Ever walked into a doctor’s office and realized you forgot which meds you’re taking? You’re not alone. Over 50% of adults in the U.S. take at least one prescription drug, and nearly 20% take five or more. That’s where a medication review appointment is a structured clinical consultation where healthcare professionals evaluate your complete medication regimen to ensure it’s safe and effective comes in. This isn’t just a chat-it’s a critical safety check. Skipping it could mean dangerous drug interactions, wasted money on unnecessary pills, or even hospital visits. Let’s break down exactly how to prepare so you walk in ready to go.
What’s a Medication Review Appointment?
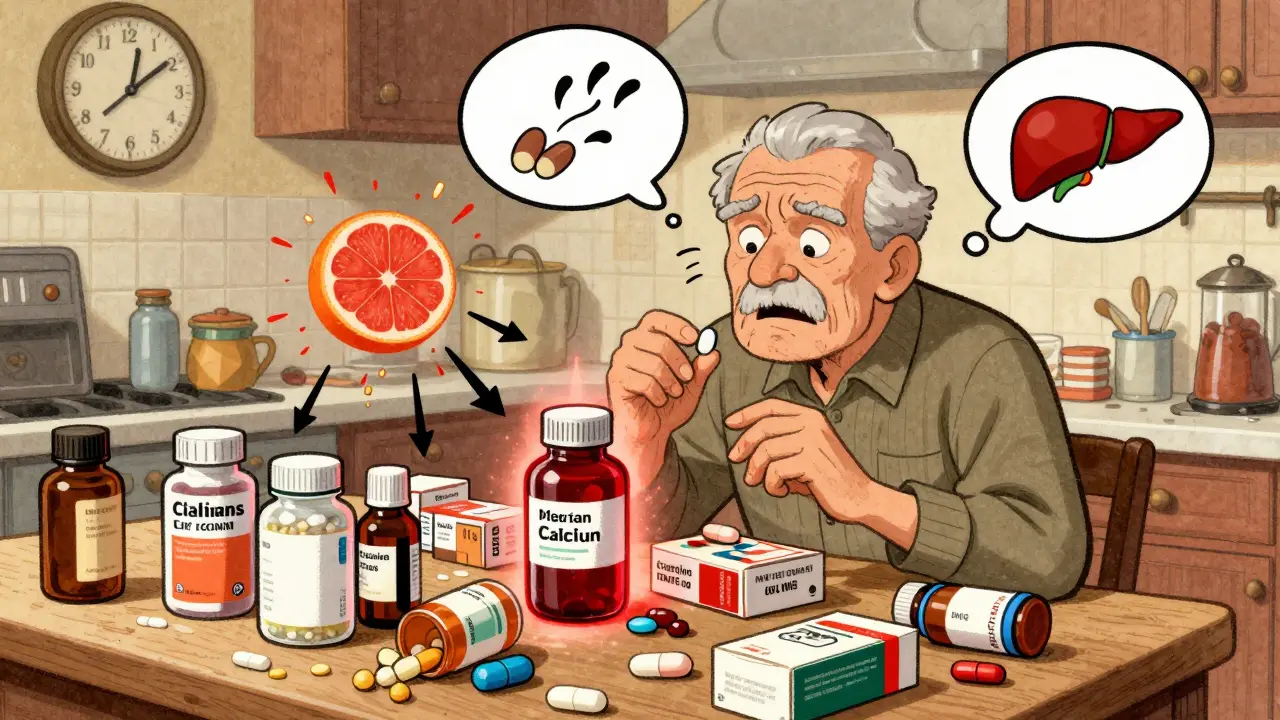
A medication review isn’t optional-it’s becoming mandatory. Doctors and pharmacists now require these appointments for patients on multiple medications. Why? Because polypharmacy the use of five or more medications regularly, which increases the risk of adverse drug reactions is a growing problem. The Northern Health and Social Services Board a healthcare authority in Ireland found that patients taking four or more medications have a 50% higher chance of dangerous side effects. During the review, your provider will check if each drug is still necessary, if doses are correct, and if there are hidden risks. It’s like a full tune-up for your medicine cabinet.
