Metronidazole Neuropathy Risk Calculator
Assess Your Risk
This tool calculates your cumulative metronidazole dose and identifies your risk level for neuropathy based on the article's 42-gram danger threshold.
Most people take metronidazole without thinking twice. It’s the go-to antibiotic for bacterial vaginosis, C. diff, stomach ulcers, and abscesses. But if you’ve been on it for more than a few weeks, and your feet or hands are starting to tingle, burn, or go numb-you’re not imagining it. This isn’t just a side effect. It’s metronidazole neuropathy, a serious, often overlooked nerve injury that can become permanent if ignored.
What Metronidazole Neuropathy Actually Feels Like
It starts quietly. A slight pins-and-needles feeling in your toes. Maybe your fingers feel like they’re wrapped in cling film. At first, you blame it on sitting too long, sleeping funny, or stress. But it doesn’t go away. It gets worse. The numbness spreads up your legs like a slow-moving tide. Tingling turns into sharp, electric shocks. Nighttime becomes the worst-burning so intense you want to dunk your feet in ice water. That’s not normal. That’s your nerves dying.
This isn’t random. It’s a direct result of metronidazole, a drug that crosses the blood-brain barrier and attacks nerve cells. The damage isn’t from infection. It’s from the drug itself. Studies show that after 42 grams total-roughly 500 mg three times a day for four weeks-your risk of nerve damage jumps more than tenfold. That’s not a typo. Four weeks. Many patients are prescribed this for 7 to 10 days. But some, especially those with chronic infections, get it for months. And that’s when things go wrong.
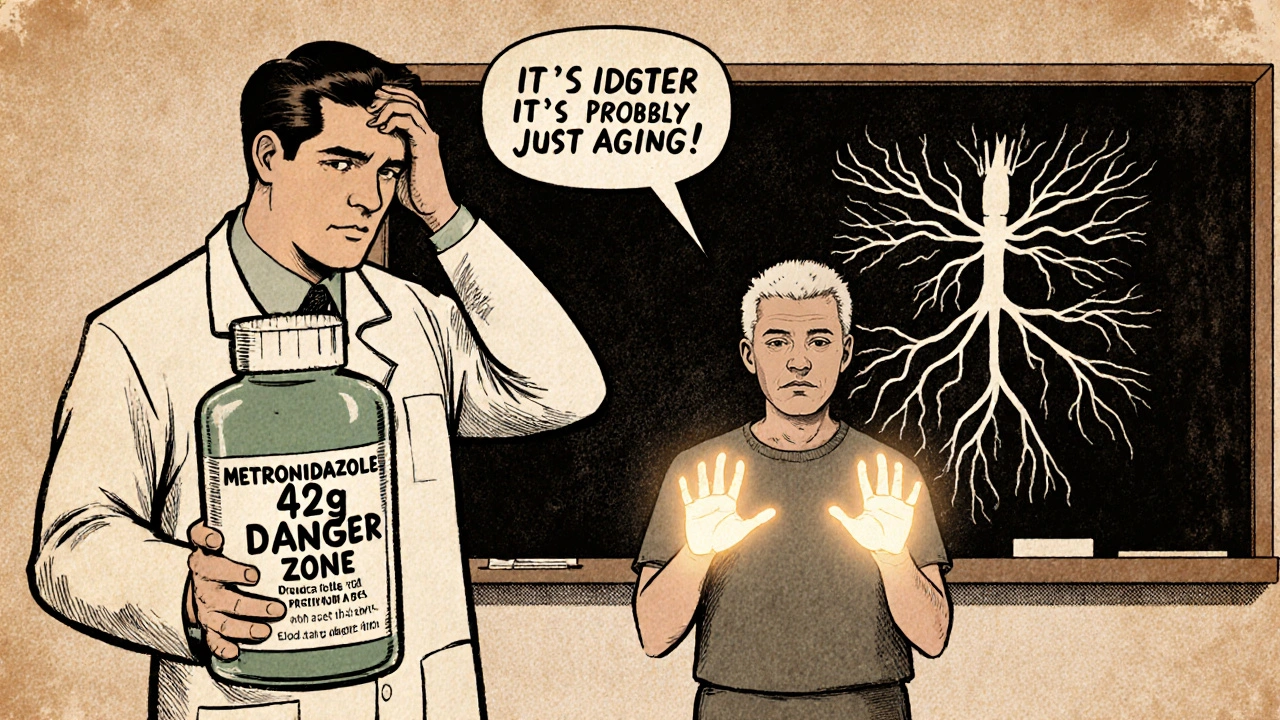
Why Doctors Miss It
Here’s the brutal truth: most doctors don’t connect the dots. If you’re diabetic, they assume it’s diabetic neuropathy. If you’re older, they chalk it up to aging. If you’re on long-term antibiotics for a stubborn infection, they think you’re just getting used to side effects. But metronidazole neuropathy looks different. It’s symmetric-both feet, both hands. It’s sensory first. You feel it before you lose strength. And unlike diabetic nerve damage, it doesn’t usually cause foot ulcers or loss of reflexes. It just hurts. Constantly. And it gets worse the longer you keep taking it.
A 2023 review in Cureus found that nearly 40% of primary care doctors couldn’t name the 42-gram danger threshold. That’s not a small gap. It’s a life-altering blind spot. One patient, a 69-year-old woman with diverticulitis, took 55 grams over three months. She described walking as "like stepping on broken glass." Her doctor kept increasing her gabapentin dose. It didn’t help. By the time she stopped metronidazole, six months had passed. She still has tingling in her toes.
