Every year, millions of people take generic medicines from countries they’ve never visited. A pill made in India might end up in a pharmacy in Brazil, Canada, or Germany. But here’s the problem: if something goes wrong - if a patient has a bad reaction - who knows? Who collects that data? And how fast can it be acted on? That’s where pharmacovigilance harmonization comes in.
Why Global Drug Safety Needs to Be Standardized
Pharmacovigilance isn’t just about tracking side effects. It’s about saving lives. When a drug causes unexpected harm, speed matters. Delays mean more people get hurt. Before international standards, a company selling a medicine in 10 countries had to file 10 different reports, using 10 different formats, following 10 different deadlines. Some countries wanted reports within 7 days. Others gave you 30. One used paper forms. Another required encrypted digital files. The system was broken. The answer? Harmonization. Starting in 1990, regulators from the U.S., Europe, and Japan came together to form the International Council for Harmonisation (ICH). Their goal was simple: make drug safety rules the same everywhere. Today, that means using the same definitions, the same reporting formats, and the same timelines - at least in theory. The result? Companies now save months preparing submissions. The FDA estimates harmonization cuts time to market by 15-20%. That’s not just money saved - it’s patients getting safe drugs faster. And it’s not just about big pharma. Generic manufacturers, who make up over 80% of global medicines, rely on these standards too. Without them, getting a low-cost drug approved across borders would be impossible.How the ICH Guidelines Work - and Where They Fall Short
The backbone of global pharmacovigilance is the ICH E2 series. These are the technical rules that tell companies how to report adverse events. E2B(R3) is the current standard for electronic case reports. It’s a single format that 89% of top pharmaceutical companies now use. That’s a huge win. Before E2B(R3), 18-22% of reports got rejected just because of coding errors. But here’s the catch: even with ICH, rules aren’t identical everywhere. The FDA requires companies to report serious, unexpected side effects within 15 days. The European Medicines Agency (EMA) does too - but only for certain types of drugs. For others, they allow up to 30 days. Japan’s PMDA has its own twist: they use AI to predict which reports are likely false alarms, cutting down noise by 25%. Meanwhile, China still demands local reporting within 15 days - even if the same case was already sent to the FDA. This isn’t just confusing. It’s costly. A 2023 survey of pharmacovigilance managers found that 82% spend 30-40% of their time just rewriting reports for different regions. One professional on Reddit said they spend over 100 hours a month adapting documents. That’s not science. That’s paperwork.Real-World Data: The Missing Piece
The future of pharmacovigilance isn’t just in forms and deadlines. It’s in data - real data from real patients. Electronic health records, insurance claims, wearable devices - these can show patterns no clinical trial ever could. The EU has mandated EHR integration since 2021. The FDA’s Sentinel Initiative now monitors 300 million patient records. The EMA’s DARWIN EU network covers 100 million. But not every country can do this. In Brazil, South Africa, and parts of Southeast Asia, fewer than 15% of potential data sources are even accessible. Why? No digital infrastructure. No trained staff. No funding. A 2022 survey found that 74% of pharmacovigilance teams in low- and middle-income countries couldn’t meet even basic ICH standards. Meanwhile, high-income countries had only 8% struggling. This gap isn’t just unfair - it’s dangerous. If a drug causes harm in Nigeria but no one can report it, the signal gets lost. That’s why WHO’s Global Smart Pharmacovigilance Strategy, being finalized in 2025, aims to set common data standards for all 150 member states by 2027. But funding is a wall. Deloitte estimates a $1.8 billion shortfall just to bring basic systems to the poorest countries.
