Autoimmune hepatitis isn’t something most people hear about until they or someone they know gets diagnosed. It’s not contagious. It’s not caused by drinking too much alcohol or eating the wrong foods. It’s your own immune system attacking your liver - like a friendly fire incident inside your body. And when it happens, it doesn’t just fade away on its own. Left untreated, it can lead to cirrhosis, liver failure, or even the need for a transplant. The good news? We’ve known how to treat it for decades, and the treatments - steroids and azathioprine - still work better than almost anything else we have today.
How Do You Know You Have Autoimmune Hepatitis?
There’s no single blood test that says, "Yes, you have autoimmune hepatitis." Instead, doctors piece together clues. First, your liver enzymes - ALT and AST - are usually way up. Like, 5 to 10 times higher than normal. That’s a red flag. But so are viral hepatitis, fatty liver, or even a bad reaction to a medication. So the next step is checking for autoantibodies. Most people with autoimmune hepatitis have either antinuclear antibodies (ANA) or smooth muscle antibodies (SMA). A smaller group has LKM1 antibodies. These aren’t just random markers. They’re signs your immune system is targeting liver cells.
But here’s the catch: the type of antibody doesn’t change how you’re treated anymore. The 2025 European Association for the Study of the Liver guidelines dropped the old system of dividing AIH into Type 1 and Type 2 based on antibodies. Why? Because whether you have ANA or LKM1, you still get the same drugs. The focus now is on what’s happening inside the liver.
That’s where the liver biopsy comes in. It’s not fun, but it’s necessary. A needle takes a tiny sample of liver tissue, and under the microscope, doctors look for something called interface hepatitis - inflammation right where the liver’s blood vessels meet the tissue. If you see that, along with high IgG levels (a type of antibody that’s elevated in 80% of cases), and you’ve ruled out other causes like hepatitis B or C, then the diagnosis is solid. The International Autoimmune Hepatitis Group scoring system helps: if your score is over 15, it’s probable. Over 20? Definite.
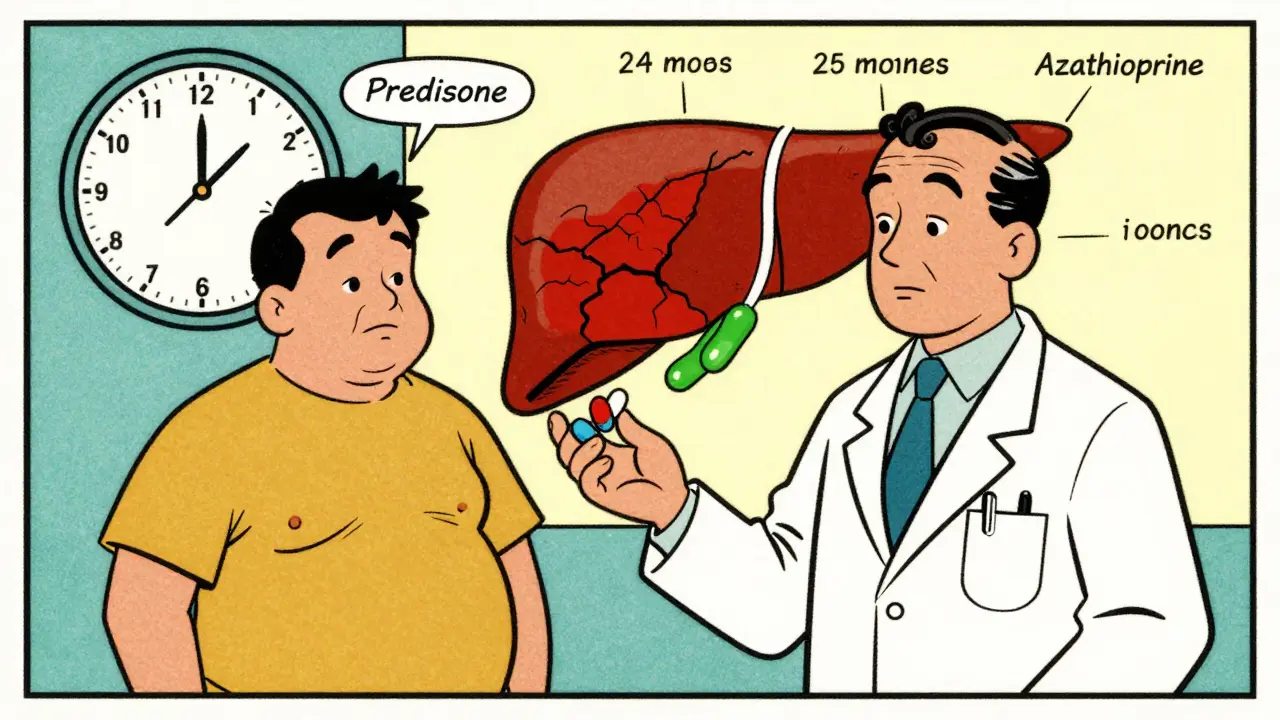
Why Steroids Are the First Line of Defense
