For someone living with rheumatoid arthritis (RA), the daily pain, stiffness, and swelling aren’t just discomfort-they’re a loss of control. Over time, untreated RA doesn’t just hurt joints; it eats away at them. But in the last 25 years, a new class of drugs has changed the game: biologic DMARDs. These aren’t your grandfather’s arthritis pills. They’re precision tools, designed to shut down specific parts of the immune system that turn against your own body. And for many, they don’t just ease symptoms-they make remission possible.
What Are Biologic DMARDs, Really?
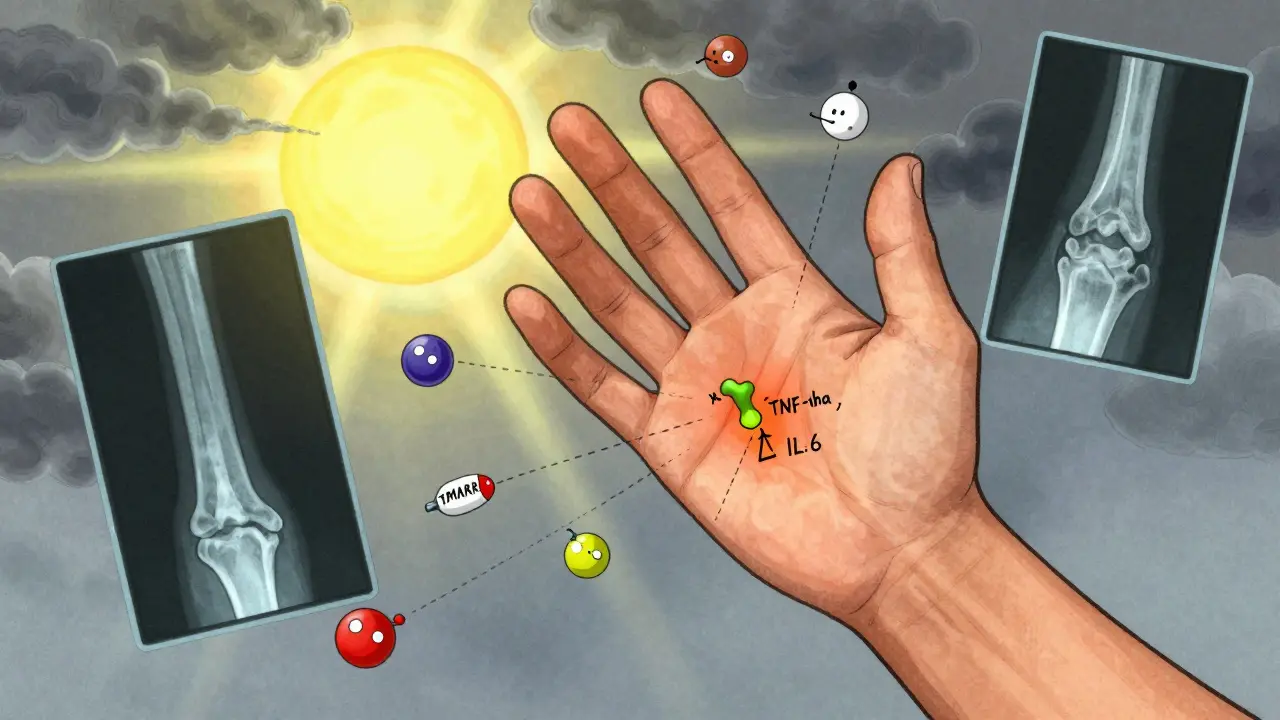
Biologic DMARDs (disease-modifying antirheumatic drugs) are made from living cells, not chemicals. They’re engineered to block specific proteins that drive inflammation in RA. Unlike older drugs like methotrexate, which broadly suppress the immune system, biologics target just the troublemakers-like TNF-alpha, IL-6, or T-cells. Think of it like using a sniper instead of a shotgun. The first one, etanercept (Enbrel), hit the market in 1998. Since then, we’ve seen a wave of new options: adalimumab (Humira), infliximab (Remicade), rituximab (Rituxan), abatacept (Orencia), and tocilizumab (Actemra). Each one works differently. Some block TNF, others stop T-cells from activating, and a few silence interleukins. The result? For many, pain drops, swelling fades, and X-rays show less joint damage.Remission Isn’t Just a Dream-It’s a Target
The goal isn’t just to feel a little better. It’s to reach remission: no signs of active disease. The American College of Rheumatology and EULAR both now treat RA like a chronic condition you can control, not just manage. Studies show that with biologics, 20-50% of patients achieve remission. Without them? Only 5-15% do. One patient in Seattle, diagnosed in 2018, had swollen hands and couldn’t open jars. After six months on adalimumab, her DAS28 score dropped from 5.8 (high disease activity) to 1.9 (remission). She’s been symptom-free for three years. That’s not rare. It’s becoming the new normal for those who respond.Not All Biologics Are the Same
Choosing the right one isn’t guesswork. It’s based on your biology, your history, and even your lifestyle.- TNF inhibitors (etanercept, adalimumab, infliximab): Fast-acting. Many feel better in days. Best for patients with high inflammation markers.
