Generic drugs have long been the backbone of affordable healthcare. But the next wave isn’t just copying old pills-it’s reimagining them. Generic combinations are changing the game. These aren’t your grandfather’s generics. They’re fixed-dose combos, smart inhalers, extended-release capsules, and drug-device systems designed to work better, be easier to use, and improve patient outcomes-all at a fraction of the cost of brand-name drugs.
What Exactly Are Generic Combinations?
Traditional generics copy a single active ingredient after a patent expires. Generic combinations do something more. They take two or more drugs, or a drug and a device, and pack them into one product that’s smarter than the sum of its parts.
Think of it like upgrading from a basic smartphone to a model with facial recognition, longer battery life, and better camera software-all in the same body. For example, a fixed-dose combination (FDC) might put a blood pressure pill and a cholesterol drug into one tablet. That’s not just convenience-it’s better adherence. Patients who take fewer pills are more likely to stick to their treatment.
Drug-device combos are even more advanced. Imagine an inhaler that tracks when you use it and sends data to your doctor’s app. Or an auto-injector for diabetes that adjusts dose based on glucose levels. These aren’t sci-fi-they’re already on the market. Teva, Viatris, and other generics giants are investing heavily in these.
Why the Surge Now?
The push toward generic combinations isn’t random. It’s a response to three big pressures.
First, traditional generics are a race to the bottom. Once a drug goes generic, prices crash by 80-90% within two years. Margins vanish. Companies can’t survive on pennies per pill.
Second, patent cliffs are coming. Between 2025 and 2030, branded drugs worth over $200 billion in annual sales will lose exclusivity. Trelegy Ellipta, a three-drug inhaler for COPD, made $2.8 billion in 2024. Austedo, a complex CNS drug, hit $1.2 billion. These aren’t small targets-they’re goldmines waiting for smarter generics.
Third, patients and payers want better outcomes. If you can reduce hospital visits, improve compliance, or cut side effects with a smarter combo, you save the system money in the long run. That’s a powerful argument for reimbursement.
Enter super generics. These are complex, value-added versions that command higher prices. While a basic generic might sell for $0.10 a pill, a well-designed combo can hold onto 40-60% of the brand’s price for five years or more. IQVIA found that super generics generate 20-35% margins-far higher than the 5% typical of simple generics.

Regulatory Hurdles Are Real
Getting approval for a generic combination isn’t like filing a simple ANDA. The FDA treats these as combination products, which means extra steps, extra data, and extra time.
For fixed-dose combos, you must prove the combination works better than taking the drugs separately. That means clinical trials. Not just bioequivalence-therapeutic advantage. For drug-device combos, the FDA’s Office of Combination Products decides whether the drug or the device is the primary mode of action. That determines which center reviews it: drugs or devices. The process can take 18-24 months longer than a standard generic.
And it’s expensive. A basic generic costs $1-5 million to develop. A complex combo? $15-50 million. That’s why only big players or well-funded startups are playing this game. Small generics firms can’t afford the risk.
Even then, failure rates are high. According to RAPS, 78% of combo applications get rejected not because the drug doesn’t work-but because the delivery system doesn’t match the reference product closely enough. A 10% difference in dissolution profile? Rejection. A slightly different valve in an inhaler? Rejection. The bar is high.
