Why mixing sedating meds can kill you
It’s not just a bad idea-it’s deadly. When you take two or more sedating medications together, your body doesn’t just feel more tired. Your breathing slows. Your brain shuts down parts it needs to stay alive. And sometimes, it stops working entirely. This isn’t a hypothetical risk. In 2020, 16% of opioid-related overdose deaths in the U.S. also involved benzodiazepines like Xanax or Valium. That’s not coincidence. It’s chemistry.
These drugs-opioids, benzodiazepines, sleep pills, muscle relaxers, even alcohol-don’t just add up. They multiply. That’s called synergy. Two drugs that each slow your breathing by 20% can together slow it by 70%. Your lungs don’t know how to catch up. Your blood doesn’t get enough oxygen. Your heart doesn’t get the signal to keep going. And you don’t wake up.
The deadliest combo: opioids and benzodiazepines
If you’re on an opioid for pain-oxycodone, hydrocodone, morphine-and your doctor also prescribed a benzodiazepine for anxiety or insomnia, you’re in a high-risk group. The FDA issued its first formal warning about this combination in 2016. Since then, data has only gotten worse.
A 2017 study in JAMA Internal Medicine found people taking both had a 154% higher risk of overdose than those on opioids alone. The odds ratio? 2.54. That means more than two and a half times more likely to die. And when you look at fatal overdoses specifically, the risk jumps even higher: patients with a current benzodiazepine prescription had a 3.86 times greater chance of dying from an opioid overdose.
Why? Opioids target the brainstem-the part that controls automatic breathing. Benzodiazepines boost GABA, a chemical that calms brain activity. Together, they silence the signals that tell your body to breathe. You don’t feel like you’re suffocating. You just drift deeper into sleep. And never wake up.
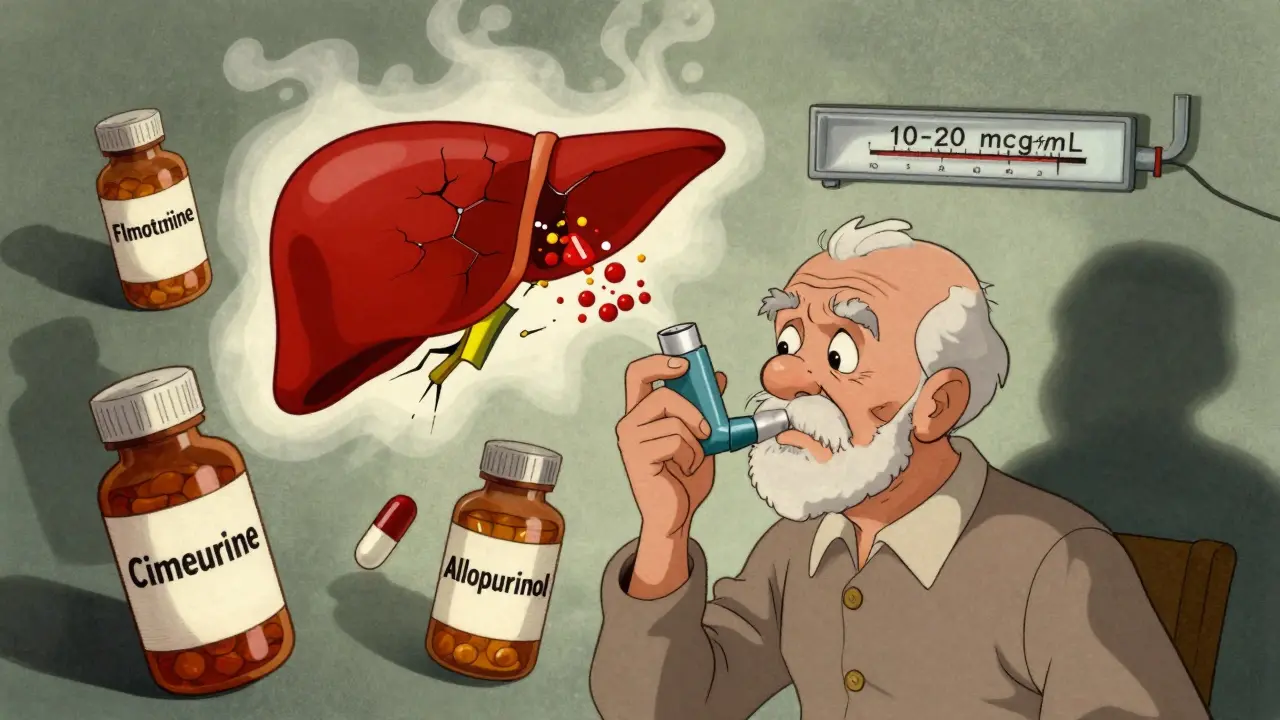
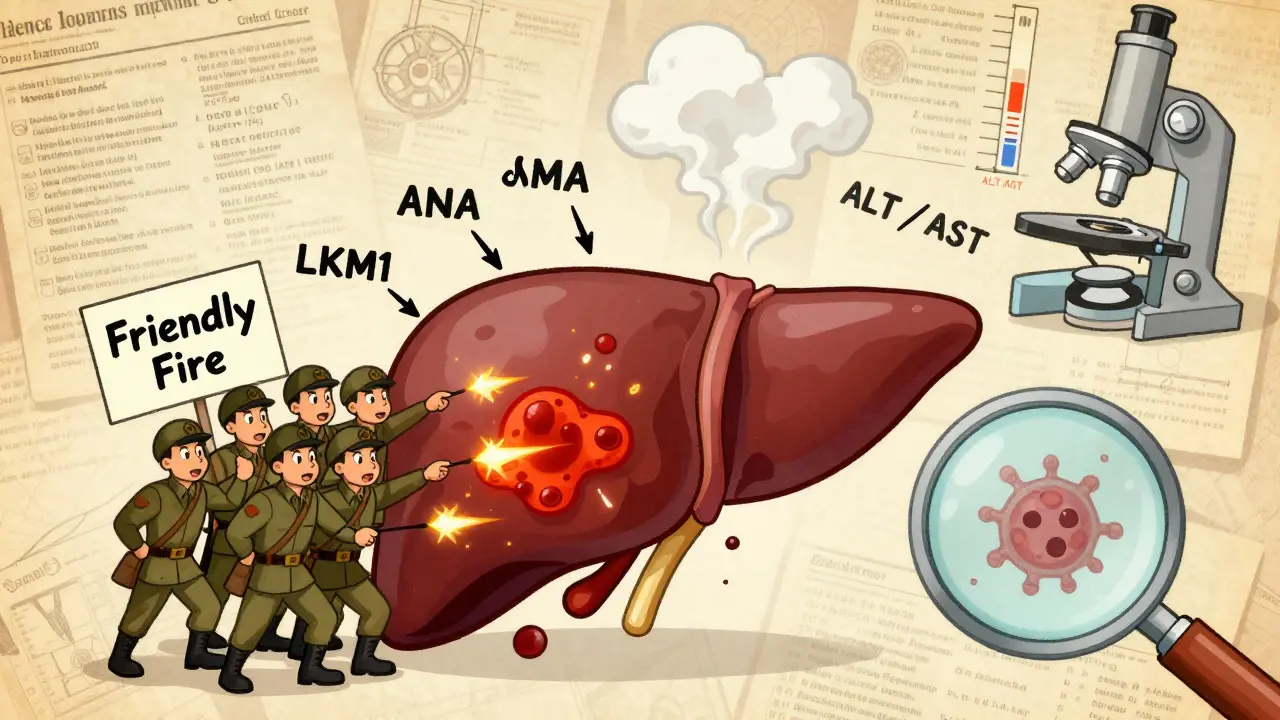
Other dangerous mixes you might not know about
It’s not just opioids and benzodiazepines. Other combinations are just as lethal.
- Alcohol + sleep meds (like Ambien or Lunesta): Just two drinks with a standard dose of zolpidem can cut your reaction time by 70%. That’s worse than being legally drunk. Falls, car crashes, and blackouts are common. One user on Reddit described a 10-hour blackout after mixing wine with his prescribed sleep pill-no memory of walking, talking, or even getting out of bed.
- SSRIs + MAOIs: These are antidepressants. Mixing them causes serotonin syndrome-a dangerous spike in serotonin levels. Symptoms include high fever, rapid heart rate, muscle rigidity, and seizures. Around 14-16% of cases are fatal if not treated fast.
