Every year, more than 36 million older adults in the U.S. fall-and nearly 32,000 of them die from those falls. The CDC calls this a public health crisis. But here’s the uncomfortable truth: many of these falls aren’t just bad luck. They’re often triggered by medications meant to help, not hurt. Sedating drugs like benzodiazepines, opioids, antidepressants, and muscle relaxants are commonly prescribed to manage pain, anxiety, or insomnia in older adults. But they don’t just calm the mind-they slow reaction time, blur vision, and throw off balance. And when someone’s already at risk for falling, these drugs can turn a simple trip to the bathroom into a life-changing injury.
Which Medications Are the Biggest Culprits?
Not all sedating medications carry the same risk. Some are far more dangerous than others when it comes to falls. The list of Fall Risk Increasing Drugs (FRIDs) includes anticonvulsants, antidepressants, antipsychotics, benzodiazepines, sedatives, hypnotics, opioids, and even some blood pressure pills. But among these, a few stand out as especially risky.Benzodiazepines like diazepam (Valium) and lorazepam (Ativan) are classic offenders. They’re often prescribed for anxiety or sleep, but they linger in the body longer as we age, building up and causing drowsiness that lasts into the next day. One study found that people taking these drugs were 60% more likely to fall than those who weren’t.
Opioids-even low-dose ones like tramadol-are another major concern. They don’t just mask pain; they cloud thinking and make you feel unsteady on your feet. The risk spikes when opioids are combined with other sedatives. A 2023 Mayo Clinic analysis showed that patients taking two or more sedating medications had more than double the fall risk of those on just one.
Antidepressants, especially tricyclics like amitriptyline, are surprisingly common in older adults and carry a hidden danger. Their sedating side effects aren’t always obvious to patients or even doctors. One 2022 study found that 44% of older adults taking these drugs reported feeling dizzy or unsteady, but only 12% told their doctor.
And then there’s baclofen, a muscle relaxant often used for back pain or spasticity. It’s one of the highest-risk medications in its class, with studies showing it increases fall risk more than any other muscle relaxant. Yet it’s still frequently prescribed without proper monitoring.
How Many Medications Are Too Many?
It’s not just about which drugs you take-it’s about how many. Taking three or more medications at once is called polypharmacy, and it’s one of the strongest predictors of falling in older adults. Each additional drug adds risk, not just from its own side effects, but from how it interacts with others.Imagine someone on a blood pressure pill, a sleep aid, an antidepressant, and a painkiller. Individually, each might be fine. Together? They create a perfect storm: low blood pressure when standing, dizziness from the sleep aid, slowed reflexes from the painkiller, and confusion from the antidepressant. The result? A stumble that leads to a hip fracture.
