When a drug is highly variable - meaning its effects differ widely from person to person - standard bioequivalence (BE) studies often fail. You might test 100 people and still not get a clear answer. That’s where replicate study designs come in. These aren’t just fancy versions of old trials. They’re the only way to fairly assess whether a generic version of a tricky drug behaves the same as the brand-name version in real patients.
Why Standard Designs Don’t Work for Highly Variable Drugs
Most bioequivalence studies use a simple two-period, two-sequence crossover: half the subjects get the test drug first, then the reference; the other half get it in reverse. This works fine for drugs with low variability - say, a blood pressure pill that acts predictably in most people. But for drugs like warfarin, levothyroxine, or certain antiepileptics, the body absorbs or metabolizes them so differently between individuals that the usual 80-125% bioequivalence range becomes meaningless.
Here’s the problem: if the reference drug’s within-subject coefficient of variation (ISCV) is above 30%, the standard approach demands huge sample sizes - sometimes over 100 people - just to have a shot at proving equivalence. That’s expensive, slow, and ethically questionable when you’re asking volunteers to go through multiple dosing periods with no guarantee of success.
Regulators noticed this. The FDA started pushing for better methods in the early 2000s. By 2010, the EMA had followed suit. Both now require replicate designs for any drug with an ISCV over 30%. Why? Because you can’t judge equivalence fairly if you don’t understand how much the drug varies within the same person.
How Replicate Designs Work
Replicate designs repeat doses of both the test and reference products across multiple periods, so you can measure how much the drug’s behavior changes within each individual. There are three main types:
- Three-period full replicate (TRT/RTR): Each subject gets the test drug once and the reference drug twice. This lets you estimate variability for both products.
- Four-period full replicate (TRRT/RTRT): Each subject gets both drugs twice. This gives the most precise data, especially for narrow therapeutic index (NTI) drugs like warfarin.
- Three-period partial replicate (TRR/RTR/RRT): Subjects get the reference drug twice but the test drug only once. You can only estimate reference variability, but it’s cheaper and faster.
These aren’t just about repeating doses - they’re about gathering the right kind of data. In a standard study, you can’t tell if differences between test and reference are due to formulation or just natural variation in how people absorb the drug. In a replicate design, you can isolate within-subject variability. That’s the key.
Reference-Scaled Average Bioequivalence (RSABE)
This is the statistical engine behind replicate designs. Instead of forcing all drugs into a rigid 80-125% acceptance range, RSABE adjusts the limits based on how variable the reference drug is. The more variable it is, the wider the acceptable range - but only if the test drug is no more variable than the reference.
For example, if the reference drug has an ISCV of 45%, the bioequivalence limits might stretch to 70-143%. That sounds loose, but it’s scientifically justified. The goal isn’t to make the drugs identical - it’s to make them therapeutically equivalent. If both drugs swing wildly in the same way, then matching their variability is more important than matching their average concentration exactly.
The FDA and EMA both use RSABE, but with slight differences. The FDA allows partial replicate designs for RSABE. The EMA requires full replicate designs for most cases. Both agree: if you’re working with a drug that has high variability, you need this method.

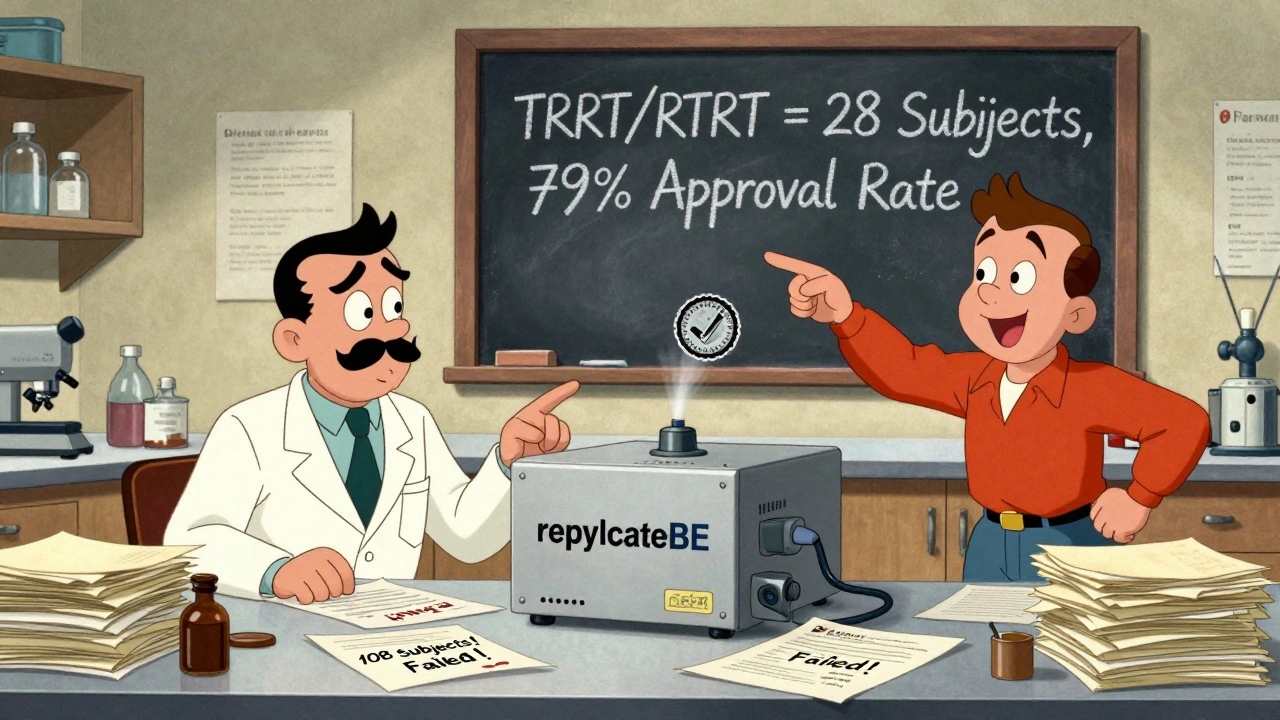
Sample Size Savings Are Real
Let’s say you’re testing a drug with an ISCV of 50%. In a standard 2x2 crossover, you’d need about 108 subjects to have an 80% chance of proving bioequivalence. With a three-period full replicate design? Just 28.