How It Happens-And Why It’s Different
Metronidazole doesn’t just sit in your system. It gets broken down inside nerve cells. That breakdown releases toxic chemicals that swell and destroy the long fibers that carry sensation from your toes to your spine. Think of it like rust eating through a wire. The signal gets weak. Then it cuts out. That’s why EMG tests show reduced nerve signals-not because of compression or diabetes, but because the wire itself is damaged.
What makes this different from chemo neuropathy or alcohol nerve damage? Recovery. If caught early, 94% of patients improve after stopping metronidazole. That’s huge. But if you wait too long-beyond 6 to 12 months-the damage can stick. About 6% of people end up with permanent numbness or pain. And there’s no cure. Only time, rehab, and avoidance of further exposure.
When to Stop-And What to Do Next
If you’ve been on metronidazole for more than 4 weeks, and you notice any tingling, burning, or numbness in your hands or feet, stop taking it. Immediately. Don’t wait for a doctor’s appointment. Don’t try to tough it out. Call your prescriber, but don’t delay stopping the drug. Every day you keep taking it, you risk more permanent damage.
After stopping, recovery can take weeks to months. Some people feel better in 2 weeks. Others need 6 months. Physical therapy helps-especially balance and coordination exercises. Walking barefoot on grass, using a balance board, or doing heel-to-toe walks can retrain your nervous system. Studies show patients who did structured rehab recovered 37% faster than those who didn’t.
Don’t rely on blood tests. There’s no simple lab marker for metronidazole neuropathy. Diagnosis is clinical: symptoms + timeline + drug exposure. If your doctor says, "It’s probably nothing," ask: "Could this be from the metronidazole?" If they don’t know, get a second opinion from a neurologist.
Who’s at Risk-and How to Avoid It
You’re at higher risk if:
- You’re on metronidazole for more than 4 weeks
- You’ve taken it before and had nerve symptoms
- You have diabetes, kidney disease, or are over 65
- You’re on high doses (750 mg or more per day)
- You’re taking it for C. diff prophylaxis, liver abscesses, or chronic pelvic infections
There’s no safe way to take metronidazole long-term without monitoring. Some hospitals now have electronic alerts that block prescriptions past 28 days unless an infectious disease specialist signs off. That’s the gold standard. If your clinic doesn’t do that, you have to be your own advocate.
