Every year, medication errors send over 1.5 million Americans to the hospital-many of them because of simple mistakes made at home. It’s not about being careless. It’s about confusion, fatigue, poor labeling, and information overload. You’re not alone if you’ve ever stared at a pill bottle wondering, Did I take this already? or Is this the same as last week’s bottle? These aren’t rare blunders. They happen in nearly every household with someone on regular meds, especially kids, seniors, and people juggling multiple prescriptions.
What Are the Most Common Medication Mistakes?
At home, the biggest errors aren’t usually about taking the wrong drug entirely. They’re subtle, quiet, and often invisible until something goes wrong.
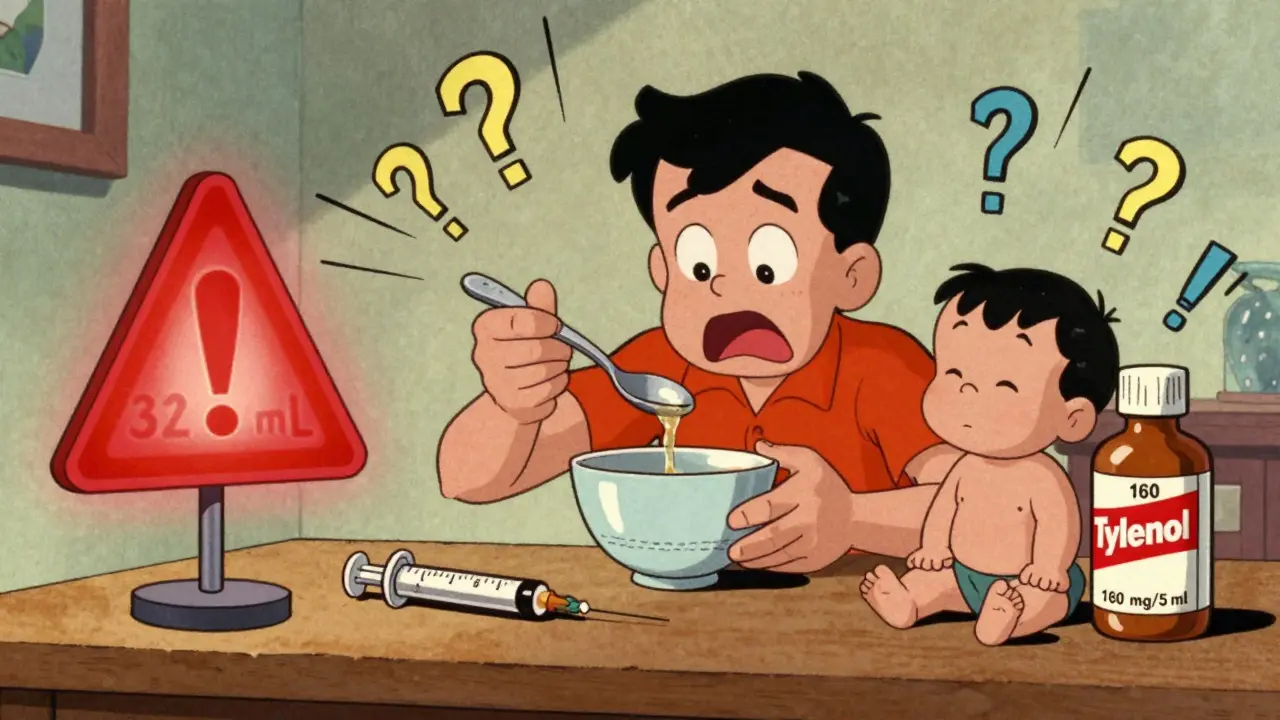
- Wrong dose: Giving too much or too little. This is the #1 error. Parents often mix up infant and children’s Tylenol because one is more concentrated. Seniors might cut pills in half without knowing the dosage isn’t evenly split.