- Benzodiazepines + muscle relaxers (like cyclobenzaprine): Both depress the central nervous system. The result? Extreme dizziness, confusion, and a 50% higher chance of falling, especially in older adults.
Even over-the-counter meds can be dangerous. Diphenhydramine (Benadryl) is a sedating antihistamine. Many people take it for sleep or allergies. Combine it with a prescription sleep aid? You’re doubling down on respiratory depression. No prescription needed to kill you.
Warning signs: What to watch for
You won’t always feel like something’s wrong. That’s the trick. These drugs make you drowsy, confused, or numb. But there are red flags that mean you’re in danger right now.
- Respiratory rate below 12 breaths per minute: Normal is 12-20. Below 12 means your body is shutting down.
- Blue lips or fingertips: That’s cyanosis-your blood isn’t carrying enough oxygen.
- Unresponsiveness to loud voices: If you can’t wake someone up with a firm shake or loud call, it’s not sleep. It’s overdose.
- Gurgling or snoring sounds: This isn’t just loud breathing. It’s airway collapse. Fluid is building up. Death is minutes away.
- Extreme confusion or slurred speech: Not just tired. Not just drunk. Disoriented in a way that doesn’t make sense.
If you see any of these in yourself or someone else-call 911 immediately. Don’t wait. Don’t try to ‘sleep it off.’ Naloxone (Narcan) can reverse opioid overdoses, but it won’t help if benzodiazepines or alcohol are involved. Only emergency care can save you.
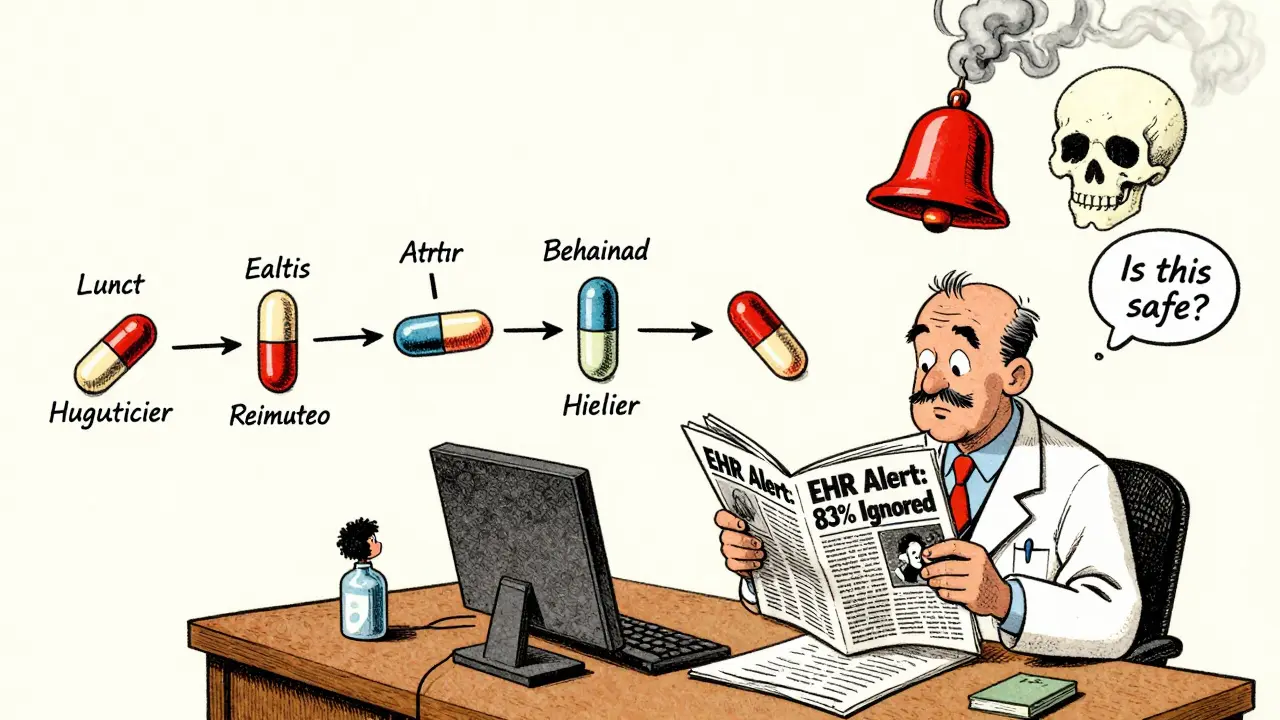
Why doctors miss this
You’d think your doctor would catch this. But they often don’t.