Research from the CDC shows that people taking five or more medications have a 50% higher chance of falling than those on one or two. And the risk doesn’t stop at the pill bottle. These drugs can interact with supplements, over-the-counter cold meds, or even grapefruit juice-making things even more unpredictable.
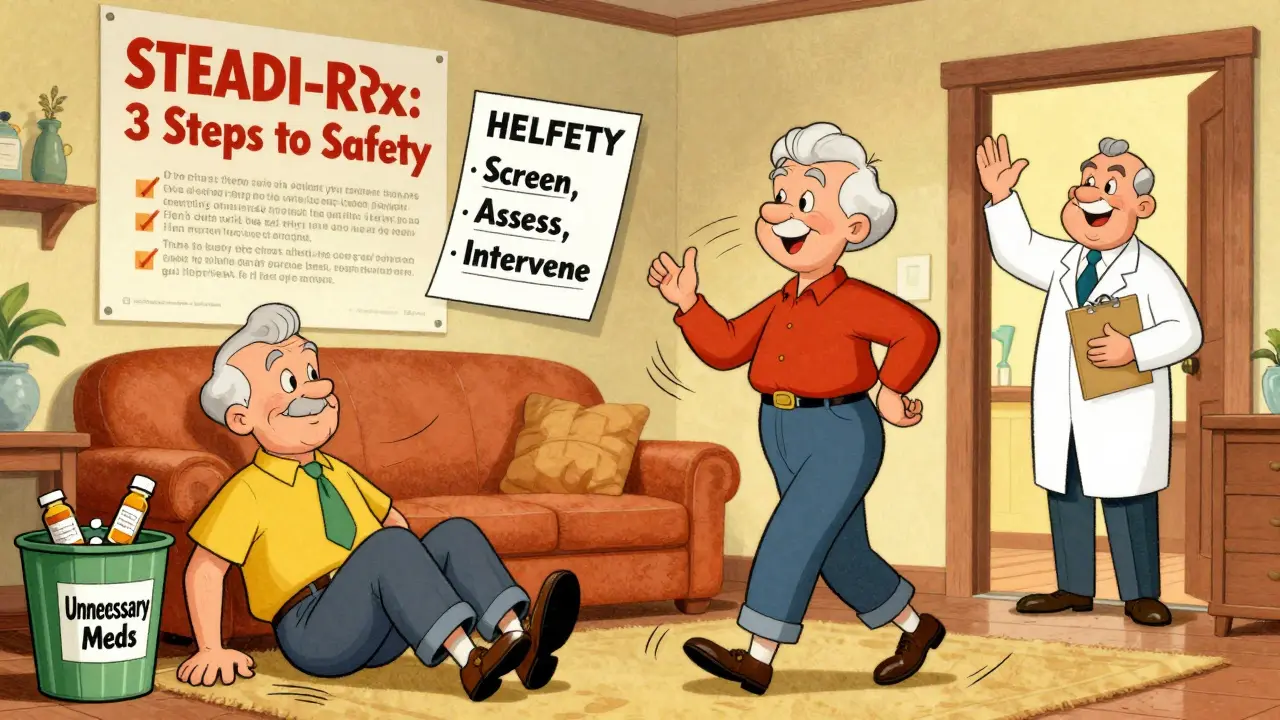
The STEADI-Rx Model: A Proven Way Forward
There’s a solution that’s working in pharmacies across the country: STEADI-Rx. Developed by the CDC and the University of North Carolina, it’s not a new drug or gadget. It’s a simple, three-step process designed to stop medication-related falls before they happen.Step 1: Screen. Every older adult should be asked: Have you fallen in the past year? Do you feel unsteady? Do you worry about falling? That’s it. No fancy tests. Just a few clear questions.
Step 2: Assess. If the answer is yes, a pharmacist or clinician reviews every medication-not just prescriptions, but supplements and OTC drugs too. They look for FRIDs, check for interactions, and note dose levels. They ask: Is this still necessary? Is there a safer alternative?
Step 3: Intervene. This is where real change happens. In 75% of cases reviewed under STEADI-Rx, the solution wasn’t adding a new drug-it was switching or stopping one. Replacing a benzodiazepine with non-drug sleep therapy. Switching from an opioid to acetaminophen with physical therapy. Stopping an unnecessary antipsychotic.
Pharmacists play a key role here. They use a Provider Consult Form to clearly explain risks and suggest alternatives to the prescribing doctor. In one pilot program, 89% of prescribers accepted the pharmacist’s recommendation. And when they did, falls dropped by 30% over six months.

Exercise Isn’t Just Good for You-It’s a Shield Against Falls
Medication review alone helps. But it works even better when paired with movement. The U.S. Preventive Services Task Force and the American Geriatrics Society both agree: exercise is one of the most effective ways to prevent falls.Balance training, strength exercises, and walking programs don’t just build muscle-they retrain the brain to react faster, stabilize the body, and recover from a stumble. A Cochrane review found that structured exercise programs reduced falls by 15-29%. Even more striking: they cut fractures by 61% and medical visits for falls by 43%.
What kind of exercise? You don’t need a gym. Tai Chi, seated leg lifts, heel-to-toe walking, and standing on one foot (with support) are all proven. The key is consistency: 30 to 90 minutes, one to three times a week, for at least 12 weeks. That’s not a lot of time-but it’s enough to make a life-saving difference.
What About Vitamin D?
You’ve probably heard that vitamin D helps prevent falls. The truth? It’s complicated. The U.S. Preventive Services Task Force recommends 800 IU daily for older adults. But a major Cochrane review found no clear benefit. Why the difference?It likely depends on whether someone is deficient. If your vitamin D level is low (under 20 ng/mL), supplementation can help. But if you’re already getting enough sunlight or eating fortified foods, extra pills won’t make you safer. The best approach? Test the level first. Don’t just give supplements blindly.
Why Don’t More Doctors Do This?