Technology Is Changing the Game - But Unevenly
AI isn’t science fiction in pharmacovigilance anymore. The EMA and FDA started using machine learning in 2022 to find safety signals. Their systems now detect problems 30-40% faster than old manual methods. Japan’s PMDA uses AI to filter out false alarms, reducing noise by a quarter. That means teams can focus on real threats. But these tools aren’t free. They need data. They need skilled staff. And they need validation. That’s why ICH announced in March 2024 that it’s working on global AI validation standards - due by mid-2026. Until then, a model that works in the U.S. might be rejected in India because it doesn’t meet local rules. And the skills needed? They’ve changed. Today, pharmacovigilance professionals aren’t just pharmacists or nurses. They need to understand data science. A 2024 survey found that 76% of leading companies now require their safety teams to have basic machine learning literacy. If you can’t read a Python script or interpret a predictive model, you’re falling behind.Who’s Leading - and Who’s Left Behind
The U.S. and EU are far ahead. Over 95% of companies there fully follow ICH E2 guidelines. Japan isn’t far behind. Canada aligns closely, though it still requires 30-day reporting for serious events - a small but persistent difference. Emerging markets? Not so much. Only 42% of companies in Latin America, Africa, and parts of Asia have adopted ICH E2B(R3). In some countries, less than 31% have even basic digital reporting systems. The WHO’s VigiBase - the world’s largest safety database with over 35 million reports - relies on data from 134 countries. But many of those reports are incomplete. Some are handwritten. Others arrive months late. This isn’t just a compliance issue. It’s a safety crisis. A 2023 Deloitte report estimated that full harmonization could prevent 1,200-1,500 drug-related deaths per year. But that only happens if every country can participate.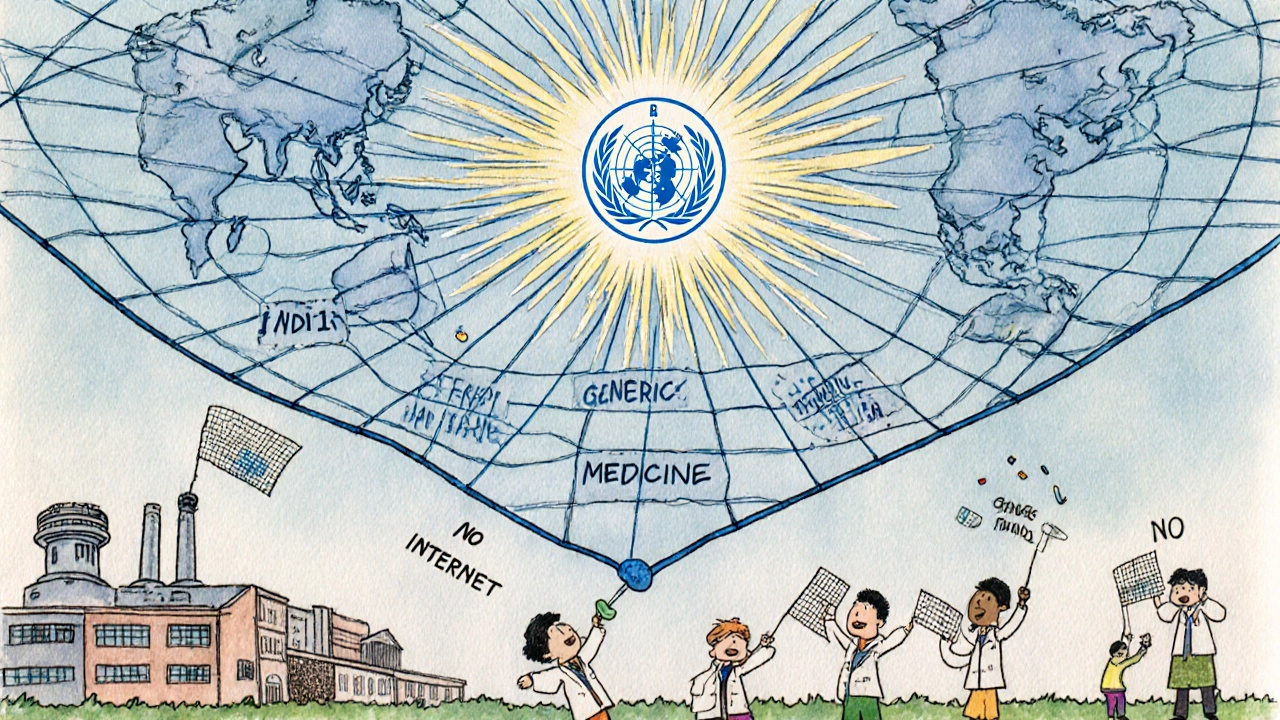
What Needs to Change - and How
Harmonization isn’t about forcing everyone to be like the U.S. or Europe. It’s about making systems talk to each other. Here’s what’s working:- Standardized formats: E2B(R3) is the gold standard. Every country should use it.
- Shared AI tools: ICH’s new AI validation guidelines could level the playing field.
- Global data sharing: WHO’s upcoming strategy must include funding for infrastructure in low-resource settings.
- Training programs: Pharmacies in Kenya or Vietnam need access to the same training as those in Boston or Berlin.







