When your knee, shoulder, or hip suddenly locks up with sharp pain-swollen, hot, and impossible to move-you might hear your doctor say, "Let’s try a cortisone shot." It’s one of the most common treatments for joint pain in the U.S., with 10 million injections given every year. But what exactly is happening inside your joint when that needle goes in? And why does the relief sometimes last weeks… and other times vanish after just a few days?
How Corticosteroid Injections Actually Work
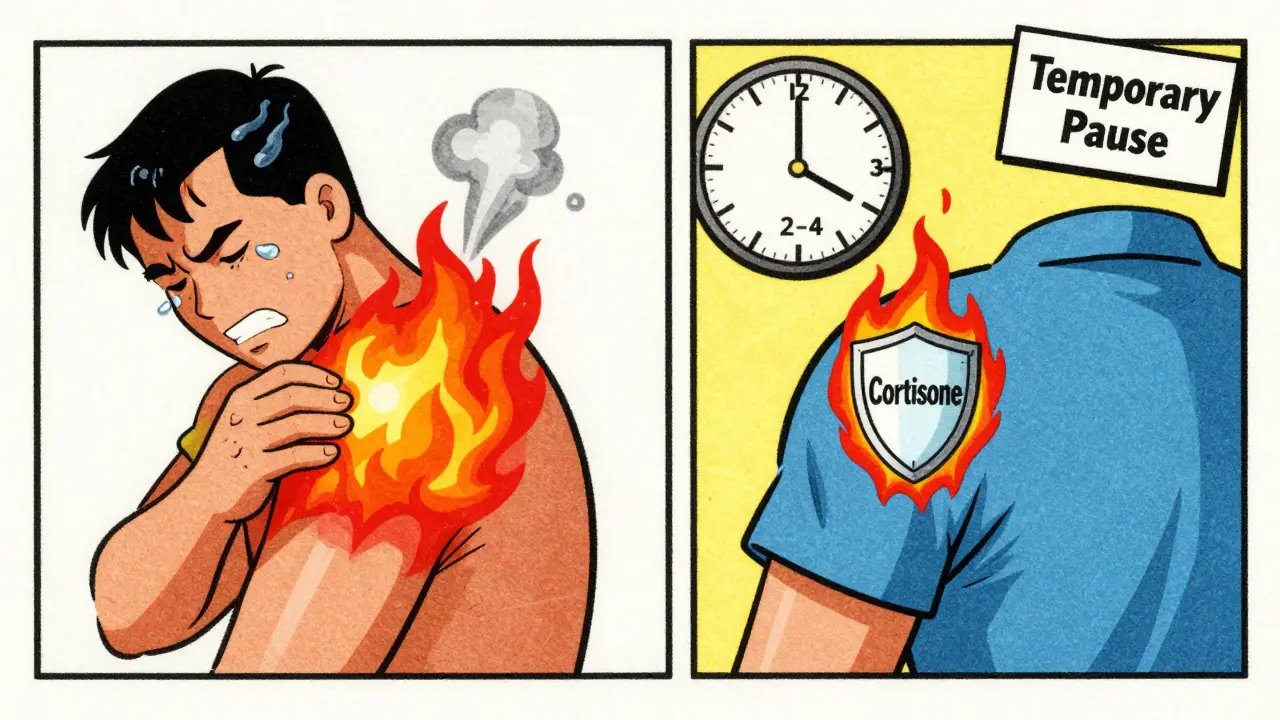
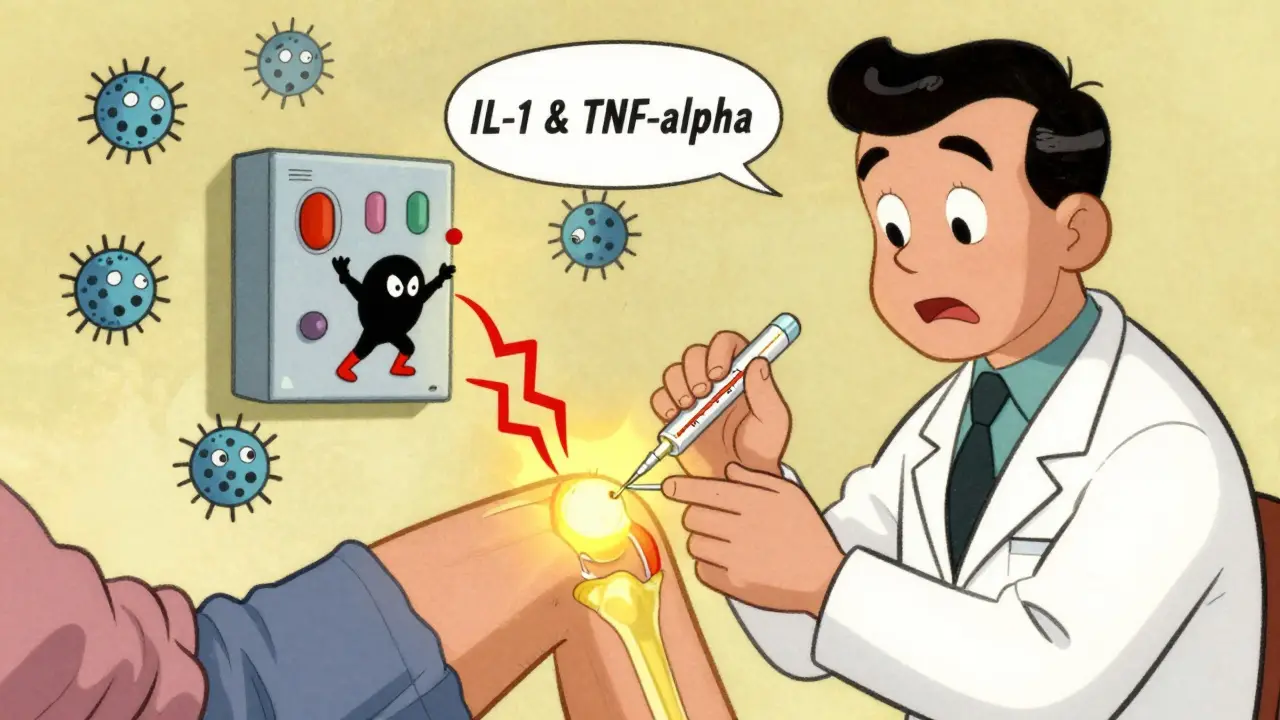
Corticosteroid injections aren’t painkillers like ibuprofen. They don’t numb the area. Instead, they’re powerful anti-inflammatory drugs that target the root cause of your discomfort: swelling. When a joint is inflamed, your body releases chemicals like interleukin-1 and tumor necrosis factor-alpha. These turn on pain signals, attract white blood cells, and break down cartilage over time. Corticosteroids like triamcinolone or methylprednisolone slip into your joint cells and shut down this whole chain reaction.
They do this by binding to receptors inside your cells, then traveling to the nucleus to block the genes that make those inflammatory chemicals. They also calm down neutrophils-immune cells that swarm inflamed joints-and reduce the stickiness of the synovial lining, which helps stop fluid buildup. The result? Less heat, less swelling, less pressure on nerves. Pain drops. Often within 24 to 72 hours.
Most injections combine the corticosteroid with a local anesthetic like lidocaine. That’s why you might feel instant relief right after the shot-it’s the numbing agent. But that fades in a few hours. The real magic happens later, when the steroid kicks in.
Which Joints Get Injections-and How Much?
Not all joints are treated the same. The dose depends on size and location:
- Knee: 40-80 mg of triamcinolone or methylprednisolone
- Shoulder: 20-40 mg
- Wrist or ankle: 10-20 mg
- Finger or toe: 5-10 mg
Smaller joints need less because they have less space and fewer tissues to affect. Injecting too much into a small joint can actually damage tendons or cartilage. Doctors use ultrasound guidance more often now-it boosts accuracy from 70% to 95%. That means fewer missed shots and less risk of hitting a tendon by accident.
