If you’re dealing with frequent heartburn, a sour taste in your mouth, or that burning feeling that climbs up your chest after eating, you’re not alone. About 20% of adults in the U.S. have gastroesophageal reflux disease, or GERD. It’s not just occasional discomfort-it’s a chronic condition that can damage your esophagus over time if left unmanaged. The good news? Most people can get control of it without surgery, using a mix of simple lifestyle tweaks, smart eating habits, and the right medications.
Start with What You Eat and When
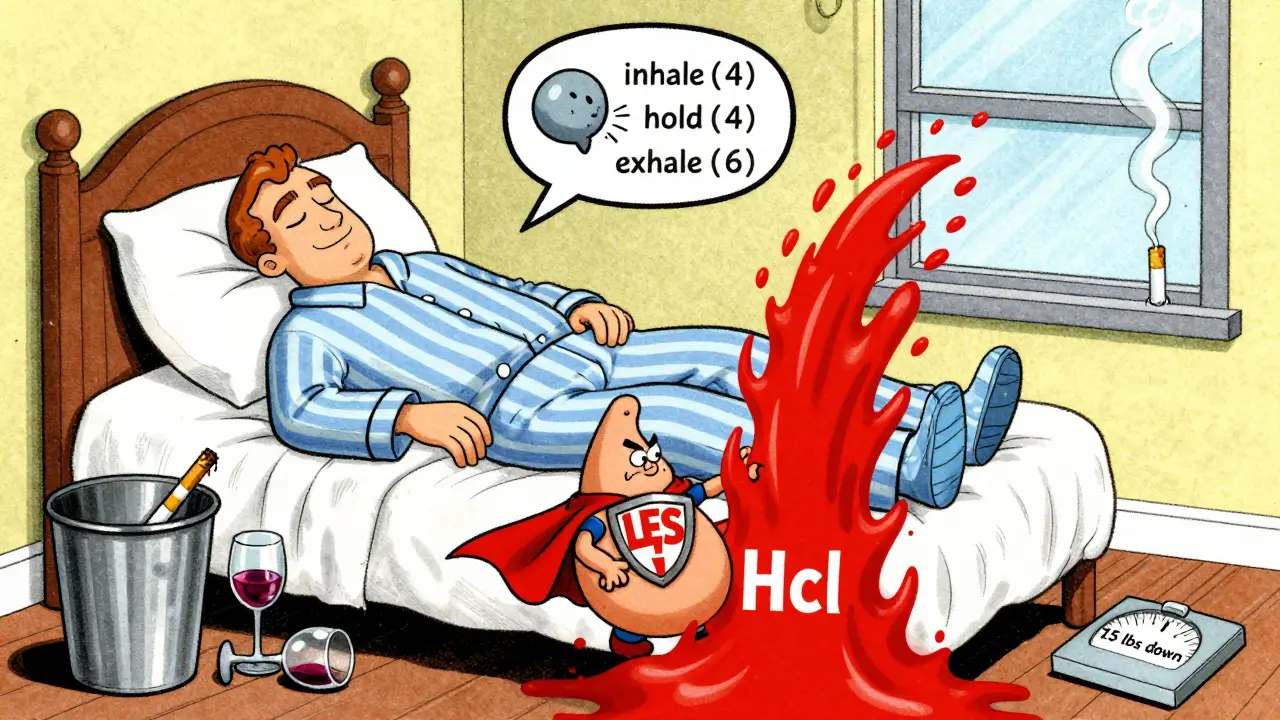
Food doesn’t cause GERD, but it can turn a quiet flare-up into a full-blown episode. Certain foods relax the lower esophageal sphincter (LES), the muscle that keeps stomach acid where it belongs. Others make your stomach churn out more acid or irritate the lining of your esophagus.Common triggers include:
- Caffeinated drinks like coffee, tea, and energy drinks-these boost acid production by 23% within 30 minutes
- Fatty meals, especially those over 30 grams of fat, which slow digestion and increase reflux by 40%
- Chocolate, thanks to methylxanthine, which loosens the LES by 10-15%
- Peppermint and spearmint, even in tea or gum, which can relax the LES within minutes
- Citrus fruits and juices (oranges, lemons, grapefruit) with pH levels as low as 2.0, directly irritating the esophagus
- Tomato-based sauces and soups, which increase stomach acidity
- Carbonated drinks that swell your stomach, pushing acid upward
- Spicy foods, which don’t cause acid but make your esophagus more sensitive to it
It’s not about cutting out everything at once. Start by keeping a food diary for two weeks. Write down what you eat, when you eat it, and how you feel an hour later. Most people find 2-3 triggers that are their personal culprits. One Reddit user, u/HeartburnWarrior, eliminated high-fat meals and started elevating their bed-no meds needed. Their symptoms vanished.