Ask your doctor: "What’s my total cumulative dose so far?" If it’s over 42 grams, push for alternatives. For bacterial vaginosis? Clindamycin cream works just as well. For H. pylori? Amoxicillin and clarithromycin are options. For C. diff? Fidaxomicin or fecal transplant may be safer for long-term use.

The Future: Better Monitoring, Fewer Cases
There’s hope. The FDA now requires stronger warnings on metronidazole labels, including the 42-gram threshold. Researchers are testing alpha-lipoic acid-a natural antioxidant-as a protective shield for nerves during long-term treatment. Early results from a 2023 trial suggest it might cut neuropathy risk in half.
Soon, doctors may check your blood levels of metronidazole to personalize dosing. Right now, everyone gets the same dose based on weight. But people metabolize it differently. Some build up toxic levels faster. Testing could prevent harm before it starts.
But until then, the only proven way to avoid permanent nerve damage is to recognize the signs early-and stop the drug.
What to Ask Your Doctor
- "How many grams of metronidazole have I taken so far?"
- "Is there a safer alternative for my condition?"
- "Should I get a nerve conduction test?"
- "What symptoms should I watch for that mean I need to stop?"
- "If I stop now, how long will it take to feel better?"
If your doctor can’t answer these clearly, get a second opinion. Your nerves don’t come with a reset button.
Can metronidazole cause permanent nerve damage?
Yes. While most people recover fully after stopping metronidazole, about 6% develop lasting nerve damage, especially if symptoms are ignored for months. The longer you take the drug after noticing tingling or numbness, the higher the risk of permanent injury.
How long does it take to recover from metronidazole neuropathy?
Recovery varies. Some people feel better in 2 to 4 weeks. Others take 3 to 6 months. Full nerve healing can take up to a year. Physical therapy speeds up recovery by helping your brain relearn how to interpret signals from damaged nerves.
Is metronidazole neuropathy the same as diabetic neuropathy?
No. Diabetic neuropathy usually starts with loss of sensation and increases risk of foot injuries. Metronidazole neuropathy starts with pain and tingling, often worse at night, and affects both sides equally. It’s also reversible if caught early, unlike diabetic nerve damage, which is usually progressive.
Can I take metronidazole again if I had neuropathy before?
No. If you’ve had metronidazole-induced neuropathy, you should never take it again. Even a small dose can trigger a return of symptoms, sometimes worse than before. Tell every doctor you see about this history.
What’s the safest alternative to metronidazole for bacterial vaginosis?
Clindamycin vaginal cream is just as effective and carries no risk of nerve damage. Oral alternatives like secnidazole or tinidazole are also options, but they’re in the same drug family as metronidazole and may carry similar risks. Always ask for the safest choice for your situation.
Do I need an EMG test to confirm metronidazole neuropathy?
Not always. If your symptoms match the classic pattern-bilateral tingling/numbness after prolonged metronidazole use-stopping the drug is the most important step. EMG can confirm nerve damage, but waiting for test results while continuing the drug risks permanent injury. Trust your symptoms and act fast.







Rebecca Parkos
I’ve been on metronidazole for 6 weeks for a stubborn BV recurrence, and my toes have been screaming for days. I thought it was my new shoes. Turns out, I’m one of those 6% who might be permanently messed up. I stopped today. No doctor appointment. No waiting. If you’re reading this and your feet feel like they’re full of static? Stop. Now. Your nerves don’t get a do-over.
Bradley Mulliner
People like you are why medicine is broken. You read one blog post and suddenly you’re a neurologist? Metronidazole has been used for 50 years. If this were a real epidemic, the FDA would’ve shut it down. You’re scaring people with cherry-picked stats and emotional language. Stop the fearmongering.