Common targets include osteoarthritis flares, rheumatoid arthritis, gout, bursitis, and tendinitis. For example, if you’ve been sidelined by tennis elbow, a cortisone shot into the elbow tendon can get you back to playing in days. But if your pain comes from worn-out cartilage (advanced osteoarthritis), the shot won’t fix the damage-it just silences the inflammation for a while.
How Long Does the Relief Last?
This is where expectations get messy. Many people assume a cortisone shot is a long-term fix. It’s not.
According to NIH meta-analyses, most patients feel better for 2 to 4 weeks. A few lucky ones get relief for 8-12 weeks. But after six weeks, the difference between a steroid shot and a placebo (like saline) disappears. At 24 weeks? No benefit at all.
One 2023 study tracked patients with lateral epicondylitis (tennis elbow). Those who got corticosteroid injections had better pain scores at one month than those who got PRP or saline. But by three months? No difference. The steroid group even had more pain recurrence.
And here’s something most patients don’t know: the first shot often works best. A Reddit thread with over 140 comments from people with chronic joint pain showed a clear pattern. The first injection gave 8 weeks of relief. The second, 6 weeks. The third? Only 3 weeks-and a 3-day flare afterward. That’s not rare. About 28% of users in online reviews report diminishing returns with repeated injections.
When It Works Best (and When It Doesn’t)
Corticosteroid injections shine in three situations:
- Acute inflammatory flares: A sudden gout attack, a flare of rheumatoid arthritis, or a swollen bursa from overuse.
- Diagnostic tool: If your shoulder hurts and you’re not sure if it’s the rotator cuff or the joint itself, a shot that brings immediate relief confirms the joint is the source.
- Temporary bridge: You need pain relief to start physical therapy. The shot gets you through the first few weeks of rehab.
But they’re not recommended for:
- Advanced osteoarthritis: The American College of Rheumatology says no. If your X-ray shows bone grinding on bone, steroids won’t rebuild cartilage. They might even speed up the damage.
- Chronic pain without inflammation: If your pain is from nerve compression or muscle tightness, steroids won’t help.
- Within 3 months of joint replacement surgery: Studies show patients who got a cortisone shot before knee or hip replacement had over 2 times higher risk of post-surgery infection.
Risks and Side Effects You Can’t Ignore
Yes, they work. But they’re not harmless.
Common side effects (affecting up to 8% of people):
- Post-injection flare: Pain, swelling, warmth for 1-3 days after the shot. It’s caused by crystals from the steroid irritating the joint. Ice and ibuprofen usually fix it.
- Temporary blood sugar spike: Diabetics need to check glucose levels for 72 hours after the shot. A 20-40% rise isn’t unusual.
- Skin thinning or lightening: Especially in the shoulder or ankle, where the skin is thin. White patches can last months.
Less common but serious risks:
- Tendon rupture: Especially in the Achilles or rotator cuff. Risk goes up with repeated shots. That’s why most doctors cap injections at 3-4 per joint per year.
- Cartilage damage: Animal and human studies show repeated injections can accelerate joint degeneration. One study found patients with knee injections had 3.2 times higher odds of radiographic osteoarthritis progression.
- Infection: Rare (less than 1 in 1,000), but dangerous. Always report redness, fever, or worsening pain after 48 hours.
Cost, Alternatives, and What’s New
Without insurance, a cortisone shot costs $100-$300. Compare that to PRP ($500-$1,500) or viscosupplementation ($500-$1,000). Steroids win on price and speed.
But new options are emerging. In 2023, the FDA approved Zilretta, an extended-release form of triamcinolone. It’s designed to last 12 weeks instead of 4. In trials, 45% of patients had significant relief at 12 weeks-compared to 24% with standard steroids. It’s pricier, around $1,200, but may reduce the need for repeat shots.
Researchers are also testing combinations: corticosteroid + PRP. The idea? Get the quick relief from the steroid, then let PRP help repair tissue. Twenty-seven clinical trials are underway right now.
