When you fill a prescription for a common drug like metformin or lisinopril, you probably don’t think twice about getting the generic version. It’s cheaper, just as effective, and your pharmacist can swap it in without asking your doctor. But what if your medicine isn’t a little pill-it’s an injection you get every few weeks for rheumatoid arthritis, cancer, or Crohn’s disease? That’s where biosimilars come in. They’re the closest thing to generics for complex biologic drugs, and they’re changing how patients access life-saving treatments.
What Exactly Are Biosimilars?
Biosimilars aren’t exact copies of brand-name biologics. That’s because biologics aren’t made like regular pills. They’re created using living cells-yeast, bacteria, or animal cells-which means each batch has tiny, natural variations. You can’t just mix chemicals in a lab and get the same result every time. A brand-name biologic like Humira (adalimumab) or Enbrel (etanercept) is made from living systems, and even the manufacturer can’t produce two identical bottles. So how do you make a copy? You don’t. You make something highly similar. That’s what a biosimilar is. The FDA requires manufacturers to prove, through dozens of tests, that the biosimilar matches the original in structure, how it works in the body, how it’s absorbed, and how safe it is. No clinically meaningful differences. That’s not marketing speak-it’s science backed by clinical trials on thousands of patients. And here’s the kicker: biosimilars are approved under a different law than regular generics. Generics follow the Hatch-Waxman Act from 1984. Biosimilars follow the Biologics Price Competition and Innovation Act (BPCIA) of 2009. The rules are different because the drugs are fundamentally different.Interchangeable Biosimilars: The Real Generic Equivalents
Not all biosimilars are created equal. There’s a special category called interchangeable biosimilars. These are the ones that can be swapped at the pharmacy without the doctor’s approval-just like generic pills. To get that label, the manufacturer has to prove more than similarity. They have to show that switching back and forth between the brand and the biosimilar won’t increase risk or reduce effectiveness. That’s a higher bar. As of late 2023, only a handful of biosimilars have been approved as interchangeable. The first one for Humira, Amjevita (adalimumab-atto), got the green light in November 2023. That’s a big deal. Humira was the top-selling drug in the world for years, with annual sales over $20 billion. Now, patients who’ve been on it for a decade might switch to a biosimilar without even knowing it-unless their pharmacist tells them. State laws vary. In 32 states, including California, New York, and Texas, pharmacists can substitute interchangeable biosimilars automatically. In others, they need the doctor’s okay. So even if a biosimilar is interchangeable federally, you might not get it unless your state allows it.Why Aren’t Biosimilars Used More?