- IL-6 blockers (tocilizumab): Great for patients with fatigue, anemia, or high CRP levels. Works even if TNF inhibitors failed.
- T-cell modulators (abatacept): Slower to work, but fewer infections. Good for older patients or those with recurring infections.
- B-cell depleters (rituximab): Ideal if you have high levels of B-cells in your joints. But if your synovial tissue shows low B-cell activity? Only 12% respond.
- JAK inhibitors (tofacitinib, upadacitinib): Oral pills, not injections. Upadacitinib beat adalimumab in head-to-head trials. But they carry a black box warning for blood clots and cancer risk.
Cost and Access: The Real Barrier
These drugs work-but they’re expensive. In the U.S., a year of treatment costs $50,000 to $70,000. That’s why many patients delay starting them, or drop out when insurance denies coverage. Biosimilars have changed that. Since 2016, copies of Humira and Enbrel have hit the market. They’re 15-30% cheaper. In 2023, 35% of TNF prescriptions in the U.S. were biosimilars. One patient switched from Humira to its biosimilar and cut her monthly copay from $400 to $120. But insurance still fights it. Getting approval can take 7-14 days. Some patients lose weeks of treatment while waiting. Manufacturer assistance programs can cover up to 100% of costs-but you need to apply, and paperwork is a nightmare.Side Effects: What No One Tells You
Biologics aren’t magic. They weaken your immune system’s ability to fight infections. You’re more likely to get pneumonia, tuberculosis, or skin infections. The risk is 1.39 times higher than with placebo. Common complaints from patients:- Injection site redness or itching (45% of adverse events)
- Frequent colds or sinus infections (30%)
- Fatigue or headaches
- High out-of-pocket costs (25%)
What If It Stops Working?
About 40% of patients lose response after 12-24 months. This is called secondary non-response. It’s not failure-it’s biology. Your immune system adapts. The key? Don’t wait. If your symptoms creep back, talk to your rheumatologist. Switching to a different class of biologic often works. For example, if a TNF inhibitor failed, switching to an IL-6 blocker or JAK inhibitor can bring remission back. But here’s the catch: each new biologic you try has diminishing returns. The third or fourth one rarely works as well as the first. That’s why experts now say: get it right the first time.
How to Get Started
If you’re considering biologics, here’s what you need to do:- Confirm you’ve tried methotrexate (or another csDMARD) for at least 3-6 months without enough improvement.
- Get blood tests: CRP, ESR, RF, anti-CCP. These help predict response.
- Ask for a TB skin test and possibly a chest X-ray.
- Discuss your lifestyle: Can you handle weekly injections? Do you travel often? Infliximab requires clinic visits every 4-8 weeks.
- Ask about biosimilars. They’re just as effective, cheaper, and often covered faster.
- Use tools like ArthritisPower or MyRApath to track symptoms and share data with your doctor.
The Future: Personalized RA Treatment
The next frontier isn’t just more drugs-it’s smarter choices. Researchers are analyzing synovial tissue from joint biopsies to predict which drug will work best. One 2022 study showed that patients with high B-cell signatures responded to rituximab; those with high IL-6 levels did better on tocilizumab. Longer-acting versions are coming. A twice-yearly injection of tocilizumab is in Phase III trials. That means fewer shots, fewer trips to the clinic. And cost? Biosimilars are expected to make up 60% of the biologic RA market by 2027. More competition means lower prices-and more people getting treated.Final Thought: Remission Is Possible
Rheumatoid arthritis used to mean a slow, painful decline. Now, for many, it means a quiet life. No swelling. No morning stiffness. No painkillers. Just living. Biologic DMARDs didn’t cure RA. But they turned it from a life sentence into a manageable condition. And that’s not just science-it’s hope.Can biologic DMARDs really put rheumatoid arthritis into remission?