That’s a 74% reduction in participants. That’s not just cost savings - it’s faster approvals, less burden on volunteers, and more efficient drug development. A 2023 survey of 47 contract research organizations (CROs) found that 83% consider the three-period full replicate (TRT/RTR) the sweet spot: enough power, manageable duration, and regulatory acceptance across major markets.
For drugs with ISCV over 50%, like some anticoagulants or antiepileptics, the four-period design becomes necessary. The FDA’s 2023 guidance on warfarin sodium specifically mandates TRRT/RTRT. Why? Because even small differences in absorption can lead to dangerous bleeding or clotting. You need every bit of precision you can get.
Where Replicate Designs Fall Short
They’re not magic. If your drug’s ISCV is under 30%, stick with the simple 2x2 design. Replicate studies add complexity without benefit. They’re also harder to run.
Long half-life drugs mean weeks between doses. That increases dropout risk. One study reported a 30% dropout rate in a four-period trial for a drug with a 48-hour half-life. That forced the sponsor to recruit 30% more subjects than planned - adding $187,000 to the budget.
Statistical analysis is another hurdle. You can’t just plug data into Excel. You need specialized software like Phoenix WinNonlin or the R package replicateBE. Analysts typically need 80-120 hours of training to use these tools correctly. Mistakes in model selection - like assuming equal variances when they’re not - can invalidate results.
Washout periods matter too. If you don’t wait long enough between doses, carryover effects skew results. Many failed studies trace back to poor protocol design, not bad data.
Industry Adoption Is Growing - and Regulatory Pressure Is Too
Back in 2018, only 42% of HVD bioequivalence studies used replicate designs. By 2023, that jumped to 68%. The FDA rejected 41% of HVD submissions that didn’t use them. For properly executed replicate studies, the approval rate is 79%.
The EMA is even stricter: 78% of approved HVD generics in Europe used replicate designs in 2023. WuXi AppTec, PPD, and Charles River now compete heavily in this space. Smaller CROs like BioPharma Services have carved out niches by specializing in statistical analysis - a skill that’s become as valuable as clinical operations.
Regulators aren’t done. The FDA’s 2024 draft guidance proposes standardizing four-period designs for all HVDs with ISCV over 35%. The EMA is holding onto flexibility. The ICH is working on a global harmonization document expected in late 2024. Until then, sponsors must tailor designs to each region’s expectations.
Getting Started: What You Need to Know
If you’re planning a bioequivalence study for a highly variable drug, here’s your roadmap:
- Estimate ISCV from prior data or literature. If it’s below 30%, use a standard 2x2 crossover.
- For 30-50% ISCV, choose a three-period full replicate (TRT/RTR). Minimum 24 subjects - at least 12 must complete the RTR arm.
- For ISCV over 50% or for NTI drugs, go with a four-period full replicate (TRRT/RTRT).
- Recruit 20-30% more subjects than your power analysis suggests to account for dropouts.
- Use replicateBE or WinNonlin for analysis. Don’t try to force it into standard software.
- Validate your model with regulatory guidance. Don’t assume your approach will fly without checking FDA or EMA product-specific guidances.
And remember: this isn’t about doing more work. It’s about doing smarter work. Replicate designs aren’t a luxury - they’re the only fair way to evaluate tricky drugs. Skip them, and you’re gambling with regulatory approval, patient safety, and millions in development costs.
What’s Next?
Machine learning is starting to enter the picture. Pfizer’s 2023 proof-of-concept study used historical BE data to predict optimal sample sizes with 89% accuracy. That could cut planning time in half. Bayesian methods, already accepted by the FDA in rare cases, may become more common.
