Managing bipolar disorder isn’t about finding one magic pill. It’s about balancing effectiveness with everyday life - and that balance shifts for every person. For millions in the U.S., mood stabilizers and antipsychotics are the backbone of treatment, but they come with trade-offs that aren’t always talked about in doctor’s offices. If you’ve ever felt like your medication is doing more harm than good, you’re not alone. About 40% of people stop taking their bipolar meds within a year, mostly because of side effects like weight gain, constant thirst, or brain fog.
What Mood Stabilizers Actually Do
Mood stabilizers like lithium, valproate, carbamazepine, and lamotrigine aren’t designed to make you feel ‘normal’ all the time. They’re meant to stop the extreme swings - the deep depressions and the wild manias - from taking over your life. Lithium, approved by the FDA back in 1970, is still the most studied. It doesn’t just calm mania; it reduces suicide risk by 80% compared to no treatment. That’s not a small number. It’s life-saving.
But lithium isn’t simple. You need regular blood tests to make sure your levels are in the sweet spot: 0.6 to 1.0 mmol/L for maintenance, and up to 1.0 for acute episodes. Go above 1.2, and you risk toxicity - slurred speech, shaky hands, even seizures. That’s why weekly blood draws are standard at first. Once stable, you drop to every 2-3 months. Many patients say the constant monitoring feels exhausting. But skipping it can be dangerous.
Side effects are common. Around 30-40% of people on lithium report needing to pee constantly. Some drink three liters of water a day and still feel dehydrated. Hand tremors affect nearly half. Weight gain averages 10-15 pounds in the first year. Nausea? That’s not rare either. One Reddit user wrote: “I was drinking water like it was my job. I still felt dry inside.”
Lamotrigine is different. It’s the go-to for bipolar depression, not mania. It’s less likely to cause weight gain - a big plus. But it comes with its own risk: a serious skin rash in about 10% of users. That’s why doctors start low - 25mg a week - and creep up slowly. If you get a rash, stop immediately. No exceptions.
Antipsychotics: Faster Relief, Heavier Costs
Antipsychotics like quetiapine (Seroquel), olanzapine, and aripiprazole weren’t originally made for bipolar disorder. But they’ve become first-line tools, especially for acute episodes. Why? Because they work faster. While lithium can take two weeks to show real improvement, quetiapine often starts helping in just seven days.
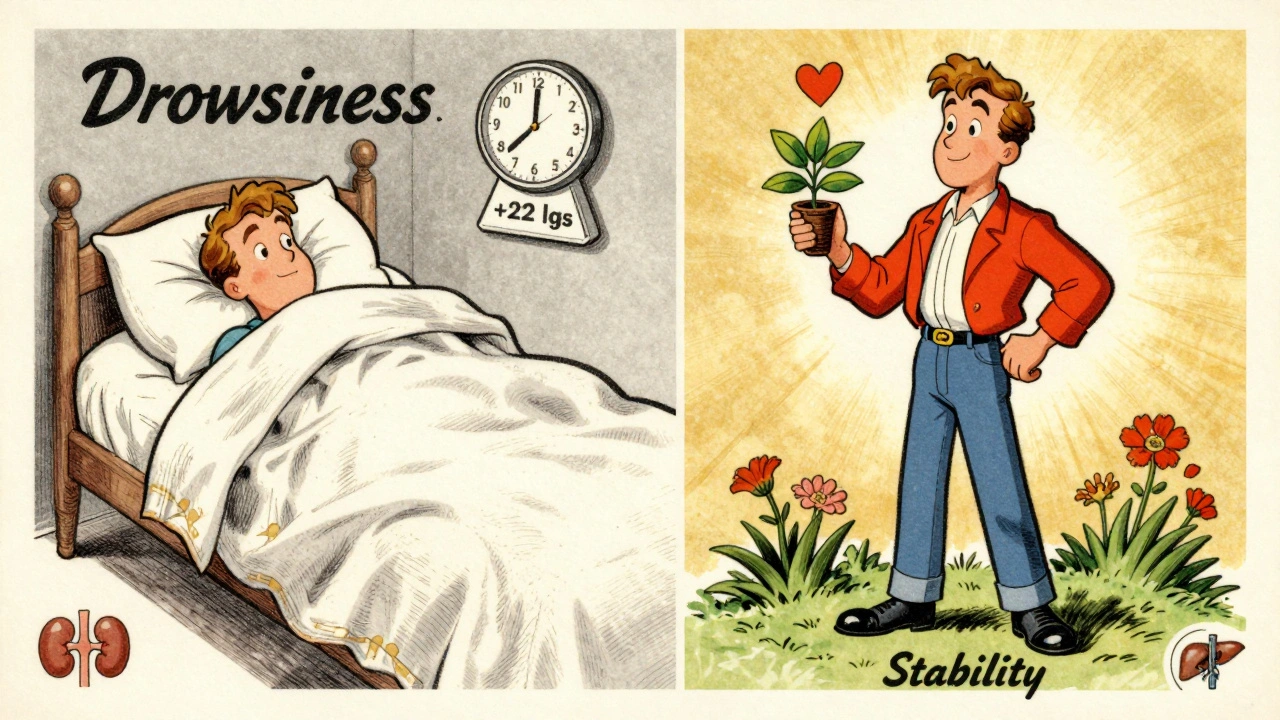
Quetiapine is the most commonly prescribed for bipolar depression. Studies show a 50.3% response rate - nearly double the placebo. But here’s the catch: 60-70% of people feel drowsy. Many say they can’t get out of bed until noon. Weight gain is another major issue. On average, users gain 22 pounds. Olanzapine? Even worse. It can cause a 4.6kg (10-pound) gain in just six weeks. And that’s not just cosmetic. It raises diabetes risk by 20-30%.
Patients on PatientsLikeMe rated quetiapine 3.7 out of 5 for effectiveness - but only 2.8 for tolerability. That gap tells you everything. You might feel better emotionally, but your body feels like it’s under siege. One user shared: “I stopped working out because I was too tired. Then I gained 30 pounds. I felt like I lost myself.”
