Theophylline Clearance Calculator
Theophylline Clearance Calculator
Theophylline has a narrow therapeutic window (10-20 mcg/mL). This calculator estimates how common medications that inhibit CYP1A2 metabolism can increase your theophylline levels and potentially cause toxicity.
Estimated Theophylline Level After Interaction
New Estimated Level: mcg/mL
Safety Status:
Important: This is an estimate. Always monitor levels clinically.
Why it matters: Theophylline toxicity can cause seizures, irregular heartbeat, or even death.
The FDA reports about 2,000 ER visits each year in the U.S. due to theophylline toxicity.
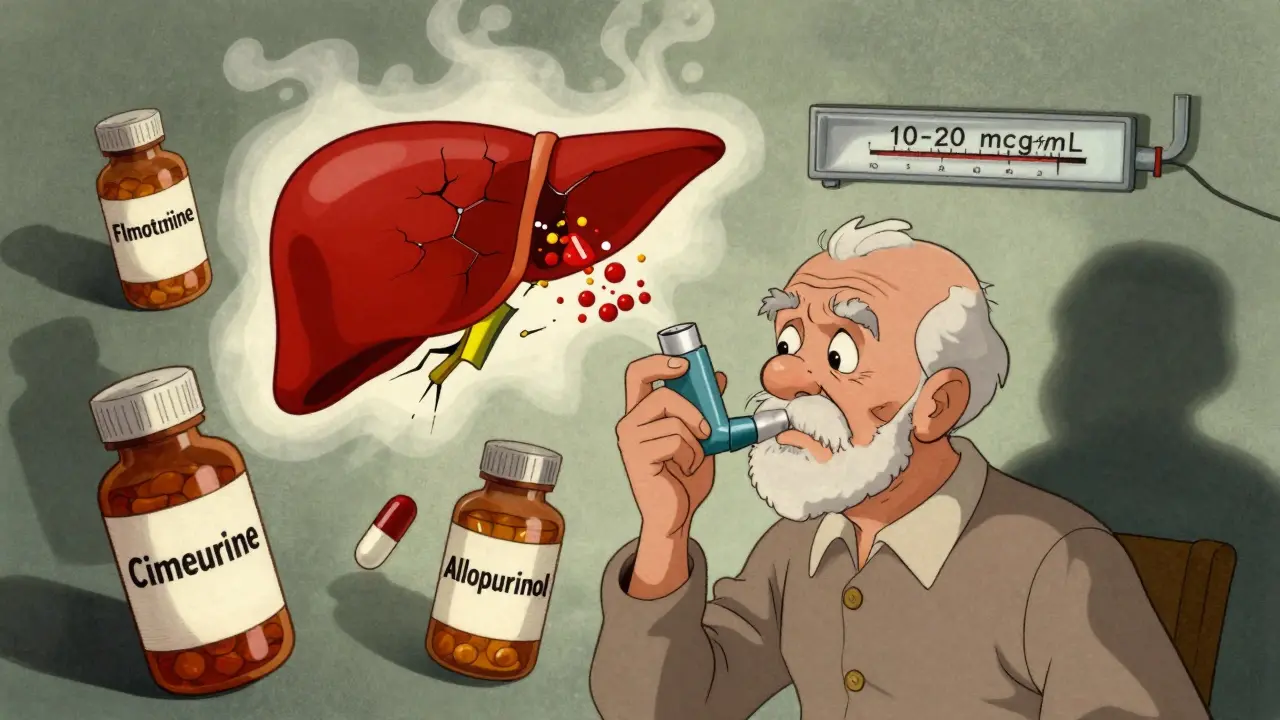
When a patient takes theophylline for asthma or COPD, even a small change in how their body processes the drug can turn a safe treatment into a life-threatening situation. Theophylline has a narrow therapeutic window - between 10 and 20 mcg/mL in the blood. Go just a little above that, and you risk seizures, irregular heartbeat, or even death. And the most common reason for this? Not overdosing. Not misusing. But drug interactions that slow down how fast the body clears theophylline.