Prednisone (or its cousin prednisolone) has been the go-to drug since the 1970s. It’s not a cure, but it’s a powerful suppressor of the immune system. The goal isn’t to kill the immune system - it’s to quiet it down enough so the liver can heal. Most patients start with 0.5 to 1 mg per kilogram of body weight per day. For a 70 kg person, that’s about 35 to 70 mg daily. That sounds like a lot, and it is. But here’s the thing: most people start feeling better within two weeks. Liver enzymes drop. Fatigue lifts. Some even notice their skin color improves.
But steroids come with a price. Within weeks, side effects show up. Weight gain - especially around the face and belly. Mood swings. Trouble sleeping. Insulin resistance that can lead to diabetes. Bone thinning. Cataracts. About 70% of people on steroid-only therapy deal with at least one major side effect. That’s why doctors don’t keep you on high doses forever. The plan is to taper down. By week 8, you’re usually down to 10-15 mg a day. The goal is to get you as low as possible, as fast as possible - and that’s where azathioprine steps in.
Azathioprine: The Steroid-Sparing Partner
Azathioprine (sold as Azasan or Imuran) isn’t a steroid. It’s an immunosuppressant that works differently. It slows down the immune system by interfering with DNA synthesis in white blood cells. It doesn’t work fast. It takes weeks to months to show its effect. But once it kicks in, it lets you cut back on steroids - often by 70-80%. That’s huge. A 2023 study found that combination therapy (steroids + azathioprine) cut steroid side effects from 70% down to 30%. That’s not just a number - it’s your quality of life.
But azathioprine isn’t risk-free. It can cause nausea, vomiting, or pancreatitis. In rare cases, it can crash your bone marrow, leading to low white blood cells or platelets. That’s why doctors test for TPMT enzyme levels before starting. About 0.3% of people have a genetic variant that makes them unable to break down azathioprine. For them, even a normal dose can be deadly. Testing costs $250-$400, and while it’s routine in Europe, only 45% of U.S. centers do it. If you’re in the U.S., ask for it. It’s not optional - it’s essential.
Most people start azathioprine at 50 mg a day, then increase to 1-2 mg per kg daily (up to 150 mg). It’s usually taken long-term. Some patients stay on it for life. And yes, it’s expensive - branded Imuran can cost $300-$500 a month. But the generic version? $25-$50. Always check for it.
How Long Until You See Results?
