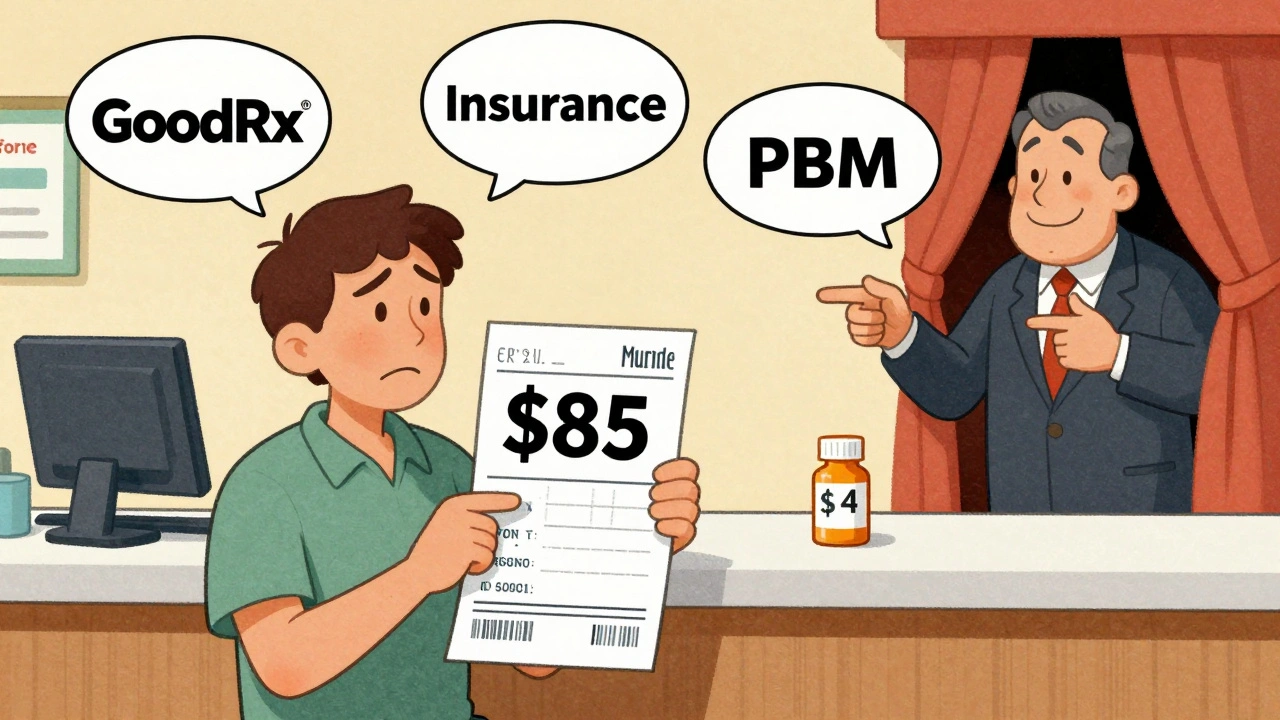
Have you ever picked up a generic prescription and been shocked by the price? You know it’s supposed to be cheap - it’s generic, after all - but the receipt says $85 for a 30-day supply? You’re not alone. In 2025, generic drug prices still vary wildly across pharmacies, insurers, and states, even for the same medication. Some people pay $4. Some pay $40. And no one seems to know why.