One thing’s clear: replicate designs are here to stay. They’ve moved from niche tools to industry standard. The question isn’t whether you should use them - it’s whether you’re ready to run them right.
What is a replicate study design in bioequivalence?
A replicate study design is a clinical trial format where participants receive multiple doses of both the test and reference drug across several periods. This allows researchers to measure within-subject variability for each drug, which is critical for highly variable drugs. Common types include three-period (TRT/RTR) and four-period (TRRT/RTRT) designs.
When do you need a replicate design for bioequivalence?
You need a replicate design when the within-subject coefficient of variation (ISCV) of the reference drug exceeds 30%. This is standard for drugs like warfarin, levothyroxine, and certain antiepileptics. Regulatory agencies like the FDA and EMA require replicate designs in these cases to enable reference-scaled bioequivalence (RSABE) analysis.
What’s the difference between partial and full replicate designs?
A partial replicate design (e.g., TRR/RTR) only repeats the reference drug, so you can only estimate its variability. A full replicate design (e.g., TRT/RTR or TRRT/RTRT) repeats both drugs, allowing you to estimate variability for both test and reference. Full designs are preferred for narrow therapeutic index drugs and are required by the EMA for most HVDs.
Why is RSABE used in replicate studies?
RSABE (reference-scaled average bioequivalence) adjusts the bioequivalence acceptance range based on how variable the reference drug is. For highly variable drugs, a fixed 80-125% range is too strict. RSABE allows wider limits - like 70-143% - as long as the test drug’s variability doesn’t exceed the reference’s. This prevents false failures due to natural biological variation.
What software is used to analyze replicate study data?
The industry standard is the R package replicateBE (version 0.12.1) and Phoenix WinNonlin. These tools handle mixed-effects models and reference-scaling calculations required for RSABE. Standard statistical packages like SAS or SPSS cannot perform these analyses correctly without custom programming.
How many subjects are needed for a replicate BE study?
For a three-period full replicate design (TRT/RTR) with ISCV of 40-50%, 24-48 subjects are typically sufficient. For ISCV above 50% or for NTI drugs, 36-72 subjects in a four-period design are common. Always over-recruit by 20-30% to account for dropouts, especially with long half-life drugs.
Are replicate designs accepted by both FDA and EMA?
Yes, both agencies accept replicate designs for highly variable drugs. The FDA allows both partial and full replicate designs for RSABE. The EMA requires full replicate designs and has stricter rules on sequence allocation. Always check product-specific guidance - regional differences still exist.


Iris Carmen
lol i just read this and thought 'wait so we're just making the rules up as we go?' like why not just say 'if it works in people, it works' and call it a day?
Michael Robinson
it's not about being exact. it's about being safe. if your body reacts wildly to a drug, you don't want a generic that acts even wilder. this makes sense.
Ronald Ezamaru
I've seen too many studies where they skip the replicate design just to save money. Then patients get sick because the generic wasn't actually equivalent. This isn't bureaucracy-it's harm reduction.
ian septian
Use TRT/RTR. 24 subjects. Done.
Steve Sullivan
i used to think this was overkill until my cousin had a seizure because the generic levothyroxine was off by 10%. now i get it. the body doesn't care about your budget.
Chris Marel
This is fascinating. In Nigeria, we often get generics without any of this testing. I wonder how many people are affected by this silently.
Elliot Barrett
Why do we even bother with all this? Just let the market decide. If it sells, it works.
Andrea DeWinter
For anyone new to this-don’t skip the power analysis. I’ve seen teams blow $2M because they assumed 30 subjects would be enough for a 55% ISCV drug. It wasn’t. You need at least 48. And always over-recruit. People drop out. Life happens.
Katie Harrison
I appreciate the clarity here. But I must note: regulatory divergence between FDA and EMA creates unnecessary complexity for global sponsors. Harmonization isn't optional-it's ethical.
Kathy Haverly
This is just pharma’s way of charging more. They want you to run expensive studies so they can keep prices high under the guise of 'safety.' Wake up.
Ronald Ezamaru
You're missing the point. If a drug has high variability, the difference between 70% and 130% exposure can mean hospitalization or death. This isn't about profit-it's about preventing overdose or underdose. People aren't lab rats.
precious amzy
One must question the epistemological foundations of RSABE. By scaling acceptance criteria to variability, are we not capitulating to biological chaos? Shouldn't bioequivalence imply constancy, not conditional tolerance?
Steve Sullivan
bro you're overthinking it. if the drug swings like a pendulum, you want the generic to swing the same way. that's it. no philosophy needed. just math and safety.
Noah Raines
Used replicateBE last month for a warfarin study. Took me 3 weeks to learn it. The software doesn't lie. If your model's wrong, it tells you. No guessing. No fudging. Just cold hard stats. If you're doing this, learn the tool. Or hire someone who has.
William Umstattd
I've worked on 12 BE studies. 8 used replicate designs. 3 got rejected because they used partial replicates when full was required. The FDA doesn't play. If you're cutting corners, you're gambling with someone's life. Don't be that guy.