Step 1: List Every Single Medication
Don’t just guess-write everything down. Include:
- Prescription drugs (name, dose, why you take them, who prescribed them)
- Over-the-counter meds like ibuprofen or allergy pills
- Vitamins, supplements, and herbal remedies (even garlic pills or chamomile tea)
- Topical creams or eye drops
Godiva Group Practice NHS a UK-based healthcare provider stresses this: patients who forget OTC items often get caught off guard. For example, taking a common painkiller like aspirin with blood thinners could cause dangerous bleeding. Your list should be detailed. If you’re unsure about a medication’s name, check the bottle-no guessing allowed. The Health Innovation Network a global health improvement organization found that 30% of medication errors happen because patients couldn’t name their own drugs.
Step 2: Bring the Actual Bottles
Yes, every single one. Even if you have a list, the pharmacist needs to see the physical bottles. Why? Labels can be misread-a pill bottle for “Lisinopril 10mg” might say “Lisinopril 5mg” if you’re not careful. The Northern Health and Social Services Board calls this “the most reliable way to verify dosages.” They also check expiration dates. Expired antibiotics or insulin can be useless or harmful. For instance, a 2023 study showed 15% of patients had outdated medications in their homes. Bring your supplements too-even if they’re just “for health.” Some herbal teas interact with heart medications. Your provider needs to see everything.

Step 3: Prepare Your Questions
Don’t wait until the appointment to think of questions. Write them down. Examples:
- “Is this medication still necessary for me?” (Some drugs lose effectiveness over time.)
- “Are there cheaper alternatives?” (Many medications have generic versions.)
- “What side effects should I watch for?” (This helps catch issues early.)
- “Do these pills interact with my other meds?” (Critical for polypharmacy patients.)
Dr. Antoine Geffrard a specialist at RMS Consultations in Southfield, MI says patients who ask questions get better outcomes. In fact, those who discussed medication risks during reviews were 40% less likely to experience adverse events. Don’t be shy-your pharmacist is there to help. If you’re unsure what to ask, just say, “I want to make sure this is the best plan for me.”
Step 4: Telehealth Prep (If Applicable)
More reviews happen over video now. If yours is virtual, extra prep is needed. First, gather all your medications in one place-you’ll need to show them on camera. Test your internet connection and camera beforehand. The Patient Safety Wisconsin a U.S. patient safety organization warns that 25% of telehealth medication reviews fail because patients can’t show bottles clearly. For chronic conditions like Parkinson’s disease, Parkinson’s UK a UK-based charity for Parkinson’s patients stresses timing precision. If you take levodopa for Parkinson’s, know the exact time of your last dose-delayed timing can cause dangerous symptoms. Have a notebook ready to jot down changes during the call.

Step 5: What Happens During the Appointment?
The review usually takes 20-45 minutes. Your provider will:
- Check your medication list against the bottles you brought
- Ask about side effects you’ve noticed (even small ones like dizziness or nausea)
- Discuss if any drugs can be stopped, changed, or combined
- Explain the risks and benefits of each medication
clinical pharmacist a healthcare professional specialized in medication management may lead the review instead of your doctor. This is common-pharmacists spend extra time on drug interactions. For example, they’ll spot if you’re taking a blood pressure med that’s less effective when combined with a common antacid. The Health Innovation Network found that pharmacist-led reviews reduce medication errors by 35%. You’ll leave with a clear action plan-whether it’s stopping a pill, switching to a generic, or adjusting doses.