Why Theophylline Is So Sensitive
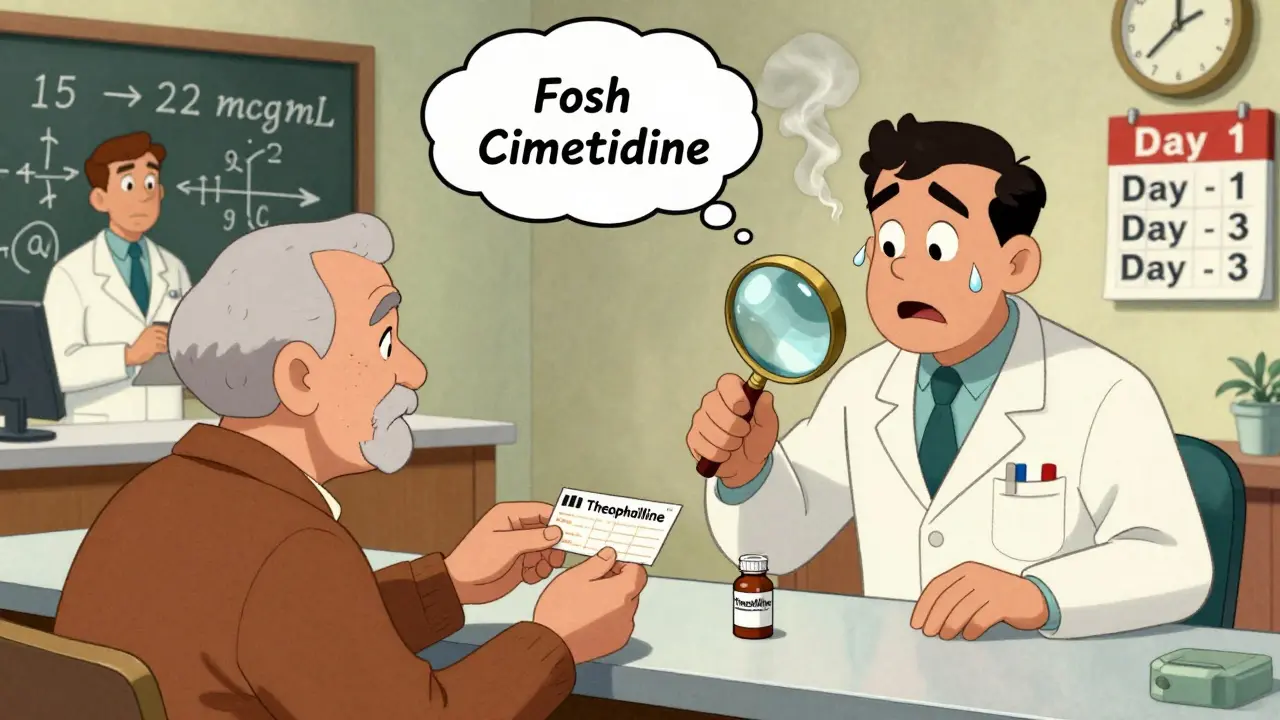
Theophylline isn’t broken down by the kidneys. Around 90% of it is processed by the liver - specifically by an enzyme called CYP1A2. This enzyme is like a factory worker: it takes the drug apart so the body can get rid of it. But if something blocks that worker - say, another medication - the factory backs up. Theophylline builds up. And because its metabolism follows non-linear kinetics, a small drop in clearance doesn’t mean a small rise in blood levels. It means a big one.For example, if a patient’s theophylline level is at 15 mcg/mL - right in the middle of the safe range - and a CYP1A2 inhibitor cuts clearance by 30%, their level could jump to over 22 mcg/mL. That’s toxic. And it can happen in just a few days.
Even more dangerous? Many patients don’t know they’re at risk. Theophylline is rarely the first choice today. Newer inhalers like LABAs and LAMAs are safer, easier to use, and less likely to interact. But it’s still used - especially in older adults, in low-resource settings, and for stubborn nighttime asthma. That means the people taking it are often on multiple other meds. And that’s where things go wrong.