Aripiprazole and lurasidone are newer options with better metabolic profiles. Lurasidone, approved in 2023 for bipolar depression, causes only 0.8kg of weight gain in six weeks - compared to 3.5kg with quetiapine. That’s why experts now recommend it as a first-line choice for depression. But it’s expensive. Brand-name versions cost over $1,200 a month. Generic lithium? $4 to $40.
Combination Therapy: When One Pill Isn’t Enough
Many people need more than one medication. About 70% of treatment-resistant cases respond when a mood stabilizer is paired with an antipsychotic. But combining them isn’t a free pass. Side effects pile up. You might get the mood control you need - but also dizziness, dry mouth, high cholesterol, and sexual dysfunction. One survey found 52% of patients reported sexual side effects from these combos.
Doctors often start with lithium or lamotrigine, then add quetiapine if depression lingers. Or they’ll use aripiprazole to manage mania while keeping lamotrigine for the lows. The goal isn’t to blanket the brain with drugs. It’s to find the minimum effective mix. Too many meds? You’re trading one problem for another.
What About Antidepressants?
This is where things get controversial. Antidepressants like fluoxetine or sertraline are sometimes used for bipolar depression. But they carry a real risk: triggering mania. Studies show 10-15% of people switch into a manic episode when taking an antidepressant alone. That’s why experts insist they should never be used without a mood stabilizer.
Some doctors, like Dr. Gary Sachs from Harvard, warn against them entirely. Others, like Dr. David Miklowitz at UCLA, say they’re okay if used carefully with lithium or valproate. The truth? There’s no universal answer. It depends on your history. If you’ve ever had a manic episode after an antidepressant, you’re probably not a candidate.
Monitoring: The Unseen Part of Treatment
Medication management isn’t just about prescriptions. It’s about tracking. The American Psychiatric Association recommends quarterly checks for:
- Weight and waist circumference (over 40 inches for men, 35 for women signals metabolic risk)
- Fasting blood sugar
- Lipid panel (cholesterol and triglycerides)
- Thyroid and kidney function (especially if you’re on lithium)
Many patients don’t realize these tests are non-negotiable. A 2022 NAMI survey found 45% of people stopped meds because they didn’t know how to manage side effects. They didn’t know metformin could help with weight gain. They didn’t know splitting lithium doses (morning and night) could reduce nausea. They didn’t know NSAIDs like ibuprofen could push lithium into toxic range.
One simple tip from real users: take lithium with food. It cuts nausea by half. Another: drink water consistently - not just when you’re thirsty. Lithium makes your body lose water faster. Dehydration raises toxicity risk.

The Real Cost: Money, Time, and Mental Energy
Bipolar disorder affects 5.7 million adults in the U.S. The average yearly cost of meds is $1,200. But that’s not the full picture. You’re also paying in time - weekly blood draws, monthly doctor visits, pharmacy trips, side effect management. And emotionally? The guilt of feeling like you’re failing because you can’t tolerate a drug that “works for others.”