- Missed doses: Skipping pills because you forgot, felt better, or couldn’t afford them. One study found that nearly 93% of parents gave fewer antibiotic doses than prescribed for their kids’ ear infections.
- Wrong timing: Taking meds at the wrong time of day-like sleeping pills at breakfast or blood pressure meds with dinner instead of morning. Food interactions matter too. Some drugs need an empty stomach; others need food to absorb properly.
- Double-dosing: Taking an extra pill because you think you missed one. Or worse-taking two different cold medicines that both contain acetaminophen. That’s how liver damage starts.
- Keeping old meds: Continuing prescriptions after they’re discontinued. A 2023 NCBI study showed that 38% of people over 75 still take drugs their doctor told them to stop.
- Confusing brand and generic names: Taking both “Lipitor” and “atorvastatin,” thinking they’re different. They’re the same drug.
For kids, the risks are even sharper. A child suffers a medication error at home every 8 minutes. Most of these happen because parents confuse concentrations-infant Tylenol is 3x stronger than children’s Tylenol. Mixing acetaminophen and ibuprofen for fever also increases error risk by 47%, according to pediatric research from UC Davis.
Why Do These Mistakes Keep Happening?
It’s not just memory lapses. The system is set up to fail.
Healthcare providers often give instructions too fast. Patients leave the office remembering only 20-40% of what was said. That’s not your fault. Studies show that over 80% of people misremember key details about their meds after a doctor’s visit.
Then there’s the clutter. Pill bottles with tiny print. Multiple doctors prescribing different drugs. No one keeps a full list. Pharmacies label things differently. One bottle says “take once daily,” another says “take every 24 hours.” Are those the same? You’re left guessing.
Look-alike, sound-alike drugs are another silent killer. “Hydralazine” and “hydroxyzine” look similar. One treats high blood pressure. The other treats anxiety. Mix them up? Dangerous.
Cost plays a role too. People skip doses because they can’t afford refills. Others cut pills to stretch supplies. But not all pills can be safely split. Extended-release tablets, for example, become toxic if crushed.
And let’s not forget language barriers, low health literacy, and rushed caregivers. A grandmother caring for her grandchild might not speak English well. A working parent might be exhausted after a 12-hour shift. In those moments, mistakes happen-not because anyone’s dumb, but because the system doesn’t support them.
How to Stop Medication Errors Before They Start
Prevention isn’t about memorizing every pill. It’s about building simple, repeatable systems.
- Keep a real-time medication list. Write down every drug you take-brand name, generic name, dose, time, reason. Include vitamins, supplements, and over-the-counter stuff. Update it every time your doctor changes something. Keep a copy in your wallet and share it with every provider.
- Use a pill organizer with alarms. Not the cheap kind with 7 compartments. Get one with labeled times (morning, noon, night, bedtime) and a timer that beeps. Some even connect to your phone. Set reminders for every dose. Don’t rely on memory.
- Ask for the teach-back method. When your doctor or pharmacist explains your meds, say: “Can you please explain how I’m supposed to take this so I can repeat it back?” If you can’t say it clearly, you don’t understand it yet.
- Check concentrations, especially for kids. Always look at the label: “32 mg/mL” vs. “160 mg/5 mL.” Never guess. Use the dosing syringe that comes with the bottle-not a kitchen spoon. A teaspoon varies by up to 20%.
- Never mix fever reducers unless directed. Don’t alternate Tylenol and Advil unless your pediatrician says so. It’s tempting, but it increases confusion and overdose risk.
- Dispose of old meds properly. Don’t keep expired or discontinued drugs in the medicine cabinet. Use a drug take-back program or follow FDA disposal guidelines. Out-of-date meds can lose potency or become unsafe.
- Know your drug interactions. Grapefruit juice can wreck the effect of statins. Antacids can block absorption of antibiotics. Ask your pharmacist: “What should I avoid while taking this?”
- Get one pharmacy. Using multiple pharmacies means no one sees your full list. One pharmacy can flag dangerous combinations.