The Top 5 Medications That Slow Theophylline Clearance
Not all drugs affect theophylline the same way. Some barely move the needle. Others are dangerous. Here are the five most common and well-documented culprits:- Fluvoxamine - This antidepressant is one of the strongest CYP1A2 inhibitors out there. It can slash theophylline clearance by 40-50%. A 2020 study in Chest found patients on both drugs had a 12.7-times higher chance of severe toxicity. The European Respiratory Society says: avoid this combo entirely.
- Cimetidine - A common heartburn pill, often sold over the counter. It reduces clearance by 25-30%. In a 2021 study of 1,247 patients over 65, cimetidine was the #1 drug linked to theophylline toxicity. One case reported a jump from 15.2 to 24.7 mcg/mL in just 72 hours after starting cimetidine.
- Allopurinol - Used for gout, this drug reduces theophylline clearance by about 20%. Even though that sounds modest, it’s enough to push someone over the edge if they’re already near the top of the safe range. The key? Dose matters. At 300 mg daily, the effect is minimal. But at 600 mg, the risk spikes.
- Erythromycin and Clarithromycin - These antibiotics, often prescribed for lung infections, inhibit CYP3A4 - a secondary pathway for theophylline metabolism. Together, they can reduce clearance by 15-25%. In elderly patients with COPD, this combo is a recipe for ER visits.
- Furosemide - The evidence here is mixed. Some studies show a 10-15% drop in clearance; others show nothing. But because furosemide is commonly used in COPD patients with heart failure, and those patients are already at higher risk for toxicity, many experts recommend caution - and monitoring.

What Happens When Clearance Drops?
The symptoms of theophylline toxicity aren’t subtle. They start with nausea, vomiting, and tremors. Then come headaches, rapid heartbeat, and insomnia. If levels keep rising, you get seizures, cardiac arrhythmias, and sometimes death. The FDA reports about 2,000 emergency room visits each year in the U.S. because of this - and 35% of them are due to drug interactions.Here’s the scary part: many of these cases are preventable. In a 2023 survey of 412 pulmonologists, nearly 80% said they’d seen a serious interaction in the past year. Yet only 37% of those cases had proper dose adjustments or blood level checks. Why? Because the alerts in electronic health records are weak, or absent. Pharmacists often don’t know the patient is on theophylline. And patients? They don’t realize that their new heartburn pill could be dangerous with their asthma med.
Who’s at Highest Risk?
It’s not just about the drugs. It’s about the person.- Older adults - Liver function slows with age. Clearance drops naturally. One study showed elderly patients with heart failure clear theophylline at less than a third the rate of healthy young adults.
- Smokers who quit - Smoking induces CYP1A2. When someone stops, their clearance drops by 30-50% within two weeks. If they’re on theophylline and then quit smoking - without telling their doctor - their levels can skyrocket.
- People with liver disease or heart failure - Both conditions reduce the liver’s ability to process the drug. Clearance can fall from 3 L/h in healthy adults to under 0.5 L/h in severe cases.
- Those on multiple medications - Polypharmacy is the silent killer here. A patient might be on theophylline, allopurinol, furosemide, and an antibiotic. Add cimetidine for heartburn, and you’ve got a perfect storm.
How to Stay Safe
If you’re taking theophylline, here’s what you need to do:- Know your current level. Get a blood test before starting any new medication.
- Check every new prescription. Ask your pharmacist: “Could this interact with theophylline?” Don’t assume they know - many don’t.
- Never start OTC meds without asking. Cimetidine is sold as Tagamet, and it’s in some cold medicines. Famotidine (Pepcid) is safer - it doesn’t affect CYP1A2.
- Monitor for symptoms. If you feel nauseous, shaky, or your heart races after starting a new drug, get your levels checked immediately.
