Hypertension Drug Comparison Tool
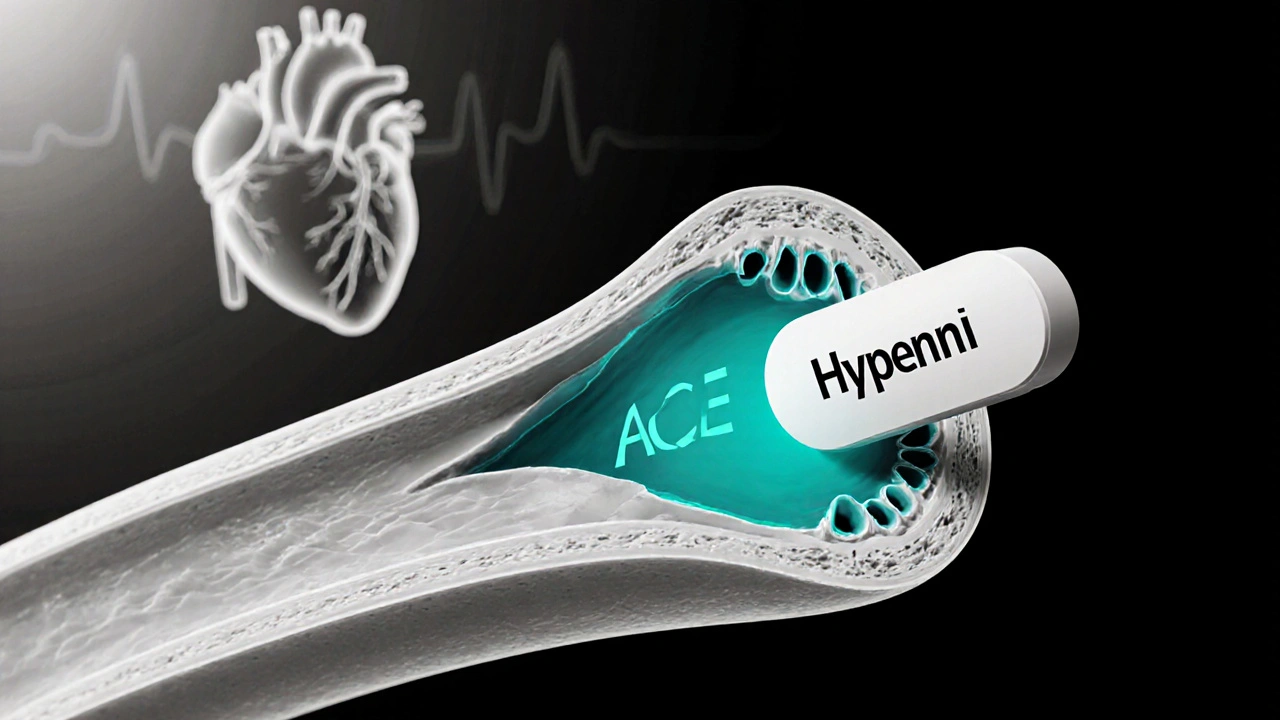
Hypernil is the brand name for Lisinopril, an ACE inhibitor that’s used to treat high blood pressure and heart failure. It works by relaxing blood vessels, which makes the heart pump more easily. If you’ve ever wondered whether Hypernil is the right choice or if another drug might suit you better, you’re in the right place.
- Hypernil lowers blood pressure by blocking the enzyme that tightens vessels.
- Alternative drugs fall into four main classes: ACE inhibitors, ARBs, calcium‑channel blockers, and thiazide diuretics.
- Side‑effects differ by class - cough is common with ACE inhibitors, while swelling is more typical with calcium‑channel blockers.
- Cost varies widely; generic ACE inhibitors are usually the cheapest option.
- Choosing the best drug depends on your overall health, other meds, and how you tolerate side‑effects.