You’d think this would be standard care by now. But it’s not. Many primary care doctors are overwhelmed. A 2022 survey by the American Society of Health-System Pharmacists found that 82% of pharmacists believe medication reviews reduce falls-but only 45% have enough time to do them properly.Prescribers often hesitate to stop medications because they fear withdrawal, worsening symptoms, or patient pushback. One patient on Reddit shared that after switching from diazepam to CBT for insomnia, her nighttime falls stopped completely. But another said her doctor refused to reduce her opioids, saying, “I don’t want you to go back to pain.”
And reimbursement is a barrier. Medicare pays for medication therapy management-but only if the pharmacist is recognized as a provider, which varies by state. Many pharmacies don’t have the staffing or training to run these programs.
What Can You Do?
If you or a loved one is taking one or more sedating medications, here’s what to ask:- Is this medication still necessary? Could it be stopped?
- Is there a non-sedating alternative?
- Could the dose be lowered?
- Have we checked for interactions with other drugs or supplements?
- Can we add balance exercises to our routine?
Bring a full list of everything you take-including vitamins, herbs, and OTC drugs-to your next appointment. Ask for a pharmacist consult. Most community pharmacies now offer free medication reviews. Don’t wait for a fall to happen. Prevention starts with a conversation.
What’s Next?
The future of fall prevention is getting smarter. In 2023, the CDC updated its STEADI toolkit to include specific deprescribing guides for benzodiazepines and opioids. More pharmacists are getting certified in geriatric pharmacotherapy-over 1,200 now hold the credential. AI tools are being tested to flag dangerous drug combinations before they’re even prescribed.But none of that matters if we don’t act now. With over 80 million Americans expected to be over 65 by 2040, the need for smarter medication use isn’t coming-it’s already here.
Can stopping a sedating medication really prevent falls?
Yes, absolutely. Studies show that removing or replacing a sedating medication can reduce fall risk by up to 30%. For example, switching from a benzodiazepine to cognitive behavioral therapy for insomnia led to zero nighttime falls in one patient over six months. The key is doing it safely-with medical supervision to manage withdrawal or symptom recurrence.
Which medications are most likely to cause falls in older adults?
The highest-risk medications include benzodiazepines (like Valium), opioids (especially strong or combined doses), tricyclic antidepressants (like amitriptyline), muscle relaxants (particularly baclofen), and sedative-hypnotics (like zolpidem). These drugs slow reaction time, cause dizziness, and impair balance. The risk increases when two or more are taken together.
How often should older adults have their medications reviewed?
At least once a year, and more often if they’ve fallen, changed doctors, or started a new medication. Anyone taking three or more prescriptions should have a formal medication review with a pharmacist or geriatrician. The CDC’s STEADI-Rx model recommends reviews after any fall, hospitalization, or change in health status.
Is it safe to stop a sedating medication on my own?
No. Stopping medications like benzodiazepines or opioids suddenly can cause dangerous withdrawal symptoms, including seizures, severe anxiety, or rebound insomnia. Always work with a doctor or pharmacist to create a slow, supervised tapering plan. Most safe reductions take weeks to months.
Do I need to take vitamin D to prevent falls?
Only if you’re deficient. If your vitamin D level is below 20 ng/mL, taking 800-1,000 IU daily may help. But if your level is normal, extra supplements won’t reduce fall risk. Get tested before starting-don’t guess. The best protection is still exercise and medication review.
Can pharmacists help with medication reviews?
Yes, and they’re often the best people to do it. Community pharmacists can review all your medications-including OTC drugs and supplements-and identify risks you might miss. Many offer free medication therapy management services. Ask your pharmacist if they’re trained in geriatric pharmacotherapy or if they use the CDC’s STEADI-Rx protocol.








Elan Ricarte
Let me tell you something-this whole system is a goddamn circus. We’re medicating grandma into a zombie just so she can ‘sleep’ while her balance goes to hell. Benzodiazepines? More like ‘Benzos for Fall-Pros’ if you ask me. And don’t get me started on the ‘just one more pill’ mentality. One guy I knew was on six sedating meds. Six. He didn’t fall-he just stopped walking. Took his meds, sat down, and never got up again. It’s not aging. It’s negligence dressed up as care.
And yeah, STEADI-Rx sounds great on paper, but who’s actually doing it? Your pharmacist? Nah. They’re too busy filling prescriptions for people who think ‘sleep aid’ means ‘I’m gonna nap through dinner.’ We need a fucking revolution in geriatric pharmacology, not another pamphlet.