Special Cases: Kids and Seniors
Children under 6 are the most vulnerable. Their bodies process drugs differently. A dose that’s safe for a 40-pound child could kill a 20-pound baby. Always dose by weight, not age. Keep all meds out of reach-even “harmless” ones like children’s Benadryl.
For seniors, the risk spikes with every additional drug. Taking five or more medications increases error risk by 30%. Many seniors get prescriptions from multiple specialists who don’t talk to each other. That’s why medication reconciliation is critical. Before leaving the hospital or clinic, ask: “Can you please review every drug I’m taking and tell me what to keep, stop, or change?”
Also, watch for signs of confusion. Forgetting to take meds, taking them twice, or mixing up names can be early signs of cognitive decline. Don’t assume it’s just aging. Talk to a doctor.
What to Do If You Think You Made a Mistake
If you gave the wrong dose, skipped a day, or took something you shouldn’t have:
- Don’t panic. Don’t try to fix it by giving another dose.
- Call your pharmacist immediately. They’re trained to handle this.
- If it’s a child, a senior, or a high-risk drug (like blood thinners or insulin), call Poison Control at 1-800-222-1222. They’re free, 24/7, and confidential.
- Write down what happened-what drug, how much, when, and why. This helps professionals give better advice.
Most errors don’t cause harm-but they can. And the only way to prevent the next one is to learn from the last one.

Tools That Actually Help
There are free, easy tools that make a real difference:
- My Meds List (from the FDA): Downloadable PDF to track all your meds. Print it, fill it out, carry it.
- Medisafe or MyTherapy: Free apps that send alerts and track adherence. Some even notify family members if you miss a dose.
- Health Literacy Universal Precautions Toolkit (AHRQ): Free guides for patients and caregivers on how to ask better questions and understand instructions.
- Drug Interaction Checker (available on WebMD or Medscape): Type in all your meds and see what clashes.
These aren’t magic. But they turn guesswork into structure. And structure saves lives.
Final Thought: You’re Not Alone
Medication errors aren’t a sign of failure. They’re a sign that the system is broken-not you. Millions of people make these mistakes. The goal isn’t perfection. It’s awareness. It’s asking for help. It’s writing things down. It’s double-checking labels. It’s saying, “I’m not sure-can you show me again?”
One small change-like using a pill organizer or keeping a written list-can cut your risk by half. Start there. Don’t wait for a crisis. Medication safety isn’t about being perfect. It’s about being prepared.
What’s the most common medication error at home?
The most common error is giving the wrong dose-either too much or too little. This includes confusing infant and children’s concentrations of acetaminophen, skipping doses due to cost or forgetfulness, or taking extra doses because you think you missed one. Nearly 33% of home medication administrations involve some kind of dosing error.
Can I cut my pills in half to save money?
Only if the pill is scored and your doctor or pharmacist says it’s safe. Many pills, especially extended-release or enteric-coated ones, shouldn’t be split. Cutting them can change how the drug is absorbed, leading to underdosing or dangerous spikes. Always ask before splitting.
Why do I keep mixing up my meds?
Look-alike and sound-alike names, poor labeling, multiple prescriptions, and stress all contribute. Many bottles look identical. One might say “Metoprolol,” another “Metformin.” Use a pill organizer with clear labels and keep a written list. Never rely on bottle shape or color.
Is it safe to give my child Tylenol and Advil together for fever?
No-not unless your pediatrician specifically tells you to. Alternating acetaminophen and ibuprofen increases the chance of dosing errors by 47%. It also makes it harder to track how much your child has taken. Stick to one and follow the weight-based dosing chart on the label.
What should I do if I accidentally give too much medicine?
Call Poison Control immediately at 1-800-222-1222. Do not wait for symptoms. Do not try to induce vomiting. Have the medicine bottle handy when you call. They’ll tell you whether to go to the ER or wait. For children, seniors, or high-risk drugs like blood thinners or insulin, never delay.