How Hypernil (Lisinopril) Lowers Blood Pressure
When you take Hypernil, it blocks the enzyme angiotensin‑converting enzyme (ACE). This prevents the conversion of angiotensin I to angiotensin II, a powerful vasoconstrictor. With less angiotensinII, your arteries stay relaxed, blood flows more freely, and the heart doesn’t have to work as hard.
Typical adult dosing starts at 10mg once daily, with the possibility to increase to 40mg based on blood‑pressure response. The tablet is taken with or without food, but it’s best to keep the timing consistent each day.
Alternative Drug Classes at a Glance
Not every patient tolerates an ACE inhibitor. Below are the most common alternatives, each with a brief snapshot.
Losartan is an angiotensinII receptor blocker (ARB) that blocks the same pathway downstream of ACE, avoiding the cough that many people get with ACE inhibitors.
Amlodipine belongs to the calcium‑channel blocker (CCB) family. It stops calcium from entering smooth‑muscle cells, which keeps arteries from tightening.
Hydrochlorothiazide is a thiazide diuretic that reduces fluid volume by prompting the kidneys to excrete more sodium and water, indirectly lowering pressure.
Enalapril is another ACE inhibitor, chemically similar to lisinopril but often prescribed at lower doses.
Ramipril is a long‑acting ACE inhibitor that’s favored for patients with both hypertension and high cardiovascular risk.
Valsartan is an ARB that’s commonly used when a patient can’t tolerate ACE inhibitors or needs an additional blood‑pressure‑lowering effect.
Side‑Effect Profiles: What to Expect
Every drug class carries its own set of typical adverse effects. Here’s a quick rundown:
- ACE inhibitors (Hypernil, Enalapril, Ramipril): dry cough, elevated potassium, rare angio‑edema.
- ARBs (Losartan, Valsartan): fewer cough complaints, possible dizziness, occasional high potassium.
- Calcium‑channel blockers (Amlodipine): swelling of ankles, flushing, heart‑rate changes.
- Thiazide diuretics (Hydrochlorothiazide): increased urination, low potassium, higher uric acid.
Knowing these patterns helps you and your doctor spot problems early. For instance, if a new cough appears after starting Hypernil, the doctor may switch you to Losartan.
Cost and Insurance: Putting Numbers on Therapy
Price matters, especially if you’re paying out‑of‑pocket. Generic lisinopril (Hypernil’s active ingredient) typically costs between $4 and $12 for a 30‑day supply in the U.S. by 2025. By contrast, brand‑name ARBs can run $30‑$60, while calcium‑channel blockers and thiazides sit somewhere in the $10‑$30 range depending on insurance coverage.
Most insurance plans treat generic ACE inhibitors as a Tier1 drug, meaning a low copay. ARBs often land in Tier2, so you might pay a bit more. Always check your pharmacy benefits for the latest formulary listings.
Choosing the Right Medication: Practical Decision Tree
- If you have no history of cough or angio‑edema, start with Hypernil or another generic ACE inhibitor.
- If you develop a persistent dry cough, ask your doctor about switching to an ARB such as Losartan or Valsartan.
- For patients with chronic kidney disease, ACE inhibitors or ARBs are preferred because they protect kidney function.
- If you need a rapid blood‑pressure drop or have coronary artery disease, Amlodipine (CCB) may be added.
- When fluid retention is a concern (e.g., in heart‑failure patients), combine a diuretic like Hydrochlorothiazide with an ACE inhibitor.
This flow isn’t a substitute for medical advice, but it mirrors how clinicians often personalize therapy.