Timing matters too. Lying down within an hour after eating increases reflux episodes by 50%. Wait at least three hours after your last meal before going to bed. That means if you eat dinner at 7 p.m., don’t climb under the covers until 10 p.m. Even better-raise the head of your bed by six inches. Gravity helps keep acid down while you sleep.
Lifestyle Changes That Actually Work
Medication won’t fix GERD if you’re still smoking, overweight, or wearing tight belts. Lifestyle changes aren’t optional-they’re the foundation of long-term relief.Smoking cuts LES pressure by 30-40% within 20 minutes of a cigarette. Quitting doesn’t just help your lungs-it helps your stomach stay put. Alcohol does the same thing. Limit yourself to under two standard drinks a day. One glass of wine might be fine. Two? That’s when reflux kicks in.
Weight loss is one of the most powerful tools. Losing just 10% of your body weight can cut GERD symptoms by 40%. That’s not a vague recommendation-it’s backed by clinical data. You don’t need to lose 50 pounds. Even a 15- to 20-pound drop can make a noticeable difference.
Stress doesn’t cause GERD, but it makes symptoms worse. Simple breathing techniques-like inhaling slowly through your nose for four counts, holding for four, then exhaling through your mouth for six-can reduce symptoms by 35% when done after meals. It sounds too simple, but it works. The diaphragm helps keep the LES closed. When you’re stressed, you breathe shallowly and weaken that natural barrier.
Medications: From Antacids to P-CABs
If diet and lifestyle changes aren’t enough, medications step in. They’re not a cure, but they’re highly effective at managing symptoms and healing damage.Start with over-the-counter antacids like Tums (calcium carbonate). They neutralize acid fast-within minutes-but only last 30 to 60 minutes. Great for occasional heartburn, not for daily use.
Next up are H2 blockers like famotidine (Pepcid). These reduce acid production by 60-70%. They kick in within an hour and last 10-12 hours. Good for nighttime symptoms or if you know you’re going to eat something spicy.
For moderate to severe GERD, proton pump inhibitors (PPIs) are the gold standard. Drugs like omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix) cut acid production by 90-98%. They’re taken once daily, 30-60 minutes before your first meal. Why before? Because they target the acid-producing pumps in your stomach while they’re waking up. Taking them after eating? You’re missing the window. A 2023 Mayo Clinic study found 40% of people don’t get full relief because they take PPIs at the wrong time.
PPIs heal erosive esophagitis in 80-90% of patients within eight weeks. But long-term use-over a year-comes with risks. The FDA warns of higher chances of pneumonia, C. diff infection, and chronic kidney disease. Some people also develop low magnesium or vitamin B12 levels. That’s why doctors now recommend the lowest effective dose for the shortest time possible.
Then there’s the new kid on the block: potassium-competitive acid blockers (P-CABs). Vonoprazan (Voquezna), approved by the FDA in December 2023, works faster and lasts longer than PPIs. In studies, 95% of patients maintained stomach pH above 4 for a full 24 hours-compared to only 65% with PPIs. That’s huge for people who wake up at 3 a.m. with heartburn (a problem called nocturnal acid breakthrough). As of mid-2024, over 120,000 prescriptions were filled in just one quarter.