How can I make sure my elderly parent takes meds safely?
Use a daily pill organizer with alarms. Keep a written list of all meds and update it after every doctor visit. Ask the pharmacist to review all prescriptions for interactions. If they’re on five or more drugs, request a medication reconciliation from their primary care provider. Watch for signs of confusion-like forgetting doses or taking them twice.
Do I really need to throw away old medications?
Yes. Expired drugs can lose effectiveness or become unstable. Keeping them increases the risk of accidental use-especially by children or confused seniors. Use a drug take-back program at a pharmacy or police station. If none is available, mix pills with coffee grounds or cat litter, seal them in a bag, and throw them in the trash. Never flush unless the label says to.
Can I use a kitchen spoon to measure liquid medicine?
Never. A kitchen teaspoon holds anywhere from 3 to 7 milliliters-far from accurate. Always use the dosing syringe or cup that comes with the medicine. If it’s missing, ask your pharmacist for one. They’re free.
Next Steps: What to Do Today
Don’t wait for a mistake to happen. Take action now:
- Grab your medicine cabinet. Pull out every bottle-prescription, OTC, vitamins.
- Write down every drug, dose, and time you take it. Include why you take it.
- Compare your list to what your doctor thinks you’re taking. Are they the same?
- Throw out expired or unused meds using safe disposal methods.
- Buy a pill organizer with alarms and fill it for the next week.
- Ask your pharmacist: “Are there any look-alike drugs I’m taking? Is there a simpler way to take these?”
One small step today can prevent a hospital visit tomorrow. Medication safety isn’t complicated. It’s just consistent.






Kirstin Santiago
My grandma uses a pill organizer with alarms now and it’s changed everything. She used to mix up her blood pressure meds and would get dizzy for days. Now she gets a beep at 8am and 8pm and even texts my mom if she misses one. Small thing, huge difference.
Also started keeping a written list in her wallet. Doctor finally saw it and caught she was still taking a statin she’d been told to stop last year. Turned out it was a miscommunication. Saved her from a potential fall.
Don’t underestimate the power of writing stuff down. It’s not fancy but it works.
And please, no kitchen spoons. I’ve seen people use them for kids’ Tylenol. It’s terrifying.
Anjula Jyala
Wrong dose is #1 error because people are lazy and don’t read labels. Pediatric formulations are not interchangeable. 32mgmL vs 160mg5mL is not a suggestion it’s a death sentence. Stop assuming you know what you’re doing. Get the syringe. Use it. Period
Marian Gilan
They dont want you to know this but pharmacies are paid to push brand names even when generic is fine. Thats why you get confused. And the pills look the same on purpose so you keep buying. Also the FDA is in bed with Big Pharma. They dont care if you mix up hydralazine and hydroxyzine. They just want you to refill. I found out my blood pressure med was switched without telling me. Took me 3 months to catch it. They dont want you to be smart
Paul Taylor
People think they can wing it with meds because theyve done it for years but the body changes. Your liver slows down. Your kidneys dont filter like they used to. What was safe at 50 is dangerous at 70. And no one tells you that.
I used to cut my pills to save money. Thought I was being smart. Turns out my extended-release melatonin was getting crushed into a powder. I was getting hit with a full dose every time. Woke up at 3am feeling like I’d been hit by a truck.
Now I use a pill splitter only for scored pills and I check with the pharmacist every time. Even if youve been on the same med for 15 years. Ask. Always ask.
And dont get me started on supplements. People take 10 different ones and think its harmless. Some of them interact with blood thinners. I had a friend almost bleed out because he was taking ginkgo and warfarin. No one told him it was a problem.
Medication safety isnt about being perfect. Its about being curious. Its about asking one more question. Even if you feel silly. Even if you think you know it all. You dont. None of us do.