Side‑by‑Side Comparison Table
| Drug (Brand) | Class | Typical Dose | Key Benefits | Common Side‑effects | 2025 Avg. Monthly Cost (US) |
|---|---|---|---|---|---|
| Hypernil (Lisinopril) | ACE inhibitor | 10‑40mg daily | Proven CV risk reduction, kidney protection | Cough, elevated K⁺, rare angio‑edema | $8 |
| Losartan | ARB | 50‑100mg daily | Same BP reduction without cough | Dizziness, high K⁺ | $30 |
| Amlodipine | Calcium‑channel blocker | 5‑10mg daily | Effective for isolated systolic hypertension | Peripheral edema, flushing | $20 |
| Hydrochlorothiazide | Thiazide diuretic | 12.5‑25mg daily | Reduces fluid volume, works well in combos | Low K⁺, increased urination | $10 |
| Enalapril | ACE inhibitor | 5‑20mg daily | Similar efficacy to lisinopril | Cough, taste disturbances | $12 |
| Ramipril | ACE inhibitor | 2.5‑10mg daily | Long‑acting, good for high‑risk patients | Cough, rash | $14 |
| Valsartan | ARB | 80‑160mg daily | Effective after ACE‑inhibitor intolerance | Dizziness, high K⁺ | $32 |
Frequently Asked Questions
Can I take Hypernil with a diuretic?
Yes. Combining an ACE inhibitor like Hypernil with a thiazide diuretic such as Hydrochlorothiazide is a common strategy to achieve stronger blood‑pressure control. Your doctor will monitor electrolytes, especially potassium.
Why do some people develop a cough on lisinopril?
Lisinopril increases bradykinin levels in the lungs, which can trigger a dry, persistent cough. Switching to an ARB like Losartan usually resolves the symptom.
Is Hypernil safe during pregnancy?
ACE inhibitors are classified as pregnancy category D, meaning they can harm the developing fetus. Women who are pregnant or planning to become pregnant should use alternative medicines under medical guidance.
How quickly does Hypernil start working?
Blood‑pressure reduction can be seen within 1‑2hours after the first dose, with the full effect appearing after 2‑4weeks of consistent use.
Can I switch from Hypernil to Losartan without a wash‑out period?
In most cases, doctors can transition directly because the half‑life of lisinopril is short. However, a brief overlap may be advised for patients with unstable blood pressure.






Dan Tenaguillo Gil
When you first start an ACE inhibitor like Hypernil, it helps to know that the drug does more than just lower the number on the cuff; it also improves the health of your blood‑vessel lining over time. The mechanism involves blocking the conversion of angiotensin I to angiotensin II, which means the vessels stay relaxed and the heart doesn’t have to pump as hard, a benefit that accumulates with consistent use. Because of this, many clinicians pair lisinopril with lifestyle changes such as reduced sodium intake, regular aerobic exercise, and weight management to amplify the effect. It’s also wise to monitor your blood pressure at the same time each day, preferably in the morning, to get an accurate trend and adjust dosage if needed. While the typical starting dose is 10 mg daily, the titration up to 40 mg should be guided by both your systolic and diastolic readings as well as how you feel; sudden dizziness or light‑headedness can signal that you’re overshooting. Keep an eye on potassium levels, especially if you’re also taking a potassium‑sparing diuretic, because ACE inhibitors can raise serum potassium and lead to hyperkalaemia in susceptible individuals. Routine labs every three to six months are a good practice, even if you feel fine, since kidney function can also be affected. If a persistent dry cough develops, that’s a classic side‑effect tied to elevated bradykinin in the lungs, and most doctors will gladly switch you to an ARB like Losartan to avoid that annoyance. Remember that the cough isn’t a sign of infection; it’s a pharmacologic quirk you can discuss with your prescriber. For patients with a history of angio‑edema, the risk is low but present, so any swelling of the lips, tongue, or throat should prompt an immediate medical review. The cost factor is often overlooked, but generic lisinopril’s price point makes it a budget‑friendly option for most insurance plans, which typically place it in Tier 1 with a low copay. In contrast, many brand‑name ARBs sit in Tier 2 or higher, which can add a noticeable expense if you’re paying out‑of‑pocket. If you’re dealing with chronic kidney disease, the protective effect of ACE inhibitors on renal perfusion makes them a first‑line choice, as they reduce proteinuria and slow progression. However, you’ll want to coordinate with a nephrologist to ensure dosing is appropriate for your reduced glomerular filtration rate. For heart‑failure patients, combining Hypernil with a thiazide diuretic can enhance fluid removal, but you must watch electrolytes closely, particularly potassium and sodium. Lastly, never stop the medication abruptly without consulting your doctor; tapering off slowly helps prevent rebound hypertension, a phenomenon where blood pressure spikes higher than before treatment. By keeping these practical points in mind, you can turn a simple prescription into a well‑rounded, personalized hypertension strategy.