Yes. Clinical trials show that 20-50% of RA patients achieve remission with biologic DMARDs, compared to only 5-15% with older drugs like methotrexate alone. Remission means no detectable signs of active disease-no joint swelling, normal blood markers, and no pain. It’s not a cure, but it’s the closest thing we have.
How long does it take for biologic DMARDs to work?
TNF inhibitors like adalimumab or etanercept often start working within days to weeks. Non-TNF biologics like abatacept or rituximab may take 3-6 months to show full effect. Patience is key, but if there’s no improvement after 3 months, your doctor may switch you to another drug.
Are biosimilars as good as the original biologics?
Yes. Biosimilars are highly similar to the original drugs in structure, function, and effectiveness. Studies show they work just as well in reducing RA symptoms and preventing joint damage. The main difference is cost-they’re 15-30% cheaper. Many patients switch without any loss of benefit.
What are the biggest risks of biologic DMARDs?
The biggest risk is serious infections-like pneumonia, tuberculosis, or sepsis. Biologics suppress parts of your immune system, making it harder to fight off germs. Other risks include injection site reactions, increased risk of certain cancers (especially with JAK inhibitors), and rare cases of nervous system disorders. Your doctor will screen you for TB and monitor you closely.
Do I have to stay on biologics forever?
Most patients stay on them long-term. Stopping often leads to flare-ups. But some who achieve deep, lasting remission may try to taper under close supervision. This is risky and only done in rare cases with expert guidance. Never stop on your own.
Can I take biologics with methotrexate?
Yes, and often you should. Combining a biologic with methotrexate works better than either alone. Methotrexate reduces the chance your body will make antibodies against the biologic, which can make it less effective. Most rheumatologists start patients on both unless there’s a strong reason not to.
How do I know which biologic is right for me?
There’s no one-size-fits-all. Your doctor will consider your symptoms, lab results (like CRP and anti-CCP), past treatment history, infection risk, lifestyle, and cost. If you’ve failed one TNF inhibitor, switching to a non-TNF biologic like abatacept or tocilizumab often works better. Newer tools like synovial tissue analysis are starting to guide choices, but most decisions are still based on experience and trial.






Doreen Pachificus
My mom’s been on adalimumab for five years. She went from needing a cane to gardening again. No drama, no hype-just real life back.
Vicki Yuan
One thing no one talks about enough: the emotional toll of waiting for insurance approval. I spent three weeks in pain while they argued over biosimilars. The system isn’t broken-it’s just indifferent. If you’re fighting this, you’re not alone.
Also, side effects? Yeah, I got a nasty rash after the third shot. But my hands don’t look like sausages anymore. Trade-offs, people.
And yes, combining with methotrexate? Absolute game-changer. My rheumy said it cuts antibody formation by half. Don’t skip it unless you have a solid reason.
ArthritisPower? I track everything. My doctor actually uses my data to adjust doses. It’s weirdly empowering.
Also, the twice-yearly tocilizumab trial? I’m signed up. Fewer shots = fewer panic attacks at the pharmacy.
Akshaya Gandra _ Student - EastCaryMS
hey i just found out my aunt is on rituximab and shes like 70 and shes hiking now?? i thought biologics were only for young people??
Ethan Purser
Let me tell you something about hope. It’s not some fluffy, feel-good word. It’s the reason I didn’t jump off the bridge when I was 29 and couldn’t button my shirt. Biologics didn’t fix me-they gave me the space to fix myself.
People say, ‘It’s just a drug.’ No. It’s the difference between being a patient and being a person. Between watching life through a fog and stepping into sunlight.
I’ve had three infections since starting. One was pneumonia. I nearly died. But I’d do it again. Because on the days I can’t feel my fingers? I still feel the grass. Still feel the wind. Still feel alive.
And yeah, the cost? I sold my car. I took a second job. I cried in the pharmacy parking lot. But I didn’t cry because I was broke. I cried because I realized I’d rather be poor and mobile than rich and paralyzed.