- Don’t quit smoking cold turkey without telling your doctor. If you’re on theophylline, you’ll likely need a dose reduction.
Doctors should follow these steps too:
- Reduce theophylline dose by 25-50% when starting a strong CYP1A2 inhibitor.
- Check serum levels within 48-72 hours after starting or stopping an interacting drug.
- Avoid theophylline altogether if the patient needs long-term fluvoxamine or cimetidine. Use alternatives.
- Use tools like the University of Lausanne’s pharmacokinetic calculator - it factors in age, smoking status, liver function, and interacting drugs to predict clearance.
The Bigger Picture
Theophylline use has dropped by 62% in the U.S. since 2000. But the people still taking it are the most vulnerable - older, sicker, on more meds. And the number of drug-interaction-related ER visits is actually rising. Why? Because the remaining patients are less likely to be monitored by specialists. Primary care doctors may not know the risks. Pharmacists may not be alerted.Some researchers are now exploring low-dose theophylline (100-200 mg daily) for its anti-inflammatory effects in COPD. But in those trials, patients on CYP1A2 inhibitors are automatically excluded. That tells you everything you need to know: the risk is real, predictable, and avoidable.
GlobalData predicts theophylline sales will keep falling 4.7% a year through 2030. But until it’s gone completely, we can’t ignore the danger. The drug isn’t the problem. It’s the lack of awareness.
For the patients still on it - and the doctors prescribing it - the message is clear: know your interactions. Check your levels. Ask the questions. Because when it comes to theophylline, a small mistake can have deadly consequences.
Can I take ibuprofen with theophylline?
Yes, ibuprofen does not significantly affect theophylline metabolism. It doesn’t inhibit CYP1A2 or CYP3A4 in a clinically meaningful way. However, if you’re taking high doses of ibuprofen for long periods - especially with kidney issues - your overall health status may change, which could indirectly affect clearance. Always monitor levels if your condition changes.
Is theophylline still used today?
Yes, but rarely as a first-line treatment. It’s mostly used for severe or refractory asthma, nocturnal COPD symptoms, or in areas where newer inhalers are too expensive. Global use is highest in Asia and Africa, where it accounts for up to 12.4% of COPD maintenance therapy. In the U.S., it’s down to 1.7%, but still responsible for hundreds of toxicity cases each year.
How long does it take for theophylline levels to change after stopping an interacting drug?
It depends on the drug. For CYP1A2 inhibitors like cimetidine or fluvoxamine, clearance begins to recover within 2-3 days after stopping, but full recovery can take 5-7 days. Blood levels may drop slowly, so it’s still important to recheck theophylline levels 48-72 hours after discontinuing the interacting drug to avoid underdosing.
Can I switch from theophylline to a safer alternative?
Yes, and it’s often recommended. Long-acting beta-agonists (like salmeterol or formoterol) and long-acting muscarinic antagonists (like tiotropium) are safer, with fewer interactions and side effects. Inhaled corticosteroids combined with these are now standard for most patients. Theophylline should only be kept if these options aren’t effective or accessible.
Do herbal supplements affect theophylline?
Yes. St. John’s wort can increase clearance, lowering theophylline levels and reducing effectiveness. On the flip side, grapefruit juice and some green tea extracts can inhibit CYP1A2, raising theophylline levels. Always tell your doctor about all supplements - even if you think they’re “natural.”


Coral Bosley
Theophylline is one of those drugs that feels like a relic from the 1970s, but somehow still haunts the ERs of America. I had a cousin on it for years after her asthma diagnosis, and she didn’t even know her heartburn pill could kill her. No one warned her. Not the pharmacist, not the primary care doc. Just a little Tagamet and boom - ICU. We need better alerts, not just for doctors but for patients too.