Why Generic Prices Are So Confusing
Generic drugs are supposed to be the affordable alternative to brand-name pills. But the system behind the price isn’t simple. It’s a tangled web of manufacturers, pharmacy benefit managers (PBMs), insurers, and pharmacies - each taking a cut, hiding rebates, and setting their own rules. What you see on the shelf isn’t what the pharmacy actually paid. What your insurer thinks it’s covering isn’t what the pharmacy charges. And what you pay at the counter? That’s often just a guess. The list price - the manufacturer’s suggested price - is rarely what anyone actually pays. Real prices are buried under rebates, discounts, and negotiated deals that only PBMs and insurers see. Patients are left in the dark, paying whatever the pharmacy says - unless they know where to look.Real-Time Benefit Tools: What Doctors Use to Save You Money
If you’ve ever had your doctor pause mid-prescription to check a screen, they’re probably using a Real-Time Benefit Tool (RTBT). These systems connect directly to your insurance plan and show the exact cost of a drug - before the prescription is even printed. Tools like CoverMyMeds and Surescripts are now used in 42% of U.S. physician practices as of 2025. When your doctor types in a drug name, the system pulls your specific coverage details: your deductible, your copay, whether a cheaper generic is covered, and if there’s a patient assistance program available. One study found that when doctors used these tools, patients’ out-of-pocket costs dropped by an average of 37%. These tools don’t just show price. They suggest alternatives. That $85 generic? The tool might say, “Switch to this other generic - same active ingredient, $12 copay, covered at your pharmacy.” It’s not magic. It’s data - and it’s becoming standard in clinics that want to reduce patient abandonment of prescriptions due to cost.GoodRx and Other Consumer Apps: Your Phone Can Be Your Price Checker
You don’t need a doctor’s office to find a better price. Apps like GoodRx, SingleCare, and RxSaver let you search for the lowest cash price for any generic drug - no insurance needed. GoodRx alone is used by 43% of U.S. pharmacies, according to J.D. Power’s 2024 survey. Type in your drug and zip code, and it shows prices at nearby pharmacies - CVS, Walgreens, Walmart, even independent shops. Some users report saving $50 or more per prescription. But here’s the catch: the price you see online isn’t always the price you pay. Many users report walking into a pharmacy with a GoodRx coupon, only to be told, “Our system doesn’t recognize that.” Why? Because pharmacies update their prices in real time, and some don’t sync with third-party apps. Others have policies that limit how much they honor coupons. Trustpilot reviews for GoodRx average just 2.1 stars - not because the app is wrong, but because the system it’s trying to fix is broken.
State Laws Are Changing the Game
While federal efforts have stalled, states are stepping in. As of April 2025, 23 states have passed laws requiring drug price transparency. Some go further. Minnesota’s law lets you compare prices for the same generic drug across pharmacies in your area - and one patient saved $287 a year by switching from a local CVS to a nearby grocery store pharmacy. California requires drugmakers to report price hikes over 16% in two years. New York mandates that insurers disclose what they pay for drugs, not just what patients pay. These laws aren’t perfect, but they’re forcing more data into the open. The biggest win? Prescription Drug Affordability Boards (PDABs) in 12 states. These panels review high-cost drugs and can cap prices for state-funded programs. They don’t control private insurance - yet - but they’re setting a precedent.What You Can Do Right Now
You don’t need to wait for a law or a doctor to save money on generics. Here’s how to take control:- Use GoodRx or SingleCare before you fill your prescription. Compare prices at three nearby pharmacies.
- Ask your pharmacist: “Is there a lower-cost generic version?” Sometimes the same drug is sold under a different name with a cheaper price tag.
- Check RxAssist.org - it’s a free database of manufacturer assistance programs. Many offer free or discounted meds to people with low income.
- If you’re on Medicare, use the Medicare Plan Finder tool. It shows your exact out-of-pocket cost for each drug under your plan.
- Ask your doctor if they use a real-time benefit tool. If not, request it. Many clinics will set it up if patients ask.

Why Transparency Alone Isn’t Enough
Even with all these tools, the system still doesn’t show you the full picture. You’ll never see the real net price - the amount the insurer actually paid after rebates. That’s because those deals are secret. PBMs keep them hidden, arguing that revealing them would hurt competition. But here’s the irony: when prices are hidden, patients pay more. A 2025 study in Health Affairs found that when patients could see the price difference between brand and generic, they chose the generic 8.2% more often. But when prices were hidden, they stuck with the expensive option - even if it meant skipping doses. The truth? Price transparency tools don’t fix the system. They just help you navigate it. Until the rebate system changes, the best price won’t always be the lowest listed price. It’ll be the one you find after asking questions, comparing options, and refusing to accept the first number you’re given.What’s Coming in 2025 and Beyond
The Drug-price Transparency for Consumers Act of 2025 (S.229) is moving through Congress. If passed, it would force drug companies to list the wholesale cost of a 30-day supply in every TV or online ad. That’s a big deal. Right now, ads show “As low as $10!” - but never say what that price actually means. The Centers for Medicare & Medicaid Services (CMS) is also expected to release new rules by the end of 2025 that could require insurers to report total drug spending - including rebates. That could finally shine a light on how much PBMs are really making. But don’t wait for Washington to fix it. The tools are here now. The data is out there. You just have to use it.Why is my generic drug so expensive even though it’s not brand-name?
