent. But honestly? He's fine. No fever. Playing. We just gave him ibuprofen. Why do we panic so much?
Nathan Brown
You're not a bad parent. You're a good one who listened. That's the whole point. Medicine isn't about doing something-it's about doing the right thing. And sometimes, the right thing is doing nothing.