Polypharmacy Risk Assessment Tool
Medication Risk Assessment
Enter the number of regular medications you take (prescription, OTC, vitamins, supplements)
Your Risk Assessment
Common Side Effects
- 1 Dizziness or balance issues
- 2 Fatigue or low energy
- 3 Confusion or memory issues
- 4 Sleep disturbances
Action Steps
If you're taking 5+ medications, ask your healthcare provider about:
- Medication review - Ask to go through all your medications
- Deprescribing - Discuss which medications might no longer be needed
- Beers Criteria - Check if you're taking medications risky for older adults
More than 40% of adults over 65 in the U.S. take five or more medications every day. That’s not just common-it’s dangerous. Taking multiple drugs might seem necessary when you’re managing heart disease, diabetes, arthritis, and high blood pressure all at once. But the more pills you swallow, the higher your chance of falling, getting hospitalized, or even dying from something preventable. This isn’t theoretical. It’s happening to real people right now.
What Exactly Is Polypharmacy?
Polypharmacy isn’t just having a few prescriptions. It’s defined as taking five or more medications regularly. That includes prescription drugs, over-the-counter painkillers, vitamins, and herbal supplements. It’s not always bad-sometimes you need all of them. But too often, medications are added without stopping others. A patient gets a new pill for sleep, then another for the dizziness it causes, then another for the stomach upset from that one. This is called a medication cascade, and it accounts for 30-40% of unnecessary prescriptions in older adults.
Doctors aren’t being careless. They’re responding to symptoms, guidelines, and time constraints. But when you’re juggling 10+ pills, no one is looking at the whole picture. The American Geriatrics Society says 91% of adverse drug events in seniors are tied to polypharmacy. That’s not a coincidence. It’s a system failure.
How More Medications Lead to More Side Effects
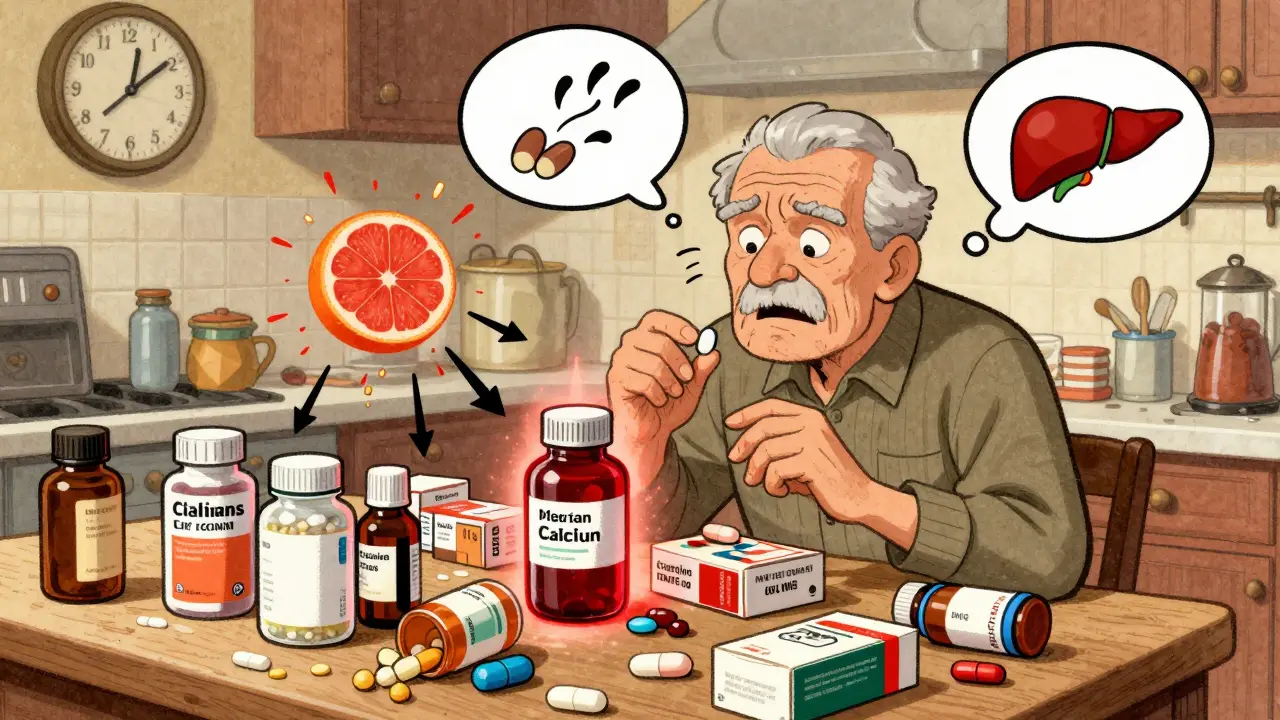
Your body doesn’t handle drugs the same way when you’re 75 as it did when you were 45. Liver and kidney function slow down. Your brain becomes more sensitive to certain chemicals. And when you take multiple drugs, they don’t just sit there-they interact.