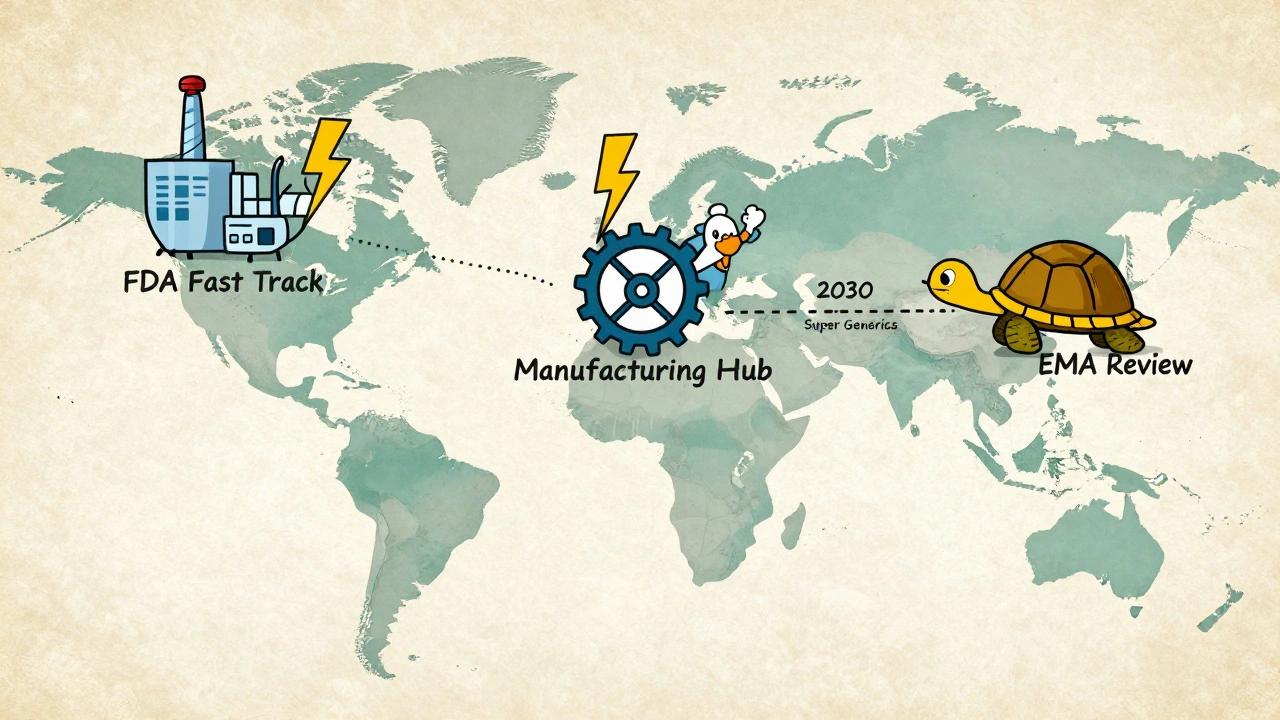
The FDA is trying to help. In October 2025, it launched a pilot program to fast-track reviews for U.S.-manufactured generic combinations. Approval timelines could drop by 3-6 months. That’s a big deal. But the European Medicines Agency (EMA) is playing it safe. Only 12 complex combos got approved in the EU through Q1 2025-compared to 37 in the U.S. That creates a split market. Companies must tailor their submissions by region.
Market Winners and Losers
Not everyone can win in this space. The winners are those who can handle complexity.
Companies like Viatris and Sandoz are doubling down. Viatris merged with Credence in 2025 for $2.3 billion to boost its combo capabilities. Sandoz, now independent from Novartis, is focused entirely on complex generics. Aspen Pharmacare is working on generic semaglutide combos-targeting the $100+ billion GLP-1 market.
Manufacturing is another bottleneck. These products need precision. A 2% error in the ratio of two active ingredients? The product fails. That requires hot-melt extrusion, lipid-based delivery systems, and equipment calibrated to ±2% tolerance. Only a handful of manufacturers globally can do this at scale.
India is becoming the manufacturing hub, producing 35% of the world’s complex generics. But quality control remains uneven. The U.S. still leads in innovation and regulatory clarity. The U.S. market captured 42% of global combo sales in 2025, thanks to better reimbursement and a more flexible FDA.
Therapeutic areas with the most growth? Oncology (11.3% CAGR), respiratory (9.89% CAGR), and CNS disorders (8.7% CAGR). These are areas with high unmet need, expensive branded drugs, and patients who struggle with adherence. Perfect targets for combos.
The Future: More Complexity, More Value
The trend is clear: the future of generics isn’t cheaper pills-it’s smarter medicine.
By 2030, super generics are expected to make up 35-40% of the total generics market value, even though they’ll only be 20-25% of the volume. That’s the power of value-based pricing.
Three big trends will shape the next decade:
- Complexity premium: Products with multiple innovations-like a combo pill with extended release + a sensor-will command 2-3x the price of a standard generic.
- Regional divergence: The U.S. will keep moving faster than Europe and Asia. Companies will need separate development paths for each region.
- Device partnerships: Generic pharma companies are teaming up with device makers. Catalent and Hikma are already working on smart auto-injectors. Expect more of this.
But there’s a warning. Morningstar predicts pricing pressure could erode generic margins by 30% over the next decade. If companies don’t move into higher-value combos, they’ll be squeezed out. The race isn’t just about cost anymore-it’s about clinical impact.
