Over 20 million Americans suffer from sleep apnea, and CPAP is the most common treatment. But what if CPAP isn't right for you? This article breaks down the key differences between CPAP and BiPAP machines, when each is recommended, and what to expect in terms of comfort, cost, and effectiveness.
What Are CPAP and BiPAP?
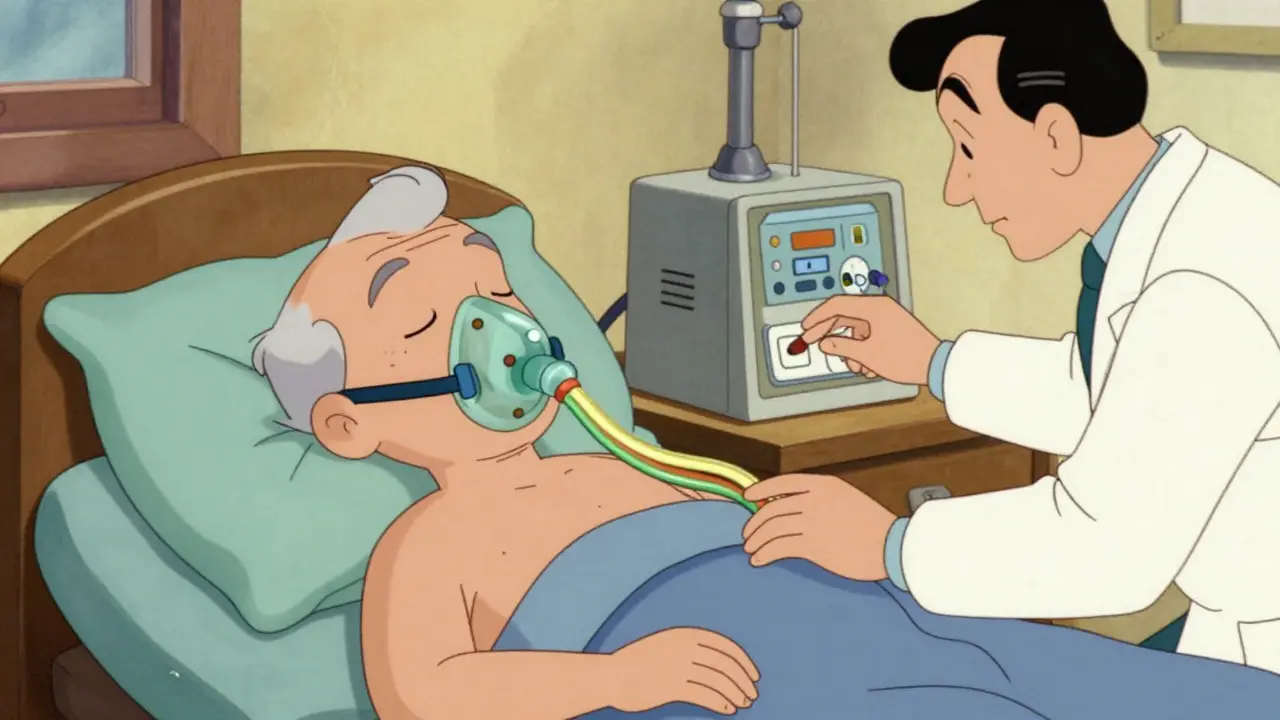
CPAP (Continuous Positive Airway Pressure) is a device that delivers a steady stream of air pressure through a mask to keep your airway open during sleep. First developed in 1981 by Dr. Colin Sullivan at Royal Prince Alfred Hospital in Sydney, it's designed primarily for obstructive sleep apnea (OSA). CPAP maintains a single constant pressure throughout the breathing cycle, typically between 4 and 20 cm H2O.
BiPAP (Bilevel Positive Airway Pressure) builds on CPAP technology but provides two distinct pressure levels. It uses a higher pressure during inhalation (IPAP) and a lower pressure during exhalation (EPAP), making it easier to breathe out. Developed in the late 1980s, BiPAP is used for more complex breathing disorders.