You’d think with 76 FDA-approved biosimilars, they’d be everywhere. But they make up less than 20% of the biologic market. Why? First, cost savings aren’t as big as with generics. A regular generic can cut a brand-name drug’s price by 80-85%. Biosimilars? More like 10-50%. That’s still a lot, especially for drugs that cost $20,000 a year, but it’s not the same shock to the system. Second, there’s fear. Some doctors and patients worry that switching from a brand-name drug they’ve been on for years might cause problems. One study found that 37% of patients had their treatment disrupted when insurers forced a switch. But only 12% of those patients actually got worse. That’s a key point: disruption doesn’t always mean harm. Third, the system is built to resist change. Brand-name companies use patent lawsuits to delay biosimilar entry. On average, they file nearly 15 patent challenges per biosimilar. That’s legal friction designed to protect revenue. It works. Some biosimilars sit on shelves for years after approval because of court battles. And then there’s education. Many doctors weren’t trained on biosimilars in medical school. A 2022 survey by the American College of Rheumatology found it takes 6-8 hours of training for physicians to feel confident prescribing them. That’s not a small barrier.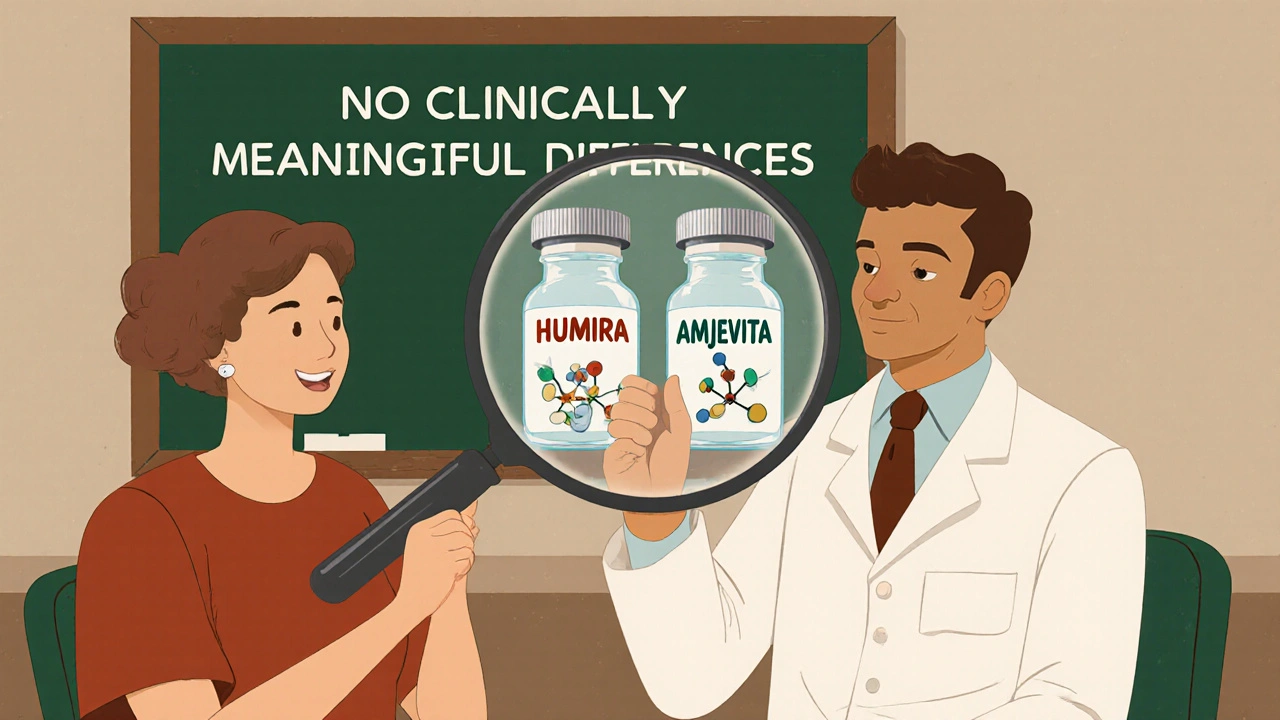
Real Patient Experiences
Patients aren’t just numbers. One woman on the American Cancer Society’s forum switched from Herceptin to its biosimilar for breast cancer. Her out-of-pocket cost dropped from $1,200 per infusion to $450. No side effects. Same results. Another patient, with rheumatoid arthritis, switched three times between the brand and two different biosimilars. She developed new injection site reactions after the third switch. Was it the biosimilar? Maybe. But no one could prove it. That’s the problem with real-world data-it’s messy. Insurance companies are pushing biosimilars hard because they save money. Medicare Part D plans cover 62% of biosimilars at the same tier as the brand. That means lower copays. But 28% put them on a preferred tier, which sounds good until you realize it means you might be forced to switch.Who Makes Biosimilars?
Three big players dominate the U.S. market: Amgen, Sandoz (a Novartis company), and Pfizer. Amgen has 12 approved biosimilars. Sandoz has 8. Pfizer has 7. Together, they’ve brought down prices for drugs used in cancer, autoimmune diseases, and diabetes. Hospitals are leading the way. A 2022 survey found 87% of U.S. hospitals have formal policies to use biosimilars when available. That’s because they buy in bulk and can negotiate better prices. Community pharmacies? Slower to adopt. They’re often caught between insurance rules, patient fears, and unclear labeling.