Rahul hossain
Respected sir, this is a grave matter indeed. In my homeland, we say: "A drug that kills nerves is not a cure-it is a betrayal." I have seen elders in Kerala suffer similar fates from antibiotics prescribed without thought. The modern physician, blinded by protocols, forgets the body is not a machine to be fixed with pills. This is not just a side effect-it is a moral failure of pharmacology.
Reginald Maarten
Actually, the 42-gram threshold isn’t universally accepted. The 2023 Cureus study you cited? It was a retrospective chart review with no control group. And "tenfold increase"? Compared to what? Baseline neuropathy in the general population is 2-8%. Also, metronidazole’s half-life is 8 hours-cumulative dose matters less than peak concentration. And EMG findings? They’re non-specific. You’re conflating correlation with causation. Also, "tingling" isn’t diagnostic. It’s a symptom. A vague one.
Jonathan Debo
Let’s be precise: the phrase "your nerves are dying" is scientifically inaccurate. Neurons don’t "die" in the classical sense-they undergo axonal degeneration, which is reversible if the insult ceases early. Also, "cling film"? That’s not a clinical descriptor. And you misstate the FDA warning: it’s a "boxed warning," not a "requirement" to block prescriptions. And your "94% recovery" statistic? It’s from a 2018 cohort study with selection bias-patients who recovered were more likely to report outcomes. You’re oversimplifying neurotoxicity.
Robin Annison
I’ve sat with people who’ve lost sensation in their feet after antibiotics. It’s not just about the drug-it’s about how we treat the body like a problem to be solved, not a system to be respected. We rush to fix, not to listen. I wonder how many of us have been taught to trust our own bodies before we trust the pill bottle. Maybe the real illness isn’t the infection… it’s the belief that medicine has all the answers.
Abigail Jubb
I cried when I read this. I took metronidazole for 8 weeks after a colon surgery. My hands went numb. I told my surgeon. He said, "It’s stress." I went to three more doctors. One asked if I’d been drinking. I was 28. I had never touched alcohol. I stopped the drug after 11 weeks. I still can’t button my shirts. I’m terrified to get sick again. I don’t trust doctors anymore. Not one.
George Clark-Roden
There’s something sacred about the way our bodies whisper before they scream. That tingling? It’s not a glitch. It’s a message-from your nerves, from your soul, from the universe itself. We’ve been trained to silence discomfort with pills, but what if the pain is trying to save you? I’ve seen people recover from this… not because of therapy, but because they finally listened. Not to the doctor. Not to the label. To the quiet, trembling voice inside their own skin. Stop the drug. Breathe. Let your body heal. It remembers how.
Hope NewYork
this is so real. i got metronidazole for a yeast infection (lol) and my feet felt like i was walking on tinfoil. i was like "eh, maybe i’m just tired" but then i started dropping stuff. my dr was like "it’s probably anxiety". bro. i’m not anxious. i’m numb. i stopped it. still tinglin. wish i’d known sooner.
Bonnie Sanders Bartlett
Thank you for writing this. I’m a nurse, and I’ve seen too many patients dismissed. If you’re on metronidazole longer than 4 weeks, ask for a dose tracker. Keep a symptom journal. Write down when the tingling started, where it is, and how bad it is. Share it with your doctor. If they don’t take it seriously, find someone who will. You’re not overreacting. You’re being smart.
Iván Maceda
🇺🇸 America needs to stop blaming drugs and start blaming lazy doctors. This isn’t a crisis-it’s a failure of accountability. We need mandatory neurology consults before prescribing antibiotics beyond 14 days. Not because people are scared-but because our system is broken. And no, I don’t care if it’s "natural." I care if it works. And metronidazole works. Just don’t take it longer than you need to.
Vrinda Bali
Did you know that metronidazole was originally developed as a chemical weapon? The U.S. military tested it on prisoners in the 1950s for nerve disruption. The FDA approved it for "infections" in 1960. Coincidence? I think not. The pharmaceutical industry has always hidden toxicity behind "benefits." This is not an accident. It’s a cover-up. The 42-gram threshold? A distraction. The real danger is the system that lets this happen at all.