CPAP vs BiPAP: Key Differences
| Feature | CPAP | BiPAP |
|---|---|---|
| Pressure Settings | Single constant pressure | Two levels (IPAP and EPAP) |
| Typical Pressure Range | 4-20 cm H2O | IPAP: 8-30 cm H2O; EPAP: 4-25 cm H2O |
| Best For | Obstructive sleep apnea (OSA) | OSA with high pressure needs, COPD, central sleep apnea |
| Exhalation Comfort | Harder to breathe out | Softer exhalation due to lower EPAP |
| Cost | $500-$1,200 | $800-$1,800 |
| Insurance Coverage | Usually covered | Requires documented CPAP failure |
When CPAP Is the Best Choice
CPAP is the first-line treatment for obstructive sleep apnea in 85-90% of cases, according to the 2023 International Classification of Sleep Disorders. It's ideal for people with simple OSA who don't have other lung conditions. For example, a 45-year-old with a BMI of 30 and no other health issues would likely benefit from CPAP. The machine's simplicity makes it easier to use and maintain.
Many users find CPAP comfortable once they adjust. A 2023 American Sleep Association poll showed 71% of CPAP users rated "ease of use" as excellent. However, some struggle with the constant pressure during exhalation. If your sleep study shows moderate OSA (AHI 15-30) and you're otherwise healthy, CPAP is usually the go-to option.

When BiPAP Is Recommended
BiPAP shines in specific clinical scenarios. For instance, if you have COPD with hypercapnia (high CO2 levels), BiPAP's dual pressures reduce breathing effort. The American Thoracic Society guidelines strongly recommend BiPAP for COPD-OSA overlap syndrome. Similarly, for central sleep apnea or obesity hypoventilation syndrome, BiPAP's backup breath feature can be life-saving.
Patients needing high pressures (over 15 cm H2O) often find BiPAP more tolerable. A 2022 Journal of Clinical Sleep Medicine study found BiPAP reduces respiratory effort by 30-40% compared to CPAP at equivalent pressures. For example, a 60-year-old with severe OSA and COPD might struggle with CPAP but thrive on BiPAP set to 14/8 (IPAP/EPAP).
Cost and Insurance Considerations
CPAP machines typically cost $500-$1,200, while BiPAP ranges from $800-$1,800. Insurance coverage differs significantly. Medicare covers 80% of CPAP costs but requires documented CPAP failure before approving BiPAP. This means you must show you can't use CPAP for at least 4 hours a night over 30 days. A 2022 CMS utilization report found 65% of CPAP users meet the usage threshold versus 60% for BiPAP users.
For those without insurance, out-of-pocket costs can be steep. However, BiPAP's higher price often reflects its complexity. A ResMed AirSense 10 CPAP retails for $899, while a Philips DreamStation BiPAP Auto sells for $1,499 as of mid-2023. Always check with your provider-some insurers cover BiPAP for specific diagnoses without requiring CPAP failure.
Real-World User Experiences
User feedback reveals clear patterns. On CPAP.com's 2023 survey of 12,450 users, 78% reported satisfaction with CPAP, and 62% used therapy ≥6 hours/night. BiPAP users showed 72% satisfaction but higher usage rates (68% ≥6 hours/night) among those with specific indications. Reddit's r/CPAP community has threads where users describe BiPAP as "life-changing" for those who couldn't tolerate CPAP pressures above 12 cm H2O.
However, BiPAP's complexity can be a hurdle. A Sleep Review Magazine survey found 34% of BiPAP users struggled with mode settings versus 18% of CPAP users. Common complaints include "machine cycling issues" where the device doesn't sync with breathing patterns. CPAP's simplicity is a major plus-71% of users rate ease of use as excellent compared to 58% for BiPAP.
Expert Insights and Guidelines
Medical professionals emphasize using the right tool for the job. Dr. David White, former president of the American Academy of Sleep Medicine, stated in a 2022 Medscape interview: "BiPAP should be reserved for specific indications rather than used as first-line therapy for simple OSA." A 2021 Cochrane review of 1,872 participants found no significant advantage over CPAP for standard OSA treatment.