This isn’t medicine. This is rebellion. Against time. Against decay. Against the quiet assumption that chronic pain is just part of life.
I don’t want a cure. I want to keep walking. And biologics? They let me do that.
So if you’re scared? Good. Be scared. But don’t wait. The clock’s ticking. And your joints? They don’t care about your fear.
Also, biosimilars? I switched. Saved $200 a month. Same results. Why pay more for the same thing? Capitalism is a scam. But this? This is survival.
And to the doctors who dismiss us as ‘non-compliant’? We’re not lazy. We’re exhausted. We’re scared. We’re trying. So please-listen.
Angie Rehe
As a rheumatology NP with 14 years in clinic, let me dismantle the myth that ‘biologics are magic.’ They’re not. They’re immunosuppressants with black box warnings. You’re trading infection risk for mobility. That’s not hope-that’s calculated risk management.
And the ‘remission’ narrative? Misleading. Most patients aren’t in true remission-they’re in low disease activity. The ACR criteria are too lenient. I’ve seen patients with DAS28 2.1 still have synovitis on ultrasound.
And JAK inhibitors? They’re not ‘oral biologics.’ They’re small molecules. Don’t conflate them. The FDA warning isn’t a footnote-it’s a siren. Especially for smokers, diabetics, or anyone over 50.
Also, ‘switching works’? Only if you haven’t exhausted all classes. After three biologics? Response rates plummet below 15%. That’s not failure-it’s biology. Stop pretending this is linear.
And biosimilars? They’re fine. But the real issue? Insurance gatekeeping. I’ve had patients wait 8 weeks for prior auth. Eight weeks. Their joints are eroding. This isn’t healthcare. It’s bureaucratic torture.
And yes, methotrexate combo? Mandatory. Without it, anti-drug antibodies form. You’ll lose efficacy. Period. Stop listening to Reddit gurus who say ‘I did it solo.’
If you’re reading this and thinking ‘I’ll just wait and see’-you’re gambling with your future. RA doesn’t pause. It doesn’t care about your timeline.
Aaron Mercado
YOU PEOPLE ARE ALL IGNORANT. I’VE BEEN ON HUMIRA FOR 8 YEARS. I’VE HAD TWO PNEUMONIAS. I’VE LOST MY JOB BECAUSE I COULDN’T WORK. I’VE BEEN DENIED INSURANCE THREE TIMES. AND STILL-I’M ALIVE. I’M WALKING. I’M NOT IN A WHEELCHAIR. YOU THINK YOU KNOW PAIN? YOU DON’T. YOU’RE JUST CLICKING ‘LIKE’ ON SOME BLOG POST.
THEY WANT YOU TO THINK IT’S ‘HOPE.’ IT’S NOT. IT’S SURVIVAL. AND IF YOU’RE NOT WILLING TO PAY THE PRICE? THEN STAY OFF MY THREAD.
AND YES-I STILL CRY WHEN I SEE MY KIDS RUN. BECAUSE I THOUGHT I’D NEVER SEE THAT AGAIN.
Vikram Sujay
While the clinical efficacy of biologic DMARDs is well-documented, the philosophical implications of their use warrant deeper reflection. The transformation of rheumatoid arthritis from a degenerative condition into a manageable chronic disease represents not merely a medical advancement, but a redefinition of human resilience.
It is worth noting that the pursuit of remission-though laudable-may inadvertently reinforce a biomedical paradigm that privileges physical functionality over holistic well-being. The emotional labor of self-injection, insurance battles, and constant vigilance against infection is rarely accounted for in outcome metrics.
Moreover, the global disparity in access raises ethical questions: while one patient may switch to a biosimilar for $120/month, another in rural India may never access even a csDMARD. The promise of personalized medicine must not become a luxury reserved for the economically privileged.
Yet, in the quiet dignity of patients who continue to walk, write, and love despite their condition, we witness not just pharmacological triumph, but the enduring spirit of the human will.
I encourage all who engage with this topic to move beyond statistics and consider the lived experience behind each DAS28 score.
Uzoamaka Nwankpa
I’m from Nigeria. We don’t have these drugs here. My sister has RA. She takes paracetamol and sits in pain all day. No one even knows what a biologic is. They say it’s ‘Western medicine’ and she’s ‘just old.’
It’s not fair. I read this and I cry. Not because I’m weak. Because I’m powerless.