Genetic testing is starting to change that. Companies like Genomind test for CYP2D6 and CYP2C19 gene variants - which affect how your body processes 40% of bipolar medications. In trials, this testing improved medication selection accuracy by 30%. It’s not mainstream yet, but it’s coming. By 2027, experts predict it’ll be standard.
Long-acting injectables like Abilify Maintena (aripiprazole) are another shift. One shot a month. No daily pills. For people who struggle with adherence, it’s a game-changer. But it’s not for everyone. You need to be stable first. And it still carries metabolic risks.
When It Works: The Stories They Don’t Tell You
Not every story is about side effects. There are people who found their peace.
One Reddit user with 85 upvotes wrote: “After three meds failed, lithium finally stabilized me. I gained 15 pounds. But I haven’t had a suicidal episode in two years. That’s worth it.”
Another said: “Lamotrigine gave me my mind back. No fog. No weight gain. Just steady. I can work. I can parent. I can breathe.”
These aren’t outliers. They’re the reason this treatment exists. The goal isn’t perfection. It’s stability. It’s showing up for your life, even if you’re not 100%.
What’s Next? The Future of Bipolar Treatment
Research is moving fast. Lumateperone (Caplyta), approved in 2023, offers antidepressant effects without the weight gain. Ketamine derivatives are being tested for rapid depression relief - something current meds can’t do. Digital tools like reSET-BD, a smartphone app that tracks mood and reminds you to take meds, reduced relapse by 22% in trials.
But here’s the hard truth: only 35% of people with bipolar disorder reach full remission. Six in ten still struggle with side effects that interfere with daily life. That’s why the most important part of treatment isn’t the drug. It’s the conversation. With your doctor. With yourself. With your support system.
You’re not broken because you need help. You’re not weak because you had to switch meds three times. You’re doing the work. And that matters more than any pill ever could.
Can you take mood stabilizers and antipsychotics together?
Yes, many people take them together - especially if one medication alone isn’t enough. Combining a mood stabilizer like lithium with an antipsychotic like quetiapine can boost effectiveness to 70% in treatment-resistant cases. But side effects also increase by 25-30%. Doctors usually start with one, then add the other only if needed. Never combine without medical supervision.
How long does it take for lithium to work?
Lithium usually takes 1-3 weeks to show noticeable effects on mania, and up to 6 weeks for full mood stabilization. Unlike antipsychotics, it doesn’t offer quick relief. That’s why doctors often pair it with a fast-acting antipsychotic during acute episodes. Blood levels must be monitored closely during this time to avoid toxicity.
Do antipsychotics cause permanent weight gain?
Weight gain from antipsychotics isn’t always permanent, but it often is if not managed. Olanzapine and quetiapine are the worst offenders. Some people gain 10-30 pounds in months. But with lifestyle changes - diet, exercise, and sometimes metformin - many can stabilize or even lose weight. The key is early action. Waiting six months makes it much harder to reverse.
Can you stop taking these meds if you feel better?
Stopping abruptly is dangerous. Even if you feel fine, stopping can trigger a relapse - sometimes worse than before. Studies show 80% of people who quit meds without medical guidance have a new episode within a year. If you want to reduce or stop, work with your doctor on a slow taper plan. Never do it on your own.
Is there a better alternative to lithium?
Lithium remains the most effective for long-term suicide prevention and preventing mania. But alternatives like valproate or lamotrigine may be better for people who can’t tolerate lithium’s side effects. Lamotrigine is especially good for depression with minimal weight gain. Newer antipsychotics like lurasidone and cariprazine are now first-line for depression due to better metabolic profiles. The best choice depends on your symptoms, history, and tolerance.
How often should I get blood tests?
When starting lithium, you’ll need blood tests weekly for the first month, then every 2-3 months once stable. For antipsychotics, metabolic checks (blood sugar, cholesterol, weight) should happen every 3 months. If you’re elderly or have kidney issues, your doctor may test more often. Skipping tests increases the risk of serious side effects - including kidney damage from lithium or diabetes from antipsychotics.
Can I drink alcohol while on these medications?
It’s not recommended. Alcohol can worsen sedation from antipsychotics like quetiapine and increase the risk of dizziness or falls. With lithium, alcohol can dehydrate you - which raises your lithium levels and pushes you toward toxicity. Even moderate drinking can interfere with mood stability. Most experts advise avoiding alcohol entirely during treatment.