Steve Hesketh
This is why I tell every elder in my community: don’t take anything new without asking your pharmacist. I’ve seen too many good people lose their way because they trusted a pill without knowing its hidden teeth. Theophylline isn’t the villain - ignorance is. Let’s spread the word like fire in dry grass. Someone’s grandma might be reading this right now. Tell her. Tell her now.
shubham rathee
cimetidine is the real villain here and everyone knows it but no one does anything because big pharma makes more money selling the combo than the warning label. also fluvoxamine is just antidepressant propaganda anyway why are we even using it why not just give them benzos like in the 80s
MAHENDRA MEGHWAL
It is with profound respect for clinical pharmacology that I acknowledge the gravity of this issue. Theophylline’s narrow therapeutic index, coupled with the pervasive use of polypharmacy among geriatric populations, represents a systemic vulnerability in current healthcare delivery. I urge all practitioners to institutionalize mandatory serum level checks prior to initiation of any CYP1A2-modulating agent, particularly in patients with comorbid cardiovascular or hepatic conditions.
Kevin Narvaes
so like... theophylline is basically the crypto of asthma meds? everyone says it's dead but somehow it's still in people's medicine cabinets and someone always gets rug pulled. and why is no one talking about how the FDA just lets this stuff slide? they're too busy approving new weight loss drugs that make you cry in the shower.
Dee Monroe
I’ve spent years working with elderly patients in rural clinics, and I can tell you - the real tragedy isn’t the drug. It’s the silence. No one talks about theophylline anymore. It’s not sexy. It doesn’t have a TikTok trend. But the people who still need it? They’re not asking for innovation. They’re asking for someone to remember them. To check their levels. To ask if they’ve started a new OTC pill. To say, ‘I see you.’ That’s the real treatment here - not the molecule, but the attention.
Sangeeta Isaac
Okay but let’s be real - if you’re still on theophylline in 2025, you’re basically playing Russian roulette with your liver. I had my dad on it for 12 years. He quit smoking cold turkey, didn’t tell his doctor, and woke up vomiting blood. Turns out his levels were at 28. He’s fine now, but I swear if he’d had one alert on his pharmacy app saying ‘DON’T STOP SMOKING WITHOUT TELLING YOUR DOCTOR,’ he wouldn’t have ended up in the ER with a cardiac monitor on his chest. Why does this still exist? Why aren’t we banning this like lead paint?
Alex Carletti Gouvea
Look, I get it. Theophylline’s old. But if you’re in a country where a $120 inhaler is a luxury, this is the only thing keeping people alive. Stop acting like it’s some American problem. In Nigeria, India, Bangladesh - this drug is a lifeline. We don’t have fancy EHR alerts or pharmacists on every corner. We have a nurse who checks levels once a month. That’s not negligence. That’s survival. Stop judging. Start funding.
Philip Williams
Thank you for this comprehensive overview. I would like to emphasize the critical importance of pharmacist-led medication reconciliation in high-risk populations. A 2022 study in the Journal of Clinical Pharmacy and Therapeutics demonstrated that structured pharmacist interventions reduced theophylline toxicity incidents by 63% in patients over 65. This is not a physician-only issue. It is a team-based care imperative. Institutions must empower pharmacists with direct access to patient records and clinical decision support tools tailored to polypharmacy risks.
Ben McKibbin
It’s wild how a drug that’s been around since 1888 still has this much power to kill - and yet we treat it like a footnote. We’ve got AI that can predict cancer from a chest X-ray, but we can’t build a simple alert that says, ‘This patient is on theophylline. Do not prescribe cimetidine.’ It’s not a technical problem. It’s a moral one. We’ve normalized complacency in drug safety. The real toxicity isn’t in the bloodstream - it’s in our indifference.
Melanie Pearson
While the article presents a compelling narrative, it fails to acknowledge the broader context of global healthcare disparities. In the United States, theophylline use is declining because of overregulation, litigation aversion, and pharmaceutical marketing dominance. In contrast, in developing nations, the drug remains in use not due to negligence, but due to necessity. To frame this as an American medical failure is not only inaccurate - it is ethically irresponsible. The solution is not to eliminate theophylline, but to ensure equitable access to monitoring tools worldwide.