Elia DOnald Maluleke
The global pharmacovigilance architecture, as it stands, is a monument to bureaucratic inertia dressed in the robes of scientific progress. We speak of harmonization, yet the very architecture of reporting remains a Tower of Babel where the same adverse event is translated into ten dialects of compliance. The ICH E2B(R3) standard? A noble attempt - but it is not law, it is suggestion wrapped in PDF. And in the Global South, where the pills are consumed but the data streams dry up, we are not participants - we are footnotes in a report written by others, for others. The $1.8 billion gap? That’s not a budget line. That’s a chasm of moral abandonment.
satya pradeep
Bro, as someone who works in pharma safety in Pune, I can tell u this: we got a guy who prints out E2B forms, fills them by hand, scans ‘em, emails ‘em to the FDA, then does it all over again for EMA. Why? Because our local system doesn’t talk to theirs. And yeah, we got AI tools - but they’re trained on US/EU data. So when a patient in Bihar has a reaction to a generic metformin, the algorithm says ‘false alarm’ because ‘no precedent.’ We’re not lagging behind - we’re being erased by design. Someone needs to fund real infrastructure, not just more guidelines.
Leslie Douglas-Churchwell
Let’s be real - this whole ‘harmonization’ is a corporate Trojan horse. 🤫 Big Pharma loves ICH because it lets them dump the same half-tested drug in 150 countries with one report. The FDA? EMA? They’re not regulators - they’re gatekeepers for patent extensions. And don’t get me started on AI ‘signal detection.’ If your algorithm can’t recognize that a 78-year-old in Lagos having a stroke after taking a $0.10 pill is a signal, then you’re not saving lives - you’re optimizing shareholder returns. 🚨📉 #BigPharmaLies
Kathryn Ware
Hi everyone - I’m a pharmacovigilance lead at a mid-sized US firm, and I just wanted to say how much I appreciate this thread. 🙌 The part about real-world data is so true - we just integrated our EHR feed with Sentinel and saw a spike in rhabdomyolysis with a generic statin that no clinical trial ever caught. It’s wild how much we miss when we only rely on clinical trial data. And yes, the paperwork is insane - I spent 40 hours last month just reformatting E2B files for Brazil’s ANVISA. But here’s the good news: we’re piloting a tool that auto-translates ICH reports into local formats using NLP. It’s not perfect, but it cut our workload by 60%. If anyone’s working on open-source harmonization tools, DM me - I want to help. We can fix this - together. 💪🌍
shubham seth
Harmonization? More like homogenization of accountability. The U.S. and EU get to call the shots, then act shocked when a drug kills 300 people in Nigeria and nobody knew because the local clinic still uses carbon paper. The ICH guidelines are a luxury - like expecting a farmer in Malawi to run a Tesla factory because the manual says ‘all cars should have airbags.’ And now they want us to learn Python? Cool. Meanwhile, our hospital’s internet cuts out every afternoon. The real ‘AI’ here is the one that predicts which countries will be sacrificed first when the next recall hits. 🤡
kora ortiz
This is the most important public health issue no one talks about and we’re actually making progress. Every report filed, every standard aligned, every trainee in Kenya getting trained - it adds up. Keep pushing. We’re not perfect but we’re moving.
Bill Machi
Let’s cut the fluff. This isn’t about global equity - it’s about liability. If a drug kills someone in India, the U.S. company still gets sued. So yes, they want harmonization - so they can bury the blame under a mountain of compliant paperwork. The real solution? Stop exporting drugs to countries that can’t monitor them. Let them make their own generics. Let them bear the risk. We’re not the world’s pharmacist. We’re a nation of taxpayers footing the bill for a system designed to protect corporate profits, not patients in Lagos or Lima. End the charade.
Prem Hungry
Bro, I feel you. I’ve been in this field for 18 years. I’ve seen reports get lost in fax machines, rejected because the patient’s age was written as ‘45 yrs’ instead of ‘45,’ and I’ve watched colleagues cry because their 3-month work got tossed because of a missing ICH MedDRA code. But here’s what I tell my juniors: don’t quit. The system is broken, yes - but someone has to keep sending the reports. Someone has to keep training the interns in Dhaka. Someone has to keep pushing the AI models to learn from non-Western data. You think the FDA doesn’t know this? They do. And they’re slowly changing. One E2B(R3) file at a time. Stay in the game. The world needs you. 🙏