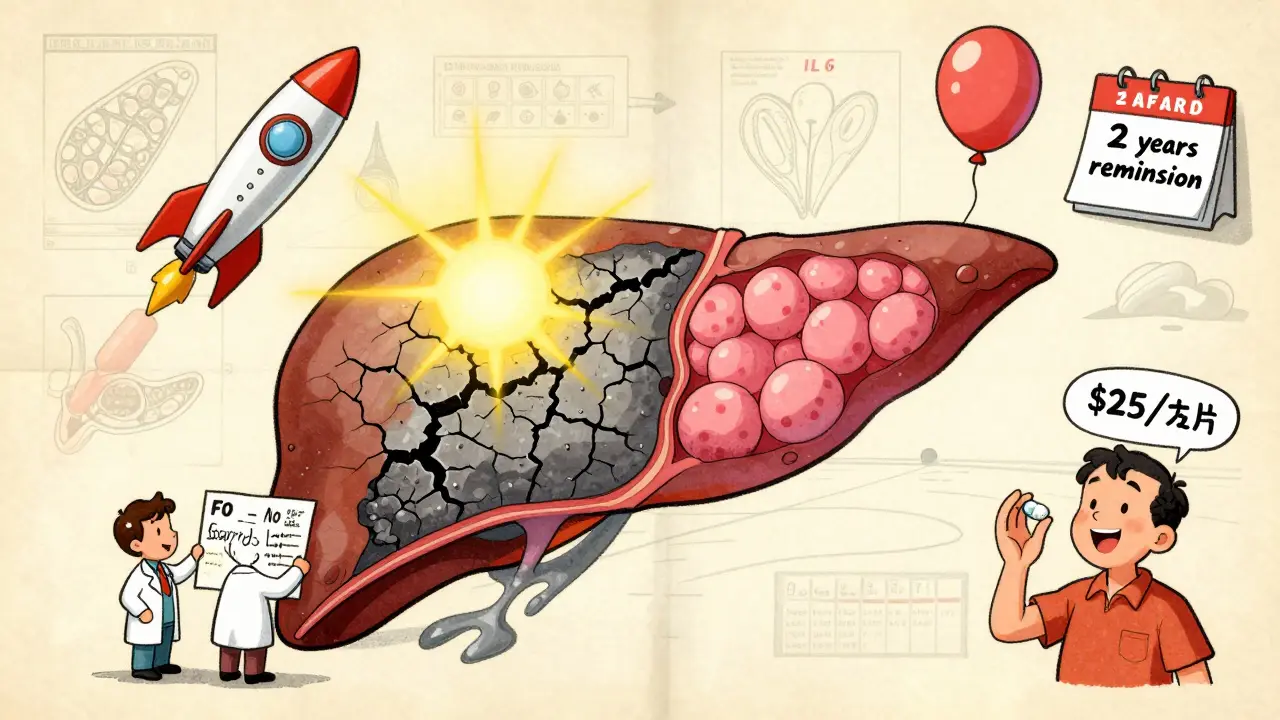
It’s not a sprint. It’s a marathon. Most patients show biochemical improvement - meaning ALT and AST levels drop - within 2 to 4 weeks. But true healing? That takes time. The liver needs months to repair the damage. Complete normalization of liver enzymes and IgG levels usually happens between 18 and 24 months. That’s why the 2025 EASL guidelines changed the timeline. Instead of checking response at 6 months, they now recommend waiting 6 to 12 months. Some people just take longer.
By the end of two years, 60-80% of patients reach complete biochemical remission. That means their blood tests look normal. But remission doesn’t always mean the liver is fully healed. That’s why a second biopsy after 2-3 years is often recommended. If the inflammation is gone, you’re in histological remission. That’s the gold standard. And yes - in many cases, the liver fibrosis reverses. One patient on Reddit described going from F3 (advanced scarring) to F0 (no scarring) after two years of treatment. That’s not rare. It’s documented.
What If It Doesn’t Work?
About 10-15% of people don’t respond to steroids and azathioprine. That’s treatment failure. It doesn’t mean you’re out of options. The next step is mycophenolate mofetil (CellCept). It’s taken twice daily, and while it’s pricier - $800-$1,200 a month - it’s effective for many who can’t tolerate azathioprine. Calcineurin inhibitors like tacrolimus are another option, especially for patients with LKM1-positive AIH.
There’s new hope on the horizon. Drugs like tofacitinib (a JAK inhibitor) and clazakizumab (an anti-IL-6 antibody) are in phase 2 trials. Early results show 50-55% response rates in people who failed standard therapy. And obeticholic acid (Ocaliva), originally for primary biliary cholangitis, just got FDA breakthrough designation for AIH. Phase 3 trials showed a 42% complete response rate - better than standard therapy.
Stopping Treatment: The Risky Gamble
Many patients want to stop. Who wouldn’t? Steroids wreck your body. Azathioprine is a daily pill with its own risks. But stopping too soon is dangerous. Studies show 50-90% of patients relapse if they stop treatment. Even if you’ve been in remission for two years, the relapse rate is still 50%. That’s why doctors only consider stopping after 2-3 years of stable remission - and even then, they taper slowly over 6-12 months. And you’re monitored like a hawk. Most relapses happen in the first 3 months after stopping.