Generic drugs are cheaper than brand-name versions, but their prices aren’t fixed. The cost depends on your insurance plan, the pharmacy’s contract with your pharmacy benefit manager (PBM), and whether the manufacturer has raised prices. Some generics cost $4; others cost $80 because of how rebates and contracts are structured behind the scenes. You’re paying what the pharmacy charges - not what they paid for it.
Can I really save money using GoodRx?
Yes - but not always. GoodRx often shows the lowest cash price at nearby pharmacies, and many users save $20-$60 per prescription. But prices can change between when you check the app and when you arrive at the pharmacy. Always ask the pharmacist to check their system with your coupon. If the price doesn’t match, walk out and try another location. Don’t assume the app is wrong - the pharmacy’s system might be outdated.
Do I need insurance to use price transparency tools?
No. Consumer apps like GoodRx and SingleCare work without insurance - they show cash prices. Real-time benefit tools used by doctors require your insurance info to show your exact copay. If you’re uninsured, use GoodRx or check RxAssist.org for free or discounted meds from manufacturer programs.
Why won’t my pharmacy honor my GoodRx coupon?
Some pharmacies have policies that limit how much they can discount drugs, especially if they’re already operating on thin margins. Others don’t have the systems to process third-party coupons. It’s not illegal - it’s just how their contracts work. If your coupon isn’t accepted, ask for the cash price anyway. Sometimes the pharmacy’s internal price is lower than the coupon.
Are there free programs to get cheap or free generic drugs?
Yes. RxAssist.org lists over 1,000 patient assistance programs from drug manufacturers. Many offer free or low-cost meds to people with low income, no insurance, or high deductibles. You’ll need to apply, and some require proof of income, but 78% of applicants get approved. It takes time, but it can save hundreds per year.

Paul Dixon
Just used GoodRx for my blood pressure med and saved $42. Walked into CVS with the coupon and they said ‘nope’ - so I went to Walgreens next door and got it for $12. Felt like a detective. 🕵️♂️
matthew dendle
so pbms are just middlemen who make money by keeping prices confusing lmao. we’re all paying for their private jets and yachts. why dont we just burn the whole system down? 🤡
Mia Kingsley
you guys are all missing the point. the real issue is that generics are just brand names with different packaging. the FDA lets them get away with it. i took a generic Adderall once and it made me hallucinate my cat was singing opera. not cool.
Jimmy Kärnfeldt
It’s wild how much power we actually have if we just take five minutes to look. I used to just pay whatever the counter said - now I check GoodRx, call three pharmacies, and sometimes even ask the pharmacist for the cash price before they swipe my card. Saved me over $600 last year. Small steps, big savings.
Kristi Pope
my grandma just found out about RxAssist.org and got her insulin for free. she cried. not because she was sad - because she finally felt seen. these tools aren’t just about money, they’re about dignity. we gotta keep pushing for more of this stuff.
Jean Claude de La Ronde
in canada we just pay $5 for everything and call it a day. you americans are out here negotiating drug prices like it’s a flea market. why do you even have PBMs? are they the reason your healthcare system looks like a broken vending machine?
john damon
so i tried the RTBT thing at my doc’s office and they said ‘oh we don’t use that’ so i said ‘well i’m switching doctors’ and they did it the next week 😂 also my pharmacist now texts me when my meds are cheaper. i’m basically a healthcare influencer now 📱💊
Jim Irish
Transparency tools help. But real change needs systemic reform. The rebate structure must be restructured to align incentives with patient outcomes. Until then, individuals must remain vigilant.
Aman deep
in india we get generics for like 10 rupees but here people act like $85 is normal. i used to work at a pharmacy in delhi - we had people driving 50 miles just to buy pills cheaper. america is broken but we’re trying. small wins matter.
Ariel Nichole
just got my prescription filled using SingleCare - $17 instead of $89. i told my pharmacist about the article and she said ‘oh we get that question every day.’ turns out, she uses GoodRx too. we’re all in this together. thank you for sharing this. it matters.