Surgery: When Medication Isn’t Enough
About 10-15% of people with GERD eventually need surgery. That’s not because they failed-they just need a more permanent fix.The most common procedure is laparoscopic Nissen fundoplication. Surgeons wrap the top of your stomach around the lower esophagus to reinforce the LES. Success rates are 90-95% at five years. But about 15-20% of patients develop gas-bloat syndrome-feeling full quickly or unable to burp. Around 5-10% have trouble swallowing solid food afterward.
The LINX device is a newer option. It’s a tiny bracelet of magnetic titanium beads implanted around the LES. It lets food pass through but snaps shut to block acid. In five-year studies, 85% of patients stayed off daily PPIs. Only 2-3% needed another surgery. But it’s not for everyone. You can’t get an MRI after LINX, and it’s not recommended if you’ve had prior stomach surgery.
Transoral incisionless fundoplication (TIF) is another minimally invasive option. Done through the mouth with an endoscope, it rebuilds the valve without cuts. Success rates are 70-75% at three years. But there are only 127 certified providers in the U.S. as of early 2025. It’s not widely available yet.

What Works for One Person Might Not Work for Another
There’s no one-size-fits-all plan. Dr. Stuart Spechler from UT Southwestern says 30-40% of GERD patients have non-erosive reflux-meaning their esophagus looks normal, but they still feel pain. For them, the issue isn’t just acid. It’s heightened sensitivity, nerve problems, or even bile reflux. That’s why personalized treatment matters.Some people heal with diet and elevation alone. Others need PPIs for years. A few find freedom with LINX. What’s right for you depends on your symptoms, your health history, and your goals. If you hate taking pills every day, surgery might be worth exploring. If you’re worried about long-term drug risks, start with lifestyle changes before jumping to medication.
And don’t ignore the emotional side. GERD can mess with sleep, confidence, and even your social life. If you’re avoiding restaurants, skipping dinner with friends, or waking up anxious about heartburn, you’re not just dealing with acid-you’re dealing with a quality-of-life issue. That’s just as important to treat.
What’s Next in GERD Care?
The GERD treatment market is growing fast-projected to hit $9.8 billion by 2028. Why? Obesity rates are climbing, and more people are living longer. The FDA just approved vonoprazan for long-term use in May 2024, expanding its use beyond short-term relief. The American College of Gastroenterology is updating its guidelines for late 2025, with new focus on non-acid reflux and individualized diets.Meanwhile, the LINX device got expanded approval in July 2024 to include patients with BMI up to 40-meaning more people who are overweight can now consider it.
One thing’s clear: the future of GERD care isn’t about choosing between pills or surgery. It’s about matching the right tool to the right person. Whether that’s cutting out chocolate, taking PPIs correctly, trying breathing exercises, or considering LINX-it’s all part of the same goal: living without constant heartburn.







Robin Williams
bro i just started elevating my bed with cinderblocks and holy shit i slept like a baby for the first time in years. no pills, no drama. gravity is real. why did no one tell me this sooner?
Alan Lin
While I appreciate the comprehensive overview of GERD management, I must emphasize the critical importance of adhering to evidence-based clinical guidelines when implementing pharmacological interventions. The temporal dynamics of proton pump inhibitor administration, for instance, are not merely procedural-they are physiologically deterministic. Failure to administer PPIs prior to the diurnal activation of gastric H+/K+ ATPase pumps renders therapeutic efficacy suboptimal, as corroborated by the 2023 Mayo Clinic cohort analysis. Moreover, the longitudinal use of PPIs necessitates vigilant monitoring for micronutrient deficiencies, particularly magnesium and cobalamin, which are increasingly recognized as iatrogenic sequelae.