A 2020 study in JAMA Network Open found that only 17.3% of dangerous sedative combinations triggered alerts in electronic health records. That means out of 100 risky prescriptions, 83 go unnoticed by the system. Why? Because most EHRs don’t track total sedative burden-they look at single drugs, not cumulative effects.
And then there’s doctor shopping. Recovery Village data from 2022 shows that 42% of people who overdosed on combined sedatives had gotten prescriptions from three or more doctors in six months. They didn’t lie. They didn’t fake symptoms. They just saw different providers who didn’t talk to each other.
Older adults are especially vulnerable. The American Geriatrics Society’s Beers Criteria lists 19 sedating combinations to avoid in people over 65. Yet, 35% of seniors still take at least one inappropriate sedative. Women are even more likely-41% versus 27% of men.
What you can do to stay safe
You don’t have to live in fear. But you do need to be smart.
- Keep a complete list of everything you take: Prescription, OTC, supplements, herbal teas-even the ones you only take “as needed.” Include doses and why you take them.
- Bring this list to every doctor visit: Even if you see a new provider. Don’t assume they know what you’re on.
- Ask: ‘Is this safe with my other meds?’ Don’t wait for them to ask you. Say it out loud.
- Know your morphine milligram equivalents (MME): If you’re on opioids, ask your pharmacist what your daily MME is. Anything over 50 MME/day increases overdose risk. Over 90 MME? The risk doubles.
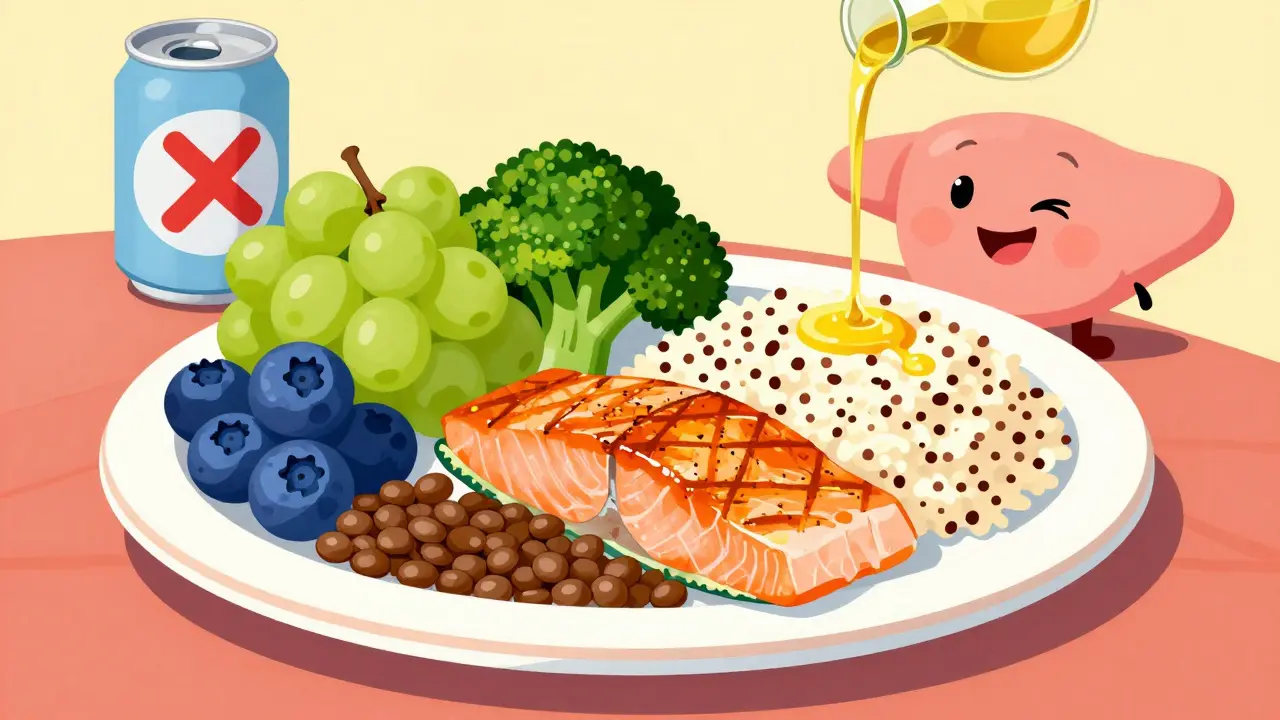
- Never mix with alcohol: No exceptions. Not one drink. Not one glass of wine. Not even a beer.