Here’s how it breaks down:
- Drug-drug interactions: One medication changes how another is absorbed, broken down, or eliminated. For example, combining a blood thinner like warfarin with an anti-inflammatory like ibuprofen can cause dangerous bleeding.
- Drug-disease interactions: A drug meant for one condition can make another worse. Anticholinergic drugs (used for overactive bladder or allergies) can worsen dementia symptoms.
- Side effect stacking: Each pill has its own side effects. Take five pills, each with a 10% chance of causing dizziness, and your total risk isn’t 10%-it’s closer to 40%. That’s why falls become so common.
Studies show that people taking seven or more medications are 42% more likely to have trouble walking or balancing. One in three seniors on multiple drugs reports falling in the past year. And falls don’t just mean bruises-they mean broken hips, long hospital stays, and loss of independence.
The Real Cost: More Than Just Money
It’s not just about health-it’s about life. A 2022 Medicare survey found that 48% of people on five or more medications believed they had a side effect from one of them. Nearly 30% said they cut back on social activities because they felt too tired, dizzy, or confused.
One woman, Martha, 72, told UCI Health: “I was taking 17 pills a day. I couldn’t remember which ones I’d taken. I felt like a pharmacy on legs.”
Then there’s the cost. People taking five to nine medications spend an average of $317 a month. Those on ten or more pay over $5,200 a year. That’s more than many retirees make in Social Security. Robert, 68, said he had to choose between his heart medication and food. He’s not alone.
Non-adherence is rampant. A 2021 study found patients on ten+ medications were 3.2 times more likely to skip doses. Why? Complexity (58%), side effects (47%), and cost (65%). When you’re overwhelmed, you stop taking the pills. That’s when things get worse.

When Polypharmacy Actually Helps
Not all multiple medications are bad. Sometimes, they save lives. For someone recovering from a heart attack, taking a beta blocker, statin, aspirin, and ACE inhibitor together can cut the risk of another heart attack by 50-60%. That’s appropriate polypharmacy-carefully chosen, evidence-based, and monitored.
The problem isn’t the number. It’s the lack of review. A 2020 study showed that when doctors took time to go through every pill a patient was taking, they found at least one unnecessary or harmful medication in 70% of cases. That’s not rare. That’s the norm.
Deprescribing: The Quiet Revolution
There’s a growing movement called deprescribing-the planned, safe reduction or stopping of medications that aren’t helping or are doing more harm than good. It’s not about cutting pills just because you’re on too many. It’s about asking: “Does this still serve a purpose?”
Here’s how it works:
- Review everything: Include prescriptions, OTC drugs, vitamins, and supplements. Many patients don’t tell their doctors about aspirin or melatonin-but those can interact dangerously.
- Use the Beers Criteria: This is a list of medications that are risky for older adults, like benzodiazepines for sleep or NSAIDs for pain. These drugs are responsible for 45% of inappropriate prescribing in seniors.
