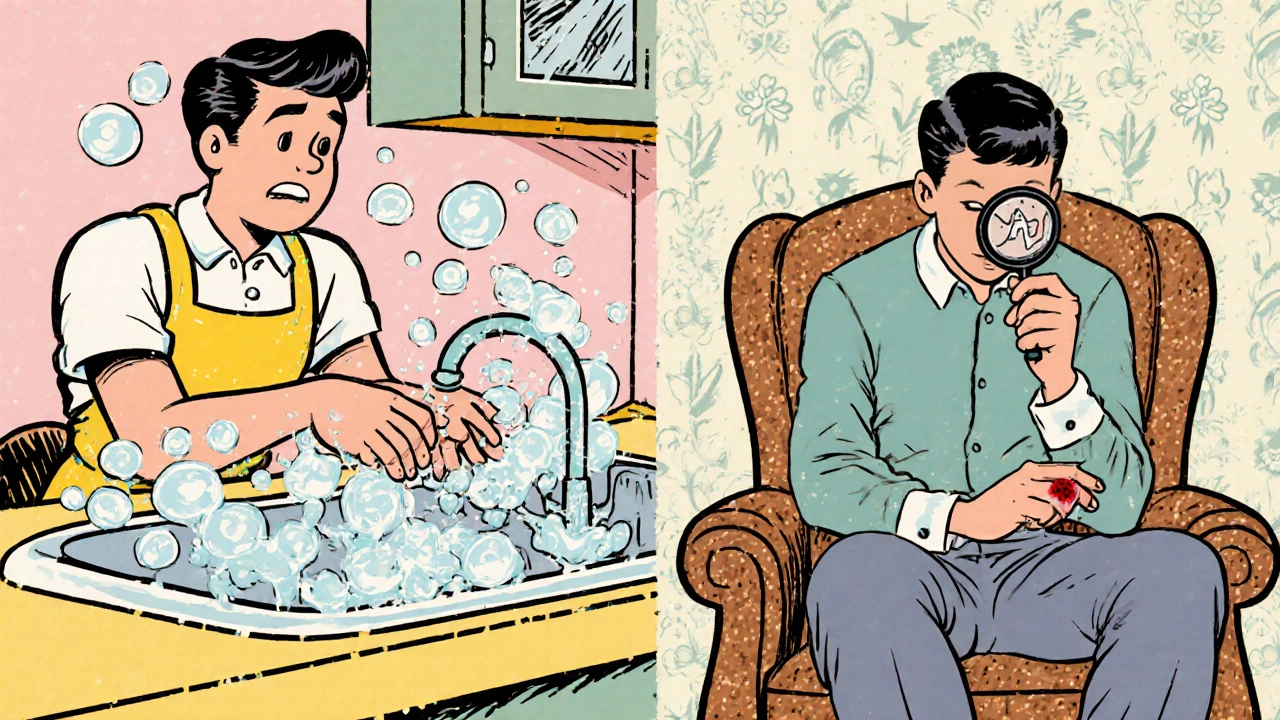
When you hear the term OCD, the image that often pops up is someone washing their hands over and over or arranging objects in a perfect line. But the reality is broader: obsessive‑compulsive disorder can intertwine with other habits that look very different, like compulsive skin‑picking. This article unpacks the link between OCD and Excoriation (Skin‑Picking) Disorder, breaks down why they often appear together, and shows what the latest research says about treatment.
What Is Obsessive‑Compulsive Disorder?
Obsessive‑Compulsive Disorder (OCD) is a mental‑health condition characterized by persistent, intrusive thoughts (obsessions) and repetitive behaviors (compulsions) performed to relieve the anxiety those thoughts generate. The obsessions can be about contamination, symmetry, aggressive impulses, or a host of other themes, while compulsions range from checking doors to mental rituals like counting. OCD affects roughly 2 % of the global population and is listed in the DSM‑5 as an anxiety‑related disorder.
What Is Excoriation (Skin‑Picking) Disorder?
Excoriation (Skin‑Picking) Disorder (also called dermatillomania) involves recurrent picking at skin lesions that leads to tissue damage, distress, and functional impairment. Unlike occasional nail‑biting, skin‑picking is driven by an urge that feels hard to resist, often providing temporary relief or a sense of satisfaction. The DSM‑5 classifies it under body‑focused repetitive behaviors (BFRBs), and prevalence estimates hover around 1‑2 % of adults.
Why Do OCD and Skin‑Picking Often Co‑occur?