Why Skipping This Step Is Risky
Ignoring a medication review isn’t just careless-it’s dangerous. The Godiva Group Practice NHS has a strict policy: if you don’t respond to three reminders for a review, they stop prescribing new medications. This isn’t bureaucracy-it’s safety. A 2022 study showed 60% of hospital admissions for older adults were due to medication errors that could have been caught in a review. For example, taking too much acetaminophen (from both painkillers and cold meds) can cause liver failure. Or mixing blood thinners with certain antibiotics could lead to uncontrolled bleeding. These aren’t rare scenarios-they’re everyday risks for polypharmacy patients. Don’t gamble with your health.
What if I can’t get to the appointment?
Many clinics offer home visits or telehealth options. The Northern Health and Social Services Board states that patients with mobility issues can request home visits when scheduling. For telehealth, make sure you have all medications ready to show on camera and a stable internet connection. If you’re unable to attend, call the clinic-they’ll help reschedule or adjust the format.
Can I bring a friend or family member?
Yes! Many patients find it helpful to have someone else there to take notes or ask questions. The Health Innovation Network encourages this, especially for older adults or those with cognitive challenges. Just let the clinic know in advance so they can accommodate extra people.
What if I don’t know why I take a certain medication?
Don’t worry-this is common. Bring the pill bottle anyway-your provider can look up the prescription history. They’ll explain why it was prescribed and whether it’s still needed. The Godiva Group Practice NHS reports that 40% of patients don’t know the purpose of all their meds, but the review is designed to clarify this.
Do I need to prepare differently for a pharmacist-led review?
No-the same prep steps apply. Pharmacists specialize in medication safety, so they’ll focus on drug interactions, dosing accuracy, and side effects. They may ask more detailed questions about how you take your meds (e.g., “Do you take your blood pressure pill with food?”). Bring all bottles and your list-they’ll use it to check for hidden risks.
How often should I have a medication review?
Annual reviews are standard for most patients. But if you’re on five or more medications, have chronic conditions like diabetes or heart disease, or notice new side effects, you may need reviews every 6 months. The Northern Health and Social Services Board says high-risk patients should have reviews as often as needed-never wait for symptoms to get worse.







Danielle Vila
Big Pharma is behind this medication review push. They want us to think we need these appointments to stay safe, but it's all a scheme to sell more drugs. I've been on my meds for a decade without issues, and now they're trying to make me think I'm at risk. They're tracking our data through these apps-privacy violations everywhere. Plus, they hide the real side effects. I read a study where 80% of medications have dangerous side effects they don't mention. They're controlling us. Also, check out my blog for the real truth. 😏 And let's not forget about the FDA's close ties to pharmaceutical companies-this is all a coordinated effort to keep us docile and dependent. The government is in on it too. They want us to believe we need these reviews, but really it's about profit. Every time you take a pill, they're making money. They're not concerned about your health-they're in it for the cash. You should do your own research instead of trusting these 'experts'. Don't fall for their lies!
Thorben Westerhuys
OMG! This is so important!! I can't believe how many people skip this!! My brother had a bad reaction because he didn't do a review!! He was on 5 meds and didn't know about the interaction!! It's a matter of life and death!! You HAVE to do this!! Seriously, my brother almost died because he didn't check his meds. It was a combination of blood thinners and an OTC painkiller. The doctor said it could have been fatal. I'm so grateful he went to the review. Everyone needs to do this. Don't wait until it's too late. It's not just about taking pills-it's about staying alive. Please, take this seriously. Your life depends on it!!
Laissa Peixoto
Medication reviews are a profound moment of self-reflection on our relationship with pharmaceuticals. It's not just about checking boxes-it's about understanding how each pill fits into the tapestry of our health. Many people view meds as a solution, but they're often part of a larger system. We should consider not just the 'what' but the 'why' behind each prescription. This process invites us to question our reliance on drugs and consider holistic approaches. However, I must acknowledge the systemic issues in healthcare that make these reviews necessary in the first place. It's a paradox: we need them, but they're a symptom of a broken system. Still, for now, they're crucial for safety. Understanding the 'why' behind each medication can empower patients to make informed decisions. It's not about blindly following orders but engaging with our healthcare providers. This review is an opportunity to take control of our health journey. We should embrace it as a tool for better health outcomes. Ultimately, it's about ensuring that our medications align with our overall wellness goals.