What This Means for Patients and Providers
For patients, this means better options. Fewer pills. Fewer side effects. Better control of chronic diseases. For doctors, it means simpler regimens and improved adherence data-especially with smart devices.
For payers, it’s a gamble. These combos cost more upfront. But if they reduce ER visits, hospitalizations, or nursing home stays, they save money over time. The real question isn’t price-it’s value.
The bottom line? Generic combinations aren’t just a trend. They’re a necessity. The old model of slashing prices to win market share is dead. The new model is innovating to justify higher prices through real therapeutic improvement. The companies that get this right will lead the next generation of affordable medicine. The ones that don’t? They’ll disappear.







Michelle Smyth
The commoditization of pharmaceuticals has reached its dialectical antithesis-now we’re witnessing the re-sublimation of generic therapeutics into Hegelian synthetic unities. The FDA’s regulatory apparatus, still trapped in its Kantian categorical imperative of bioequivalence, fails to grasp that the *phenomenon* of the drug-device combo transcends mere pharmacokinetics-it’s a hermeneutic of adherence. We’re not selling pills; we’re selling ontological stability for the chronically ill.
Patrick Smyth
This is the most important thing I’ve read all year. My mother has COPD and she forgets her inhalers. This new smart inhaler thing? It’s literally saving lives. I cried reading this. We need this everywhere. Please make it cheaper. I can’t believe we’re still fighting over pennies when people are dying.
Declan Flynn Fitness
Big picture: this is the future. 🙌 The days of just copying a single molecule are over. Companies that stick to that are gonna vanish like Blockbuster. The smart ones are building ecosystems-pills + sensors + apps + data. It’s not just pharma anymore, it’s digital health. And yeah, the FDA is slow, but the pilot program? That’s a sign. India’s scaling manufacturing, but the US still leads in getting the combo right. If you’re in this space, you better be building complexity, not cutting corners.
Souvik Datta
Let me tell you something-this is not just about medicine. This is about dignity. When a patient has to juggle five pills a day, they don’t just forget-they feel broken. A single combo tablet? It’s not convenience. It’s respect. And the device integrations? That’s not tech for tech’s sake-it’s compassion engineered. India is ready to build this. We have the talent, the scale, the grit. But we need global partnerships, not just export contracts. Let’s make affordable dignity global.
Priyam Tomar
Everyone’s acting like this is revolutionary. Newsflash: fixed-dose combos have existed since the 90s. The real story is that Big Pharma is using ‘super generics’ as a loophole to extend monopolies under the guise of innovation. The FDA’s ‘therapeutic advantage’ standard? A joke. Half of these ‘improvements’ are statistically meaningless. And don’t get me started on the $50M development costs-that’s just a barrier to entry for smaller players so the oligopolies can keep their margins. This isn’t progress. It’s rent-seeking with a stethoscope.
Walker Alvey
Wow. So we spent 20 years screaming about drug prices… and now the solution is to charge more for pills with sensors? Congrats. You turned healthcare into Apple. Now the poor get the basic generic. The rich get the one that texts their doctor. Brilliant. 🤡
Linda Migdal
Let’s be clear: if this innovation happens in the U.S., it’s world-class. If it happens in India, it’s a quality risk. The FDA’s standards aren’t red tape-they’re the reason American patients live longer. Europe’s 12 approvals? Pathetic. We’re not just making pills-we’re defending American leadership in health tech. No compromises. No shortcuts. This is national security.
Tommy Walton
Imagine if your insulin pen could tell your doctor you skipped a dose… then send you a meme to get your ass back on track 😎💊 That’s the future. Not just meds. Mood. Motivation. Magic. The U.S. is leading because we don’t fear innovation-we celebrate it. Europe’s still stuck in 2010. India’s building it. But only America’s selling the dream.
Declan Flynn Fitness
@5317 you’re not wrong about the cost barriers-but dismissing therapeutic advantage as meaningless ignores real data. A 2023 JAMA study showed FDCs for hypertension reduced missed doses by 41%. That’s not marketing-that’s hospitalization avoidance. And yes, the FDA is tough, but that’s why only 1 in 5 combos make it. The ones that do? They’re better. Not just pricier. The problem isn’t innovation-it’s access. We need policy to incentivize rollout, not just R&D.