- Get a medication review every 3 months if you’re over 65: The START criteria say anyone over 65 on three or more sedating meds needs a full review within 30 days.
If you’re on multiple sedatives and want to cut back, don’t quit cold turkey. That can cause seizures, hallucinations, or rebound anxiety. Work with your doctor on a slow taper-usually 10-25% reduction every 1-2 weeks. For older adults, diazepam equivalents should never exceed 5 mg per day.

There’s hope-better tools are coming
Change is happening. In 2022, the FDA required all opioid and benzodiazepine packages to include a boxed warning-the strongest type. In 2023, all 50 states mandated electronic prescribing for controlled substances, which now includes automatic checks for dangerous combinations.
And there’s new tech. The FDA-approved DETERMINE platform, launched in July 2022, uses AI to predict your personal risk of a bad interaction with 87.4% accuracy. It looks at your age, weight, liver function, genetics, and current meds-not just the drugs themselves.
The NIH is investing $127 million over the next few years to develop pharmacogenomic tests that can tell you, before you even take a drug, whether your body will react dangerously to it. That’s the future.
But right now, the only thing that saves lives is awareness. Knowledge. Asking questions. Speaking up. You are your own best advocate.
What to do if you’re already on multiple sedatives
If you’re currently taking two or more sedating medications, don’t panic. But don’t ignore it either.
Start by talking to your primary care doctor or pharmacist. Ask: ‘Is this combination necessary? Is there a safer alternative?’ Many anxiety disorders can be treated with therapy or non-sedating meds like buspirone. Chronic pain can be managed with physical therapy, nerve blocks, or non-opioid pain relievers.
And if you’ve ever passed out, fallen without reason, or had a blackout after taking your meds-tell your doctor. That’s not weakness. That’s data. That’s a warning sign they need to act on.
Some people do benefit from carefully managed combinations-18% of patients in one Healthline survey said their quality of life improved under strict supervision. But that’s not the norm. It’s the exception. And it requires close monitoring, frequent check-ins, and zero alcohol.
If you’re not getting that level of care, you’re at risk. And you deserve better.
Can I mix my sleep pill with a glass of wine?
No. Mixing sleep medications like Ambien, Lunesta, or zaleplon with alcohol-even one drink-can dangerously slow your breathing and cause blackouts, falls, or death. The combined effect is not just additive-it’s multiplicative. Just two drinks with a standard dose of zolpidem can reduce reaction time by 70%. There is no safe amount.
What should I do if someone passes out after taking multiple sedatives?
Call 911 immediately. Do not try to wake them by shaking or slapping. If you have naloxone (Narcan) and suspect opioids are involved, administer it. But naloxone won’t reverse benzodiazepines or alcohol. Only emergency medical help can provide oxygen, breathing support, and monitoring. Do not wait to see if they wake up on their own.
Are over-the-counter sleep aids safe to combine with prescription sedatives?
No. Over-the-counter sleep aids like diphenhydramine (Benadryl) or doxylamine (Unisom) are sedating antihistamines. When combined with prescription sleep meds, benzodiazepines, or opioids, they increase the risk of respiratory depression, confusion, and falls. They are not harmless supplements-they’re CNS depressants with the same risks as prescription drugs.
Why don’t my doctors warn me about these combinations?
Many electronic health record systems don’t flag dangerous combinations unless they’re flagged by the FDA as a known high-risk pair. Even then, alerts are often ignored or overridden. Doctors may not know your full medication list, especially if you see multiple providers. You must be your own advocate-bring a complete list to every appointment and ask directly: ‘Is this safe with everything else I’m taking?’
Can I stop taking these meds on my own if I’m worried?