Matthew Morales
Hey, this is super useful! 😊 I always forget to bring my bottles to the doc. Thanks for the reminder! I'll make sure to check all my meds next time. Also, the part about OTC meds is key-like I had no idea my allergy pills could interact with my heart med. Duh! 😅 Gotta be careful with that. Thanks again! I just realized I've been taking ibuprofen with my blood pressure meds and didn't know it could cause issues. I'll definitely bring all my bottles next time. Also, the vitamins I take-like fish oil and vitamin D-should be included. This guide really opened my eyes. I've been taking meds for years but never thought to list everything. Thanks for sharing this. It's such a simple step but makes a huge difference. I'll be more careful from now on. Really appreciate the advice!
Dr. Sara Harowitz
Americans are so careless with their medications! It's no wonder there are so many issues. I've seen this time and again-people don't take their reviews seriously. It's embarrassing! You need to be disciplined and follow the guidelines precisely. There's no room for error here. If you can't even list your meds properly, you shouldn't be taking them at all. This is why the U.S. healthcare system is failing-because of people like you who don't take responsibility. Get your act together! I've treated patients who ignore the review process and end up in the ER. It's preventable. You think you know your meds, but you don't. This isn't complicated-just list them and be honest. Stop being lazy and take your health seriously. The system is broken because of people like you. If you can't follow basic instructions, you shouldn't be on medication. It's that simple.
Brendan Ferguson
Medication reviews are a great opportunity to ensure your treatment is safe and effective. I've worked with many patients who thought they knew their meds, but the review uncovered hidden interactions. It's not about being told what to do-it's about collaboration. Pharmacists and doctors want to help you, not control you. Taking a few minutes to prepare can prevent serious issues. Trust the process and be honest about your meds-it's the best way to stay healthy. I've seen firsthand how these reviews save lives. A patient of mine was on four medications that interacted dangerously, but the review caught it. It's not just about checking boxes; it's about understanding your body's needs. Everyone should take this seriously. Don't be afraid to ask questions-your healthcare team is there for you. This is a chance to optimize your health, not a burden. Embrace it as part of your wellness routine. It's simple, effective, and crucial for your safety.
Johanna Pan
This guide is really helpful! 🌍 I love how it covers all the bases. I'm from a country where medication reviews aren't common, so this is eye-opening. Always good to check in with your meds. It's easy to forget about OTC stuff, but it's so important. Thanks for sharing this-hope more people see it! 😊 I've never had a medication review before, but after reading this, I realize how crucial it is. I take several supplements and OTC meds, and I didn't know they could interact. This is such important information for everyone. I'll definitely prepare my list and bottles for my next appointment. It's amazing how much we can learn from these reviews. I'm so glad I came across this. It's a simple step that can prevent so many problems. Thank you for making it so clear and accessible. Everyone should do this-it's a small effort for big rewards.
Jenna Elliott
Medication reviews are mandatory. Period.
Pamela Power
Let's be real-most people can't even handle a simple medication review. They skip it because they're lazy or ignorant. I've had to deal with so many patients who don't know their own meds. It's a disaster waiting to happen. If you're not prepared, you shouldn't be taking any prescription drugs. This isn't rocket science-just list your pills and know why you're taking them. If you can't do that, you're a liability to yourself and others. I've seen countless cases where patients ignore this step and end up in the hospital. It's not complicated. You have a list of medications. You know why you take them. If you can't manage that, you shouldn't be on medication. It's simple: prepare properly or don't take the meds. No excuses. This is basic healthcare responsibility. If you can't do this, you're putting yourself and others at risk. Period.