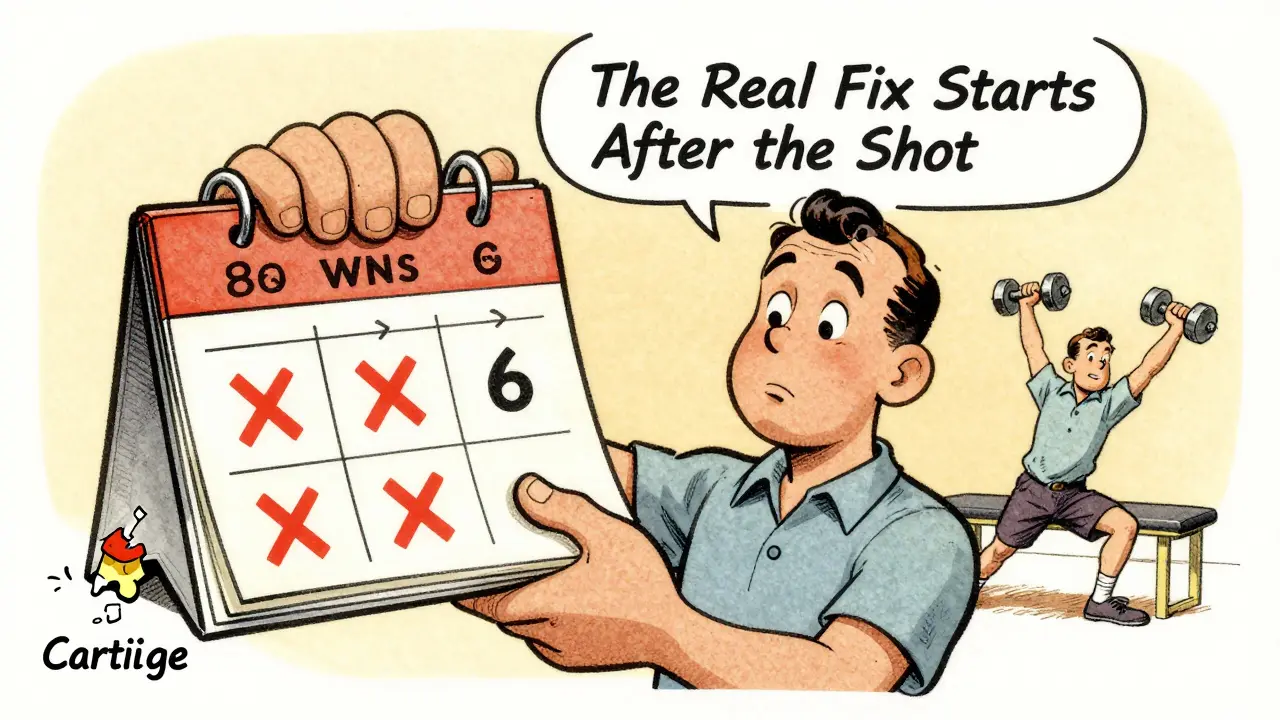
What You Should Do After the Shot
Don’t go back to lifting weights or running the next day. Your joint is still healing. Here’s what experts recommend:
- Rest for 48 hours: Avoid heavy lifting, running, or high-impact activity.
- Use ice: If you feel a flare, apply ice for 15 minutes every few hours.
- Monitor blood sugar: If you’re diabetic, check glucose levels daily for 3 days.
- Start physical therapy: Use the pain-free window to strengthen muscles around the joint. That’s how you prevent the next flare.
- Track your results: Write down when the pain came back and how long it lasted. That helps your doctor decide if another shot is safe.
Many people think cortisone is a cure. It’s not. It’s a pause button. The real work-strengthening muscles, improving movement, managing weight-happens after the shot wears off. Without that, you’re just delaying the problem.
Final Thought: A Tool, Not a Fix
Corticosteroid injections are one of the most effective tools we have for calming down sudden joint inflammation. They’re fast, affordable, and backed by decades of use. But they don’t fix broken cartilage, worn tendons, or degenerated joints. They just turn down the volume on pain.