No. Stopping sedating medications suddenly-especially benzodiazepines or barbiturates-can cause seizures, hallucinations, or life-threatening withdrawal. Always work with your doctor to create a slow, supervised taper plan. Reducing by 10-25% every 1-2 weeks is typical. Never quit cold turkey.
Is it safe to take sedatives if I’m over 65?
The American Geriatrics Society Beers Criteria recommends avoiding most sedating medications in older adults due to increased fall risk and slowed metabolism. If you’re over 65 and taking a sedative, ask your doctor if it’s absolutely necessary. The daily diazepam equivalent should not exceed 5 mg. Even then, the risk of confusion, falls, and respiratory depression remains high. Non-drug options like sleep hygiene, CBT-I, or physical therapy are safer.
Next steps: Protect yourself today
Here’s what to do right now:
- Write down every medication, supplement, and OTC drug you take-include doses and why.
- Call your pharmacy and ask them to run a drug interaction check on your full list.
- Schedule an appointment with your doctor to review every sedating drug you’re on.
- Remove alcohol from your routine while taking any CNS depressant.
- Teach a family member the warning signs of overdose so they can act if you can’t.
Medications are meant to help. But when combined carelessly, they become silent killers. You don’t need to be a doctor to save your own life. You just need to ask the right questions-and listen to the answers.






Bob Cohen
I've seen this happen to a friend. Took Xanax for anxiety and oxy for back pain. Thought he was being careful. One night, he didn't wake up. No alarm. No struggle. Just... gone. The worst part? His doctor never flagged it. We all assumed he was just 'sleeping it off.' Don't be that person. Know your meds.
Ishmael brown
💀💀💀 I just took a Benadryl and a glass of wine. I'm already half-dead. If I don't wake up tomorrow, tell my cat I'm sorry. 🐱🍷
Aditya Gupta
Bro, this is real. My uncle died like this. 70+ and on 4 meds. No one told him. Just trusted the script. Don't wait for a tragedy. Ask questions. Now.
Nancy Nino
Let me be clear: this is not a suggestion. It is a public health emergency. The fact that 83% of dangerous combinations go unflagged by EHRs is not an oversight-it is a systemic failure. If your doctor doesn't proactively review your regimen, find a new one.
Jaden Green
The irony is thick enough to spread on toast. We have AI platforms like DETERMINE that can predict interactions with 87.4% accuracy, yet we still rely on human clinicians who are overworked, underpaid, and trained to treat symptoms-not polypharmacy. This isn't about individual responsibility-it's about a broken infrastructure that treats patients like data points with limbs.
Angel Fitzpatrick
You think this is about meds? Nah. This is Big Pharma’s quiet genocide. They push these combos because they know people will die. Then they sell the Narcan. Then they sell the grief counseling. Then they sell the ‘safe’ replacement drugs. It’s a cycle. A profit loop. And they’re laughing all the way to the bank while your grandma stops breathing.
Nidhi Rajpara
I am a nurse in Mumbai. We see this daily. Elderly patients on benzodiazepines, antihistamines, and NSAIDs. Families say, 'He just needs to sleep.' But sleep is not the goal. Survival is. Please, if you are reading this, take a list. To every appointment. Every single time.
Chris & Kara Cutler
Y’all need to stop sleeping on this. 💪 This is life or death. Print this. Stick it on your fridge. Tell your mom. Tell your uncle. Tell your weird cousin who takes melatonin with vodka. 🚨❤️
Donna Macaranas
I used to take Ambien and wine. Thought it helped me relax. Turns out I was just one step away from never waking up. I stopped. Started yoga. Now I sleep better. No pills. No regrets. You don't need chemical crutches to rest.
Rachel Liew
my grandma took 5 meds for sleep and anxiety. she fell 3 times last year. we didn’t connect it until she almost died. now she’s off everything but one low-dose thing. she smiles more. she walks better. please. ask. please.
Nicki Aries
I'm not saying this to scare you-I'm saying this because I've sat in ERs while families sobbed over bodies that didn't have to die. The fact that we have AI tools to prevent this, and yet people still mix alcohol with sleep meds? That's not ignorance. That's negligence. And it's killing people. Period.
Ed Di Cristofaro
you think your doctor cares? nah. they get paid to write scripts. not to read them. if you’re on more than 2 sedatives, you’re already playing russian roulette. and the gun’s loaded.