Also, vitamin D? Please. If you’re not deficient, you’re just shelling out cash for glitter in a capsule. Exercise? Yes. But only if you stop treating it like a weekend hobby. You don’t do one Tai Chi class and call it a win. You do it like your life depends on it-because it does.
Camille Hall
Thank you for writing this. I’ve seen so many older relatives get stuck on meds that no one ever reevaluated. My mom was on amitriptyline for ‘anxiety’ for eight years-turns out, she just had chronic pain and no one connected the dots. When we finally got her off it, her dizziness vanished, and she started walking again. Not because of some miracle drug, but because we stopped treating symptoms and started treating the person.
Pharmacists are unsung heroes here. I wish more people knew they could walk into a pharmacy and ask for a full med review. No appointment. No charge. Just a conversation. And yes-exercise isn’t optional. Even 10 minutes of heel-to-toe walking by the kitchen counter counts. Small steps, literally and figuratively.
Ritteka Goyal
OMG I am from India and we dont have this problem here because we dont overmedicate like USA! In my village, old people drink turmeric milk, do yoga, and walk 5km daily. No pills! Only when they get very sick we give one or two medicine. But in USA, you give 10 pills for one problem! I saw a video of old man with 12 bottles of medicine, he was like walking pharmacy! This is madness.
Also, why you dont use Ayurveda? It is ancient science, from India, very safe. Why you always follow western medicine? Even WHO say Ayurveda is good for elderly. You need to learn from us! We dont have fall crisis because we dont overthink everything. Simple life, simple food, simple medicine. You need to change your culture, not just your pills!
THANGAVEL PARASAKTHI
Hey, I’m a pharmacist in Bangalore, and I’ve seen this play out in both India and the US. Yeah, India’s got less polypharmacy-but we’ve got our own mess: people buying antibiotics online, mixing herbal stuff with BP meds, and no real med reviews. STEADI-Rx? We should adapt it. We’ve got community pharmacists everywhere, just no training.
And vitamin D? Totally agree. My uncle took 2000 IU daily for years. His level was 45. Zero benefit. Waste of money. But his neighbor? Level was 12. Took 800 IU, started walking again. So yeah-test first. Don’t guess.
Also, Tai Chi? We’ve got it here too. Called ‘Yoga for Seniors.’ Same thing. Just need people to show up. Not hard. Just needs a quiet park and a loud instructor.
Chelsea Deflyss
So let me get this straight-you’re saying we should just STOP giving people meds that help them sleep, calm down, or feel less pain? Like, what, tell grandma to ‘tough it out’? That’s not care, that’s cruelty. Some people can’t walk, can’t sleep, can’t even hold a spoon without meds. You can’t just yank them away and say ‘do yoga instead.’
And who’s gonna do this ‘review’? The same overworked doctors who can’t even answer a simple question? Please. This isn’t a fix. It’s a guilt trip for people who already feel guilty for needing help.
Scott Conner
Wait, so if I’m on two sedating meds, I’m double the risk? What if I’m on three? Triple? Is there a calculator for this? I feel like someone should make a fall-risk app. Scan your med list, boom-red/yellow/green. Would save so many people. Also, why is baclofen so bad? I thought it was just for muscle spasms? Is it worse than the benzos? I need a chart. Someone please make a chart.
Sam Dickison
From a clinical perspective, the data here is solid. The FRID taxonomy is well-established, and the polypharmacy correlation is dose-dependent with a clear threshold at ≥3 agents. The STEADI-Rx model aligns with the Beers Criteria and the STOPP/START guidelines-both of which emphasize deprescribing as a primary intervention. What’s missing in practice isn’t evidence-it’s workflow integration. Most EHRs don’t flag FRIDs, and pharmacists aren’t reimbursed for time-intensive med reconciliation. We need policy change, not just awareness.
Also, exercise efficacy is supported by RCTs with effect sizes of 0.4–0.7. The number needed to treat to prevent one fall is ~5. That’s stronger than most pharmaceutical interventions. Yet we still prioritize pills over movement. Systemic bias.
Karianne Jackson
My grandma fell last year. Broke her hip. Now she’s in a wheelchair. They said it was ‘just age.’ But I know. It was the sleeping pill. The one she’d been on for 12 years. No one ever asked if she needed it. I cried for a week. Now I scream at every doctor. I won’t let it happen again. If you’re taking anything that makes you sleepy, ask. Just ask. Please.