Only 45% of attempts to stop treatment succeed. That means more than half need to go back on medication. So don’t rush. Talk to your doctor. If you’re thinking about stopping, get a repeat biopsy. Don’t rely on blood tests alone.
What You Need to Do Before Starting Treatment
Before you take your first pill, there are two critical steps. First, get tested for hepatitis B. About 15-20% of people with AIH have hidden (occult) hepatitis B. If you start immunosuppressants without treating it, the virus can explode. That’s life-threatening. If you’re positive, you’ll need antiviral therapy like tenofovir before starting steroids or azathioprine.
Second, get vaccinated. If you haven’t had hepatitis A or B vaccines, get them now - before you start immunosuppression. Once you’re on steroids or azathioprine, your immune system won’t respond as well. Vaccine effectiveness drops from 90% to 40-60%. Get them early. Protect your liver before you start suppressing your immune system.
Real Stories, Real Side Effects
One patient on Reddit said: "Moon face. 30 pounds of fluid weight in three weeks. Insomnia like permanent jet lag." Another said azathioprine gave them pancreatitis at 100 mg. They switched to mycophenolate - and finally saw their liver enzymes drop.
But there are wins too. A woman in the Autoimmune Hepatitis Association registry said: "After two years on 5 mg prednisone and 75 mg azathioprine, my biopsy showed complete fibrosis reversal." That’s the power of this treatment. It doesn’t just slow things down. It can heal.
Side effects are real. Weight gain. Mood swings. Hair thinning. Fatigue. Bone loss. But they’re manageable. With good monitoring, diet, exercise, calcium and vitamin D supplements, and regular bone density scans, many patients live full lives on these drugs. The alternative - cirrhosis, liver failure - is far worse.
What’s Next for AIH Treatment?
Research is moving fast. The STOP-AIH trial is testing whether people in long-term remission can safely stop treatment. Early data suggests 65% stay in remission - much better than past numbers. The AASLD is developing a patient decision tool to help people understand the trade-offs between side effects and disease control. And biomarkers are being studied. A blood test using microRNA panels can now predict steroid responsiveness within two weeks. That could mean less trial and error.
For now, the standard remains: steroids and azathioprine. It’s not perfect. But it’s effective. It’s been proven. And for most people, it’s life-saving.
Can autoimmune hepatitis be cured?
Autoimmune hepatitis can’t be cured in the traditional sense - meaning, the immune system doesn’t go back to normal. But it can be controlled. With proper treatment, most patients reach remission, where liver enzymes normalize and inflammation stops. Some even see liver scarring reverse. The goal is long-term control, not a cure.
How long do you need to take steroids and azathioprine?
Most patients need treatment for at least 2-3 years. Many require lifelong therapy. About 60-80% of people need maintenance treatment. Stopping too early leads to relapse in 50-90% of cases. If you’re in deep remission for years, your doctor might consider a very slow taper - but only after a repeat biopsy confirms healing.
Is azathioprine safe long-term?
Yes, for most people. The biggest risk is bone marrow suppression, which is rare if you’ve been tested for TPMT enzyme levels. Regular blood tests every 3 months catch any drops in white cells or platelets early. Long-term use is associated with a slightly higher risk of certain cancers, but the risk is low compared to the danger of untreated liver damage.
Why do I need a liver biopsy if my blood tests are normal?
Blood tests show inflammation, but they don’t show healing. A biopsy reveals whether the liver tissue has actually repaired itself. You can have normal ALT levels but still have active inflammation under the surface. That’s why biopsies are used to confirm remission - not just to diagnose.
Can I drink alcohol if I have autoimmune hepatitis?
No. Alcohol adds stress to your liver - and your liver is already under attack from your immune system. Even small amounts can speed up scarring and increase the risk of cirrhosis. Complete abstinence is strongly recommended.
Are there alternatives to steroids and azathioprine?
Yes, but only if you can’t tolerate them. Mycophenolate mofetil is the most common second-line drug. Calcineurin inhibitors like tacrolimus are used for resistant cases. New drugs like JAK inhibitors and monoclonal antibodies are showing promise in trials but aren’t standard yet. For now, steroids and azathioprine remain the most effective and widely used combination.