- Taper slowly: Don’t stop cold turkey. Withdrawal can cause rebound symptoms. A 3-6 month plan is typical.
- Monitor closely: Watch for changes in mood, balance, sleep, or energy. If symptoms improve, you’re likely on the right track.
One patient on Reddit, described by a nurse, was taking 12 medications. After deprescribing three that weren’t needed, her dizziness and confusion vanished. She started walking again. She stopped falling.

Who’s Responsible?
It’s not just the patient’s job to manage this. Doctors, pharmacists, and insurers all play a role.
The American Society of Health-System Pharmacists says physicians should review all medications for anyone on five or more drugs. The FDA approved a tool called MedWise in 2022 that flags dangerous combinations-and it reduced high-risk pairings by 37% in early trials.
Medicare now requires medication reviews for people on eight or more drugs. But only 28% of primary care doctors say they have good systems to handle complex regimens. And only 12% of medical schools teach polypharmacy as a formal topic.
That’s the gap. We have the tools. We have the data. But we don’t have the systems.
What You Can Do Right Now
If you or a loved one is on five or more medications, here’s what to do:
- Make a complete list of everything you take, including doses and why you take them.
- Bring it to your next appointment. Ask: “Is this still necessary?”
- Ask specifically about anticholinergics, benzodiazepines, and NSAIDs. These are the most common culprits.
- Don’t be afraid to say: “I’m having side effects. Can we try reducing something?”
- Ask if a pharmacist can do a medication review. Many pharmacies offer this for free.
It’s not about taking fewer pills for the sake of it. It’s about taking only what you truly need. One woman told her doctor she felt better after stopping a cholesterol pill she’d been on for 15 years-she’d never had a heart problem. He said, “I’m glad you brought it up. I didn’t realize you were still on it.”
That’s the problem. No one’s keeping track.
The Future Is Clear
Without action, polypharmacy will cause 40% more adverse drug events and $127 billion in extra healthcare costs by 2035. But change is possible. The Choosing Wisely campaign, launched in 2021, cut inappropriate prescribing by 22% in participating clinics. That’s proof it can work.
It’s time to stop thinking of pills as solutions and start seeing them as risks. Every medication you take has a cost-financial, physical, and emotional. The goal isn’t to take less. It’s to take only what matters.
Your body isn’t a pharmacy. It’s a living system. Treat it like one.








Nicholas Gabriel
I’ve seen this firsthand with my dad-17 pills a day, and he couldn’t tell you what half of them were for. He was dizzy all the time, kept falling, and his doctor never asked if any could be cut. Then we brought the whole list to a geriatric pharmacist, and three were outright dangerous. He’s been walking without a cane for 8 months now. It’s not magic-it’s just common sense. Why do we treat pills like candy? We wouldn’t give someone five different painkillers without checking interactions, so why do it with chronic meds? Someone needs to audit these regimens like they audit bank accounts. It’s insane we don’t have mandatory annual med reviews for seniors on five+ drugs. This isn’t just medical-it’s a civil rights issue. People deserve to live, not just survive in a pill fog.
Cheryl Griffith
My grandma took 11 pills. She stopped eating because she was too tired. She stopped talking because she was too confused. We thought it was just aging-until we stopped three of them. The change was like flipping a switch. She remembered my name again. She laughed at my dumb jokes. She started gardening. It wasn’t that the meds were ‘bad.’ It’s that no one was looking at the whole picture. Doctors treat symptoms like puzzle pieces, but they forget they’re painting a portrait. And the portrait was getting darker. I wish more people knew how easy it is to fix this. Just ask: ‘What if we tried taking this one away?’ It’s not risky. Not doing it is the risk.
swarnima singh
they said its just aging but its not... its the pharmasuticals... they want you sick forever... they dont want you to get well... they make money off your confusion... they give you pills for the side effects of other pills... its a cycle... a trap... the system is designed to keep you dependent... i saw my aunt take 14 pills... she forgot how to walk... then she died... they called it natural causes... but she was fine before the meds... the truth is buried under white coats and prescriptions... dont trust them... they are not your friends...