What should I do if I miss a dose?
If you miss a dose of lithium or an antipsychotic, take it as soon as you remember - unless it’s close to your next scheduled dose. Never double up. Missing one dose usually won’t cause a crisis, but repeated missed doses can trigger mood episodes. Use pill organizers or phone alarms. Some people benefit from long-acting injectables to avoid daily dosing altogether.
Managing bipolar disorder with medication is a marathon, not a sprint. There’s no perfect drug. But there is a right path - one that’s tailored, monitored, and supported. You don’t have to suffer in silence. You don’t have to choose between feeling stable and feeling like yourself. With the right team and the right plan, you can have both.







Jay Everett
Man, I wish I’d known about the lithium + food trick years ago. Nausea cut in half? That’s a game-changer. I was on the verge of quitting because I felt like my stomach was staging a rebellion every morning. Now I eat a banana before my pill and suddenly I’m not crying in the bathroom anymore. 🙌
Shannara Jenkins
Thank you for writing this. So many people think it’s just ‘taking pills and being fine’-but it’s a daily negotiation between survival and self. You’re not broken for needing help. You’re brave for showing up anyway. 💛
Elizabeth Grace
I gained 40 lbs on quetiapine and felt like a ghost in my own body. Stopped cold turkey. Had a manic episode three weeks later. Now I’m on lurasidone + therapy. It’s not perfect, but I can see my face in the mirror again. 🥲
Lynn Steiner
Why do we keep pretending these drugs are ‘safe’? They’re chemical restraints with a side of diabetes. You’re not ‘managing’ bipolar-you’re surviving a pharmaceutical experiment. 🇺🇸
Steve Enck
The empirical data presented herein demonstrates a statistically significant correlation between metabolic dysregulation and second-generation antipsychotic administration, particularly in the context of prolonged therapeutic exposure. Moreover, the absence of standardized biomonitoring protocols across primary care settings constitutes a critical systemic failure in psychiatric pharmacovigilance. One must also consider the epistemological dissonance between patient-reported quality-of-life metrics and clinician-derived efficacy benchmarks. The reductionist model of pharmacological intervention fails to account for the phenomenological complexity of affective dysregulation.
मनोज कुमार
Lithium blood levels need to be tight 0.6-1.0 anything over 1.2 is toxic stop pretending its safe
Joel Deang
bro i took lamotrigine and my skin started itching like crazy and i thought it was just dryness but then i saw the rash and panicked. i stopped right away. never knew it could be that serious. thanks for the heads up. 🙏
Alicia Marks
You’re not alone. And you’re doing better than you think.
Paul Keller
It is worth noting that the current paradigm of pharmacological intervention in bipolar disorder remains fundamentally inadequate when viewed through the lens of neuroplasticity and neuroinflammation. The overreliance on monoaminergic modulation ignores emerging evidence implicating glial dysfunction and mitochondrial impairment in mood dysregulation. While lithium remains the gold standard for suicide prevention, its mechanism of action-GSK-3β inhibition, inositol depletion, and BDNF upregulation-is grossly oversimplified in public discourse. We must move beyond symptom suppression toward disease-modifying strategies. The future lies in precision psychiatry, not pill cocktails.
dave nevogt
I’ve been on lithium for 12 years. I’ve had the tremors, the thirst, the weight gain. I’ve cried in the bathroom after blood draws. But I’ve also held my daughter when she was scared. I’ve shown up for my job. I’ve written songs. I’ve lived. The pills aren’t perfect. But they gave me back my life. Not the one I imagined. The one I could actually have.
Arun kumar
in india we dont even get access to lamotrigine its too expensive and doctors just give valproate and olanzapine and say take it
Zed theMartian
Oh look, another ‘meds are magic’ fairy tale from the psychiatric-industrial complex. You’re not ‘managing’ bipolar-you’re being chemically pacified to fit into a capitalist machine that has zero tolerance for emotional depth. The real treatment? Quit your job. Move to the woods. Stop taking your meds. Let the storm rage. You might just find out who you are when the pills are gone.
Ella van Rij
Oh honey, you mean besides the 10+ lbs of weight gain, the brain fog that makes you forget your own name, and the fact that you can’t orgasm anymore? Yeah, I’m sure that’s ‘worth it.’ 💅
ATUL BHARDWAJ
lithium cheap and works if you test