Ellie Chung
Jumping straight into the nitty‑gritty, I’ve tried Hypernil for a couple of months and the cough thing really showed up like a mischievous neighbor screaming at 3 am; swapping to Losartan was a game‑changer, and my blood pressure stayed rock‑solid without that annoying throat tickle. Also, the price tag on the generic was pleasantly low, so my wallet didn’t scream either.
Sophia Simone
Whilst the comparative table is exhaustive, it neglects to mention that the pharmacokinetic profiles of lisinopril and enalapril differ not only in half‑life but also in hepatic activation, an aspect crucial for patients with impaired liver function. Moreover, the assertion that ARBs present ‘fewer cough complaints’ oversimplifies the nuanced incidence of angio‑edema, which, albeit rare, is not exclusive to ACE inhibitors. The cost analysis, albeit accurate for the United States, fails to account for regional pricing disparities, rendering the advice less universally applicable. Finally, the decision tree assumes linear patient pathways, ignoring the reality of polypharmacy and comorbidities that often compel clinicians to deviate from textbook protocols.
Dean Briggs
In reflecting upon the decision tree presented, it becomes evident that such linear schemata, while pedagogically useful, risk oversimplifying the lived experience of managing hypertension amidst the tapestry of daily life. One must consider not only the pharmacological parameters but also the psychosocial elements: the stress of work, the cultural attitudes toward medication adherence, and the fluctuating rhythms of sleep that can modulate blood pressure independent of drug selection. Hence, while the algorithm correctly prioritises ACE inhibitors for patients without cough or angio‑edema, a practitioner should incorporate shared decision‑making, allowing patients to voice concerns about side‑effects, cost, or pill burden. The philosophical underpinning of medicine, after all, is a balance between evidence and empathy, a dance where the clinician leads but must remain responsive to the patient’s tempo. This perspective aligns with the notion that therapeutic success is not merely the numbers on a sphygmomanometer but the holistic well‑being of the individual, a principle that arguably deserves more prominence in educational resources.
Sadie Speid
Take heart, folks! Even if the numbers seem daunting, staying consistent with Hypernil can bring real, measurable improvements in cardiovascular risk-stay motivated, track your readings, and celebrate each small victory.
Sue Ross
I hear you, and it’s reassuring to know that many have navigated the cough issue successfully; your openness about side‑effects helps others feel less isolated.
Rohinii Pradhan
It is imperative to note that the pharmacodynamic description of lisinopril herein omits the critical detail that its bioavailability is approximately 25 %, a fact that influences both dosing strategies and therapeutic expectations. Furthermore, the claim regarding generic cost uniformity neglects the variability introduced by pharmacy pricing algorithms, which can cause substantial out‑of‑pocket discrepancies. A precise exposition should also address the contraindication in pregnancy, emphasizing that teratogenic risk supersedes the modest financial advantage. Lastly, the side‑effect enumeration would benefit from quantifying incidence rates, thereby furnishing clinicians with data‑driven guidance rather than anecdotal warnings.
Anna-Lisa Hagley
The analysis is thorough, yet the tone borders on being overly pompous, obscuring the practical takeaways that patients actually need.
A Walton Smith
Nice.
Theunis Oliphant
One must consider the elegance of simplicity; a medication that does its job without fanfare is often the most virtuous.