But for complex cases, BiPAP is indispensable. The American College of Chest Physicians recommends BiPAP for COPD with hypercapnia (Grade 2B) and central sleep apnea. Dr. Indra Narang, Director of Sleep Medicine at Toronto's Hospital for Sick Children, notes BiPAP's backup rate feature is critical for central apnea but unnecessary for obstructive apnea. This underscores that device choice must be diagnosis-dependent.
Frequently Asked Questions
What's the main difference between CPAP and BiPAP?
CPAP delivers a single constant pressure during both inhalation and exhalation, while BiPAP provides two different pressures: a higher pressure when inhaling (IPAP) and a lower pressure when exhaling (EPAP). This makes breathing out easier with BiPAP, which is especially helpful for people with lung conditions or high pressure needs.
Is BiPAP better than CPAP for sleep apnea?
For most cases of obstructive sleep apnea (OSA), CPAP is the preferred first-line treatment. BiPAP is typically reserved for specific situations like COPD with hypercapnia, central sleep apnea, obesity hypoventilation syndrome, or when patients can't tolerate CPAP pressures above 15 cm H2O. A 2021 Cochrane review found BiPAP offers no significant advantage over CPAP for standard OSA treatment.
Can I switch from CPAP to BiPAP if I'm not comfortable?
Yes, but it requires a new sleep study to confirm the need. Most insurance providers, including Medicare, require documented CPAP failure before covering BiPAP. This means showing you can't use CPAP for at least 4 hours a night over 30 days. Your sleep specialist will adjust settings based on your new study results.
How long does it take to adjust to a BiPAP machine?
Adjustment time varies, but BiPAP typically requires 3-6 weeks due to more complex settings. ResMed's 2023 data shows CPAP users usually adapt in 2-4 weeks. Working with a respiratory therapist to fine-tune pressure settings and mask fit can speed up this process significantly.
Do I need a prescription for BiPAP?
Yes, both CPAP and BiPAP are medical devices requiring a prescription. A sleep study (polysomnography) must determine the appropriate pressure settings. Without a doctor's recommendation, you can't legally obtain or use these machines in the U.S.







Lakisha Sarbah
I've been using CPAP for 3 years now. At first it was hard to get used to but now its so much better. The mask fits great and I sleep better than ever.
Ariel Edmisten
CPAP works for most OSA cases. BiPAP for complex issues.
Niel Amstrong Stein
I've been using BiPAP for about a year now. 😊 At first I was worried it would be complicated but it's actually pretty simple. The dual pressure really helps with exhaling. I used to struggle with CPAP because it felt like I was fighting the machine to breathe out. Now with BiPAP, it's smooth. The machine is quiet and the mask fits well. 😌 I sleep through the night without waking up. My doctor recommended it after my sleep study showed high pressure needs. The cost is higher but worth it for the comfort. I've noticed better energy during the day. 🌞 The insurance covered it after they saw CPAP wasn't working. It's made a huge difference in my quality of life. I'd recommend BiPAP to anyone with similar issues. Definitely worth trying if CPAP isn't working for you. The only downside is the higher price but it's worth it. 😅
Paula Sa
After using CPAP for a year, I switched to BiPAP. The difference in comfort was noticeable. It's good to know the options exist.
Mary Carroll Allen
I HATE CPAP! It was so hard to breath out against the constant pressure. Switched to BiPAP and now I sleep like a baby. 😍
Joey Gianvincenzi
It is my firm belief that CPAP should remain the first-line treatment for obstructive sleep apnea. BiPAP is frequently prescribed without adequate justification, leading to unnecessary healthcare costs. Insurance providers should not impose arbitrary barriers to BiPAP access.
Amit Jain
CPAP is the way to go for 90% of cases. BiPAP is overkill. People should just stick with CPAP and get used to it.
Sarah B
BiPAP is useless
Tola Adedipe
I've used both. BiPAP is better for my needs. But CPAP works well for others. It's about what works for you.