Use them wisely. Limit them to 3-4 times a year per joint. Never use them as a crutch to keep doing the same thing that hurt you in the first place. And if you’ve had three shots and the relief keeps getting shorter? It’s time to rethink your approach-whether that’s physical therapy, weight loss, bracing, or even surgery.
The goal isn’t to avoid shots forever. It’s to use them when they matter most-and then move on to what actually heals you.
How long does a cortisone shot last in a joint?
Most people get relief for 2 to 4 weeks. Some may feel better for up to 12 weeks, especially with newer extended-release versions like Zilretta. But after 6 weeks, the effect usually fades to the same level as a placebo. Repeated injections often provide shorter relief over time.
Can cortisone shots make joint pain worse?
Yes, in a few ways. Some people get a post-injection flare-pain and swelling for 1-3 days as the crystals irritate the joint. Repeated shots can weaken tendons or accelerate cartilage breakdown, especially in advanced osteoarthritis. In rare cases, they increase infection risk after joint replacement surgery.
Are cortisone injections safe for diabetics?
They can raise blood sugar levels for up to 72 hours after the injection. Diabetics should monitor glucose more frequently during that time and adjust insulin or medication as needed. It’s not dangerous if managed properly, but it requires extra attention.
How many cortisone shots can you get in a year?
Most guidelines recommend no more than 3 to 4 injections per joint per year. More than that increases the risk of tendon rupture, cartilage damage, and infection. The American College of Rheumatology advises against repeated use in joints with advanced degeneration.
Do cortisone shots help with arthritis?
They help with the inflammation and pain from arthritis, especially in flares of rheumatoid arthritis or gout. But they don’t slow down or reverse joint damage from osteoarthritis. In fact, repeated injections may speed up cartilage loss in worn-out joints. They’re a symptom treatment-not a disease-modifying therapy.
What’s the difference between cortisone and PRP injections?
Cortisone reduces inflammation quickly but doesn’t heal tissue. PRP (platelet-rich plasma) uses your own blood platelets to stimulate healing and may offer longer-term benefits. PRP works better for chronic tendon injuries and early osteoarthritis, but it takes weeks to show results and costs more. Cortisone wins for fast relief; PRP wins for long-term repair.
Next steps: If you’re considering a cortisone shot, ask your doctor: "Is this for inflammation, or for structural damage?" If it’s the latter, explore physical therapy, braces, or lifestyle changes first. If it’s the former, make sure you have a plan for what comes after the shot wears off.






Siobhan K.
Corticosteroid injections are basically the medical equivalent of slapping a bandage on a broken leg and calling it a day. You get temporary relief, but the underlying damage keeps creeping in. I’ve had three knee shots in two years - each one shorter than the last. Now I’m doing PT and losing weight. No more needles. Just slow, boring, real healing.
Doctors love these shots because they’re quick and billable. Patients love them because they feel better immediately. Nobody talks about the long-term cost - until your cartilage turns to dust and you’re on the transplant list.
It’s not magic. It’s a delay tactic dressed up as a solution.
Brian Furnell
From a biomechanical standpoint, the anti-inflammatory cascade triggered by corticosteroids - specifically via NF-kB pathway inhibition - is well-documented; however, the downregulation of chondrocyte metabolism and collagen synthesis is a critical, underappreciated consequence. The 2023 meta-analysis by the Journal of Orthopaedic Research demonstrated a 3.2-fold increase in radiographic joint space narrowing in patients receiving >3 injections annually.
Furthermore, the post-injection flare phenomenon is not merely ‘crystal-induced irritation’ - it’s a localized sterile inflammatory response mediated by NLRP3 inflammasome activation. This is why NSAIDs are contraindicated in the first 24 hours - they mask the signal without mitigating the damage.
PRP, while cost-prohibitive, activates TGF-β and IGF-1 pathways, promoting extracellular matrix remodeling. The real question isn’t ‘which is better?’ - it’s ‘when do we stop treating symptoms and start repairing tissue?’