Isabella Reid
I’m a nurse, and I’ve watched this play out for 20 years. The saddest part? Most patients don’t even know they’re on meds they don’t need. They think if the doctor wrote it, it’s sacred. But here’s the thing: deprescribing isn’t about taking away care-it’s about restoring dignity. One woman I worked with was on gabapentin for ‘nerve pain’ she didn’t have. She was on it for 8 years because someone else started it. We tapered her off. She started reading again. She started going to book club. She cried and said, ‘I didn’t know I could feel like this.’ That’s the real cost of polypharmacy-not just falls or ER visits. It’s stolen joy. We need more pharmacists in primary care. Not just for scripts. For sanity.
Jody Fahrenkrug
My mom’s on 8 meds. I help her with her pill organizer every Sunday. It’s a whole thing. I get it-she needs them. But I also get that she’s tired all the time, and her balance is off. I asked her doctor if any could be cut. He said, ‘We’ll look at it next visit.’ Next visit is in 6 months. I’m not mad-I’m just... tired. It shouldn’t be this hard to get someone to look at a list. I printed it out, color-coded it, put sticky notes on the ones that might be risky. He didn’t even glance at it. Just nodded. I’m starting to think the system isn’t broken. It’s just designed to ignore this.
Kasey Summerer
So let me get this straight… we’ve got a population of seniors drowning in pills, and the solution is… more paperwork? 😂
Doctors get 12 minutes per patient. They’re not evil-they’re just drowning in their own system.
But hey, at least we’ve got an FDA-approved app to flag bad combos… while the same people who made the problem are still selling the pills.
Meanwhile, my 74-year-old neighbor just stopped her statin because she couldn’t afford it. Now she’s on a ‘natural remedy’ that costs $80 a bottle and says ‘cures everything’ on the label.
At this point, I’m just waiting for someone to patent a pill that tells you which other pills to stop. 😅
kanchan tiwari
THEY KNOW. THEY KNOW WHAT THEY’RE DOING. EVERY SINGLE PILL IS A TRAP. THE PHARMA COMPANIES PAY DOCTORS TO KEEP YOU ON MEDS. THEY OWN THE GUIDELINES. THEY OWN THE STUDIES. THEY OWN THE FDA. THEY WANT YOU DEPENDENT. THEY WANT YOU AFRAID. THEY WANT YOU TO BELIEVE YOU CAN’T LIVE WITHOUT 10 PILLS A DAY. THAT WOMAN WHO TOOK 17 PILLS? SHE WAS A TEST SUBJECT. THE NURSE WHO HELPED HER? SHE WAS PAID. THE REDDIT POST? A STAGED CAMPAIGN TO MAKE YOU FEEL SAFE. THEY’RE STILL WATCHING. THEY’RE STILL PROFITING. YOU THINK YOU’RE IN CONTROL? YOU’RE A NUMBER IN A DATABASE. YOUR BODY IS A MARKET. YOU’RE NOT A PERSON. YOU’RE A REVENUE STREAM. STOP TAKING THE PILLS. STOP TRUSTING THE SYSTEM. THE TRUTH IS OUT THERE… BUT THEY’RE ERASING IT.
Bobbi-Marie Nova
My aunt cut down from 12 to 5 meds last year. She’s now hiking with her grandkids. No more naps at 3 p.m. No more confusion at family dinners. She didn’t ‘get better’-she just stopped being drugged into a zombie. The doctor didn’t even charge her for the med review. Free. At a pharmacy. That’s it. No magic. Just someone taking a minute to ask, ‘Do you still need this?’ I wish every senior had someone to do that for them. And I wish doctors got paid for doing it. Not just for writing more scripts. 🤍