Kegan Powell
Honestly this post made me cry 😭 I used to be the person who mixed up my meds every week. Thought I was fine. Then my mom had a stroke and I had to manage her whole regimen. I realized I had no idea what half the pills were for. I thought Lipitor and atorvastatin were different. I was so embarrassed. But then I started using MyTherapy app and it changed my life. Now I get alerts and even a weekly summary email. I print it out and bring it to every appointment. My doctor says I’m the most prepared patient he’s ever had. It’s not about being perfect. It’s about showing up. And you can show up even if you’re scared or tired or confused. You just need one tool. One system. One person to help you. You’re not alone. 💪❤️
Harry Henderson
If you’re still using a kitchen spoon to measure medicine you deserve to lose your kid. No excuses. No sympathy. You are not a victim of the system. You are a negligent parent. Get the syringe. Buy a pill organizer. Stop being lazy. This isn’t rocket science. It’s basic parenting. If you can’t handle it then don’t have kids. Simple.
suhail ahmed
Man this hits different when you’re the one doing the caregiving. I’ve been looking after my uncle for two years now. He’s on 11 meds. Some from three different docs. I used to just wing it until one day he started slurring and couldn’t stand up. Turned out he was double-dosing on a blood thinner because two bottles looked the same. One said ‘warfarin 5mg’ the other ‘warfarin 2.5mg’ - same color, same shape, same font. I nearly lost him.
Now we use color-coded stickers. Red for morning, blue for night. We take a pic of every bottle and label it on our phone. We use a pillbox with 7 days and four slots. And we call the pharmacy every time a new script comes in - ‘Hey, can you confirm this is the same as last month?’
It’s exhausting. But it’s better than burying someone because you didn’t ask a question.
Also - never trust the label on the bottle. Always check the script. Always. The pharmacy printed ‘take with food’ on a med that’s supposed to be taken empty. We caught it because I compared it to the doctor’s note.
System’s broken? Yeah. But we’re not powerless. We just gotta be the ones to fix it - one pill at a time.
Candice Hartley
I used to mix up my thyroid med and my anxiety med. Same size. Same color. Same bottle shape. One morning I took the wrong one and felt like I was having a panic attack. Turned out I’d taken my anxiety pill instead of my thyroid. Took me 2 hours to realize. Now I keep them in different drawers. And I write the purpose on the cap with a Sharpie. Small thing. Big safety net. 🙏
astrid cook
I just found out my neighbor’s 8-year-old almost died because she gave him children’s Tylenol thinking it was the same as infant. She didn’t even know the concentrations were different. I told her she should’ve read the label. She cried and said she was exhausted. I didn’t feel bad. If you’re too tired to read a label, you shouldn’t be giving meds to a child. This isn’t hard. It’s basic. And people are dying because they don’t care enough to try.
Kathy McDaniel
i just started using a pill organizer and honestly it’s been a game changer. i used to forget if i took my blood pressure pill or not and would take it twice. now i just look at the box and if it’s empty i know i took it. also threw out all my old meds and got a free disposal bag from the pharmacy. felt so good to clean out that cabinet. 🌿
Patrick Merrell
They don’t want you to know that most medication errors are caused by pharmacies switching generics without telling you. I’ve had the same prescription for 7 years. Last year they switched the maker. The pill looked different. I didn’t question it. I got dizzy for three weeks. Turns out the inactive ingredients were triggering migraines. No one warned me. No one cared. This isn’t about you being careless. It’s about corporations playing Russian roulette with your life.
Murphy Game
I work in a hospital pharmacy. I’ve seen it all. People bring in 17 different meds from 5 different doctors. No one has a list. No one knows what’s what. We have to call each doctor to figure out what’s still active. Sometimes the patient is in the ER because they took 3 different painkillers that all had acetaminophen. They’re in liver failure. And their family says, 'But we thought they were different!' No. You just didn’t read the tiny print. You didn’t ask. You didn’t care. This isn’t a system failure. It’s a human failure. And you’re part of it.