Orlando Marquez Jr
The clinical utility of corticosteroid injections in the management of acute inflammatory arthropathies remains well-established within the current standard of care. However, the growing body of longitudinal data suggests a need for more stringent patient selection criteria, particularly in the context of degenerative joint disease.
As evidenced by the American College of Rheumatology guidelines, the threshold for intervention should be predicated upon objective inflammatory markers, not merely subjective pain reports. The potential for accelerated cartilage degeneration, particularly with repeat administration, necessitates a multidisciplinary approach integrating physical rehabilitation and lifestyle modification.
It is imperative that clinicians communicate not only the benefits, but the limitations and potential iatrogenic consequences of this intervention, in order to foster informed decision-making and prevent therapeutic nihilism.
Cara C
I had a cortisone shot for my shoulder last year and it gave me exactly three weeks of pain-free sleep. That was the first time I’d slept through the night in over a year. I didn’t go back to lifting weights - I started stretching, did PT three times a week, and changed my posture at my desk. Now, six months later, I still don’t need another shot.
It’s not that the shot was the cure. It was the push I needed to finally do the work. If you’re waiting for a needle to fix your life, you’re going to be disappointed. But if you use the quiet window it gives you to change how you move - that’s when real healing starts.
Michael Ochieng
Man, I’ve been through this whole cycle. First shot: 8 weeks of bliss. Second: 5 weeks, then a flare. Third: 2 days of relief and a week of agony. I was ready to give up until my PT told me, ‘You’re not broken - you’re overused.’
I stopped playing basketball every weekend. Started swimming. Did daily hip mobility drills. Lost 20 pounds. Now I can walk my dog for miles without thinking about my knee.
Cortisone isn’t evil. It’s just not the hero we want it to be. The real hero is consistency. And patience. And not being an idiot who keeps doing the thing that hurts you.
Dan Adkins
Let me be clear: The pharmaceutical-industrial complex has weaponized corticosteroid injections as a profit engine disguised as medical care. The FDA approval of Zilretta was not a breakthrough - it was a monetization strategy. The same corporations that market these injections also control the clinical trials, the continuing education for physicians, and the insurance reimbursement codes.
Meanwhile, physical therapy is underfunded, under-reimbursed, and under-promoted. Why? Because it doesn’t generate $1,200 per visit. The system is designed to keep you dependent, not healed.
And don’t get me started on the suppression of alternative modalities like acupuncture and low-dose naltrexone - all proven to reduce inflammation without the collateral damage.
This is not medicine. It’s corporate healthcare.
Adrian Thompson
They’re lying to you. Every single one of them. Cortisone shots? They’re not for pain - they’re for control. The government and Big Pharma want you to believe you need these injections so you’ll keep going to the clinic, keep getting prescriptions, keep paying. Meanwhile, the real cure - diet, sunlight, vitamin D, and avoiding processed carbs - is buried under layers of jargon and ‘evidence-based guidelines.’
My cousin got three shots in his hip. Now he’s on insulin, has high blood pressure, and his knee is collapsing. Coincidence? I think not.
They don’t want you to heal. They want you to be a patient forever.
Southern NH Pagan Pride
soo... i read this whole thing and im just like... why do they even give these shots if they make things worse? like, if the science says they accelerate cartilage loss, why are doctors still doing it? is it because they dont care? or because theyre paid to? i mean, i know its supposed to be for inflammation but... if its just masking the problem, isnt that kinda like putting duct tape on a leaking pipe?
also, anyone else notice that every single study that says it works was funded by a drug company? just saying.
John Hay
I’ve had three cortisone shots in my ankle over five years. Each one worked less. The last one gave me 48 hours. I didn’t go back. I started walking barefoot on grass every morning, did calf stretches, and got custom orthotics. No more pain.
Doctors don’t teach you this stuff. They teach you the shot. But healing isn’t in a syringe. It’s in movement. In patience. In listening to your body when it says, ‘Stop.’
Use the shot if you need it. But don’t let it become your crutch. The real work starts after the numbness fades.