The Future Is Here
The global biosimilar market was worth $10.1 billion in 2022. By 2030, it’s projected to hit $58.6 billion. That’s a 24% annual growth rate. Why? Because biologics are exploding. Over $115 billion in biologic sales are set to lose patent protection by 2028. That’s a goldmine for biosimilar makers. The FDA is speeding things up. Their Biosimilars Action Plan aims to approve 15-20 new biosimilars a year by 2025. In May 2023, they released new guidance to make labeling clearer. Now, every biosimilar must clearly state which brand it copies and which conditions it treats. No more confusion. Congress estimates biosimilars will save Medicare $53 billion between 2024 and 2033. The whole U.S. healthcare system could save $314 billion over the next decade. That’s not just money-it’s access. More people can get treated. More patients can afford insulin. More families won’t have to choose between rent and their medication.What You Need to Know
If you’re on a biologic drug:- Ask your doctor if a biosimilar is an option.
- Check with your pharmacy. Are they allowed to substitute? Do they have one in stock?
- Look at your insurance formulary. Is the biosimilar on a lower tier?
- Don’t assume switching is dangerous. For most people, it’s safe and effective.
- If you have a bad reaction after switching, report it. But don’t panic. One bad experience doesn’t mean all biosimilars are risky.
Are biosimilars the same as generic drugs?
No. Generic drugs are exact chemical copies of small-molecule drugs like aspirin or cholesterol pills. Biosimilars are highly similar but not identical copies of complex biologic drugs made from living cells. Because biologics are so complex, exact copies aren’t possible. Biosimilars must prove they work the same way and are just as safe, but they’re not chemically identical.
Can pharmacists substitute biosimilars without asking my doctor?
Only if the biosimilar is labeled as "interchangeable" and your state allows it. As of 2025, 32 states-including California, New York, and Texas-permit pharmacists to swap interchangeable biosimilars without a doctor’s approval. In other states, the pharmacist must contact your doctor first. Always ask your pharmacist if substitution is allowed.
How much money do biosimilars save?
Biosimilars typically cost 10% to 50% less than the brand-name biologic. That’s less than the 80-85% savings you get with regular generics, but still significant. For a drug that costs $20,000 a year, even a 30% discount saves $6,000 annually. Over time, that adds up for patients, insurers, and the healthcare system.
Are biosimilars safe?
Yes. The FDA requires biosimilars to meet the same high standards as brand-name biologics. They must prove no clinically meaningful differences in safety, purity, or effectiveness. Thousands of patients have used biosimilars for years with no increase in side effects. The FDA continues to monitor them after approval. If anything unusual happens, it’s reported and investigated.
Why aren’t more biosimilars available in the U.S.?
Patent lawsuits delay entry. Brand-name drugmakers file an average of 15 patent challenges per biosimilar to block competition. Also, doctors and patients are often hesitant to switch, and insurance rules vary. Plus, biosimilars are harder and more expensive to develop than generics, so fewer companies enter the market. But with more biologics losing patents by 2028, expect a big increase in biosimilar options.







Chrisna Bronkhorst
Biosimilars are just pharma's way of milkin' the system with fancy labels. Same drug, different price tag. They call it 'highly similar' like that means something. If it works the same, why not just call it a copy? The real villain is the patent trolling. 15 lawsuits per biosimilar? That's not innovation, that's extortion.
Shante Ajadeen
I switched my mom from Humira to a biosimilar last year. Her copay dropped from $800 to $120. No side effects, no drama. She didn't even notice until I told her. If your doctor says it's safe, just go for it. Money saved = more groceries, more gas, less stress.
Amie Wilde
My pharmacist switched me without asking. I didn't even know until I got the bill. Best thing ever. Saved me $5k a year. No issues. Why is this even a debate?