Gregory Parschauer
Of course, the real issue here is that people refuse to take responsibility. You eat greasy pizza at midnight, then blame your esophagus? Pathetic. I’ve been GERD-free for 12 years because I don’t indulge in childish cravings. No chocolate. No coffee after noon. No lying down until 4 hours after dinner. If you can’t follow basic biological rules, don’t expect medicine to fix your laziness. This isn’t a buffet-it’s your digestive tract.
Anny Kaettano
Just wanted to add that P-CABs like vonoprazan are game-changers for nocturnal breakthrough-especially if you’re on a PPI and still waking up at 3 a.m. with that burning sensation. The 24-hour pH control data is insane. I’ve seen patients go from 5 PPIs a week to one P-CAB and sleep through the night. The only catch? Insurance still fights covering it unless you’ve failed at least two PPIs. So if your doc says ‘try this first,’ push back. It’s not about cost-it’s about quality of life.
Scottie Baker
Y’all are overcomplicating this. I had GERD for 15 years. Took PPIs. Got kidney issues. Quit caffeine. Stopped eating after 7. Raised my bed. Done. No surgery. No magic pills. Just stop being a damn fool and listen to your body. Why is this so hard?
Kimberly Mitchell
Let’s be real-most of these ‘lifestyle changes’ are just bourgeois nonsense. People who have the luxury to wait three hours after dinner, buy expensive bed risers, and stress about methylxanthine content are the same people who think ‘mindfulness’ solves chronic illness. I work two jobs. I eat when I can. My GERD isn’t a personality flaw-it’s a systemic failure of healthcare access. Stop blaming the patient.
Vinaypriy Wane
Thank you for this detailed, well-researched post. I especially appreciate the inclusion of clinical percentages and timelines. I have been managing GERD for over a decade, and the P-CAB data is indeed promising. However, I must caution that the LINX device, while innovative, is contraindicated in patients with prior abdominal surgery or those who may require future MRI scans. Many physicians overlook this, and patients end up in worse situations. Please, always consult a gastroenterologist before proceeding with implants.
Diana Campos Ortiz
okay so i tried the bed elevation thing with pillows and it just made my neck hurt… then i bought a wedge pillow for $25 and now i sleep like a log. no meds. just… gravity. also, i stopped eating spicy food at night. not because it’s ‘bad’-but because my body told me to. listen to your body. it knows.
Jesse Ibarra
Anyone who thinks PPIs are safe for long-term use is either misinformed or complicit in pharmaceutical propaganda. The FDA warnings are buried in fine print, and doctors keep prescribing them like candy. I’ve seen patients develop interstitial nephritis from three years of omeprazole. This isn’t medicine-it’s corporate convenience. And don’t even get me started on the ‘breathing exercises.’ If your esophagus is being eroded by acid, deep breaths won’t fix your anatomy. Fix the source. Not the symptom.
jefferson fernandes
Just wanted to say: if you’re using antacids daily, you’re already in trouble. They’re a Band-Aid on a ruptured artery. H2 blockers? Fine for occasional use. But if you need something every day, you’re past the point of ‘diet tweaks.’ You need a plan. And if your doctor isn’t talking about P-CABs or LINX by now, find a new one. This isn’t 2010 anymore. We have better tools. Use them.
Acacia Hendrix
It’s fascinating how the literature now distinguishes between erosive and non-erosive reflux disease, yet the mainstream discourse still lumps them together as ‘GERD.’ The neurosensory hypersensitivity component in NERD is profoundly under-researched, and the pharmacological interventions targeting visceral afferent pathways-such as low-dose tricyclics or gabapentinoids-are rarely considered in primary care. This post, while thorough, still operates within a reductionist acid-centric paradigm. The future lies in neuromodulation, not just proton suppression.
mike swinchoski
you know what fixes GERD? not eating. just don’t eat. problem solved. also, stop drinking water after meals. it dilutes your stomach acid and makes it worse. science.
Lance Nickie
lol the guy who said ‘no meds needed’ after raising his bed and cutting fat? that’s not a success story-that’s a fluke. I’ve done all that. Still got acid at 2 a.m. PPIs saved my life. Don’t shame people who need meds.