Johnson Abraham
lol biosimilars are just placebo with a lab coat. Big pharma lets them in so they can say 'we lowered prices!' while still charging $15k. The real savings? Gone. Into the pockets of the same CEOs who made the original drug. Also, my cousin got a rash after switching. Coincidence? I think not. 😏
Elizabeth Buján
I used to think biosimilars were just cheap knockoffs. Then my brother got on one for his Crohn's. He went from crying in the bathroom after infusions to hiking on weekends. No magic, just science. But man, the system is rigged. Patent lawsuits? 15 per drug? That's not protection, that's greed with a law degree. We need to stop letting corporations hold patients hostage for profit. This isn't just about money-it's about dignity. People shouldn't have to choose between rent and life.
And yeah, some docs are scared to switch patients. But that's because they weren't trained. Not because biosimilars are dangerous. We need mandatory continuing ed for prescribers. Not lawsuits. Education. Compassion. Real talk.
When I first heard 'biologic' I thought it meant 'organic.' Like, green tea in a syringe. Turns out it's just living cells in a bioreactor. Weird. Beautiful. Complex. And yeah, we can't copy it exactly. But we can make something damn close that saves lives. That's not a compromise. That's progress.
I get why people are nervous. Switching meds is scary. But fear shouldn't be the default setting. Data says it's safe. Real people say it works. So why are we still arguing?
And don't get me started on state laws. One state says you can swap, another says you need a note from your grandma. This isn't healthcare. It's a bureaucratic maze designed to confuse people into giving up.
Amgen, Sandoz, Pfizer-they're not saints. But they're the only ones pushing this forward. Maybe we should thank them instead of calling them villains. The real villains are the ones who sit in boardrooms and count how many patients they can afford to lose.
I used to think healthcare was broken. Now I think it's just asleep. Biosimilars are the alarm clock. Loud. Annoying. Maybe even a little scary. But necessary.
Eve Miller
There is a critical error in the article: biosimilars are not approved under the Hatch-Waxman Act. That is exclusively for small-molecule generics. Biosimilars are governed solely by the BPCIA. This is not a minor oversight-it is a foundational misunderstanding of U.S. pharmaceutical regulation. The distinction is legally and clinically significant. Please correct this immediately.
Esperanza Decor
My sister’s oncologist told her biosimilars were 'experimental.' She cried. Turned out it was just his ignorance. She switched to the biosimilar, saved $400/month, and her tumor markers are stable. Why are doctors still acting like this is uncharted territory? We’ve had biosimilars in Europe for 15 years. The science isn’t new. The fear is.
And why does insurance only cover them if you agree to switch? That’s not choice. That’s coercion. If the drug is safe, why force people? Let patients decide.
Deepa Lakshminarasimhan
Did you know the FDA gets funding from pharma companies? They approve biosimilars so fast because they’re being paid off. The real reason they're pushing this is to make you dependent on cheaper drugs that are secretly less effective. They want you to get hooked on the biosimilar so they can raise prices later. They did it with insulin. They'll do it again. Watch.
Gary Hattis
I’m from South Africa, and we’ve had biosimilars for years. In Cape Town, you can get a Humira biosimilar for $150 a month. Here? $1,500. Same drug. Same science. Different country. Different greed. The U.S. is the only developed country where you pay 10x more for the same medicine. It’s not about innovation. It’s about profit. And it’s killing people.
When I worked in a clinic in Nairobi, we had a patient who skipped doses because she couldn’t afford the brand. She got a biosimilar last year. She’s back at work. That’s not a statistic. That’s a human being. Why does America treat healthcare like a luxury?
Danae Miley
Interchangeable biosimilars require additional switching studies-not just one, but multiple cycles of alternating between brand and biosimilar. This is not a trivial regulatory hurdle. The FDA’s guidance on this is meticulous. The fact that only a few have achieved this status reflects the rigor of the process, not industry failure. Mischaracterizing this as 'bureaucratic delay' undermines public trust in regulatory science.
dace yates
So if a biosimilar is interchangeable, why do some pharmacies still refuse to switch without a doctor’s note? Is it the law? Or just fear? I called three pharmacies. Two said they didn’t stock any. One said they’d need a new prescription. I didn’t even ask for a biosimilar. I just asked if they had it. Confusing.