Clinical surveys consistently report that up to 30 % of people diagnosed with OCD also meet criteria for excoriation disorder, and vice‑versa. Several mechanisms explain this overlap:
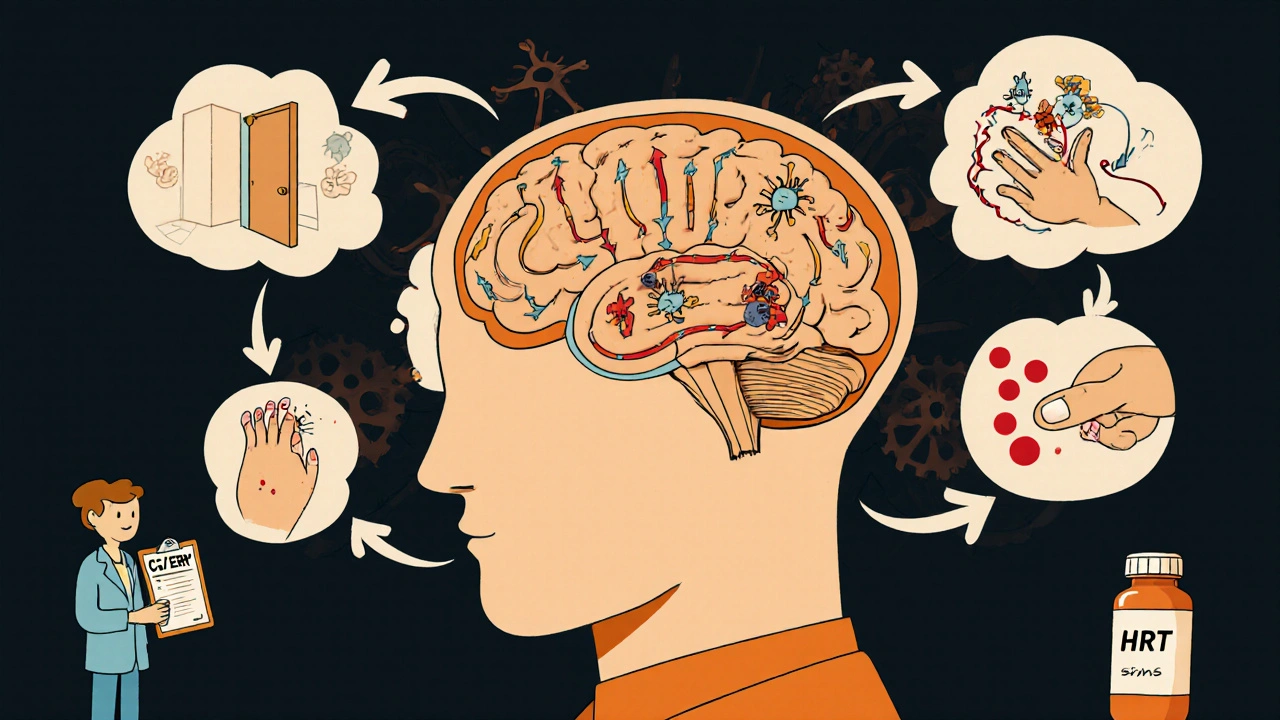
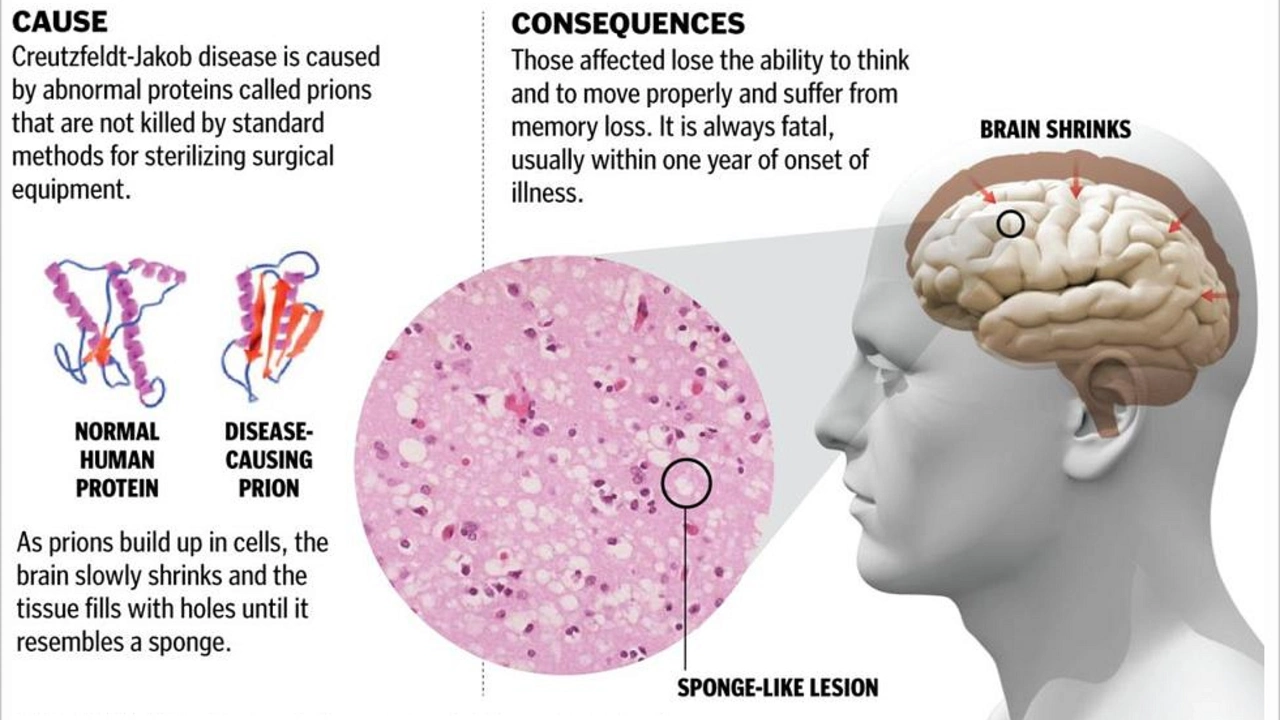
- Shared neurobiology: Functional imaging shows abnormal activity in the cortico‑striato‑thalamo‑cortical (CSTC) circuit for both conditions, suggesting a common “habit‑loop” that drives repetitive actions.
- Genetic factors: Twin studies reveal that genetic liability to OCD also increases the odds of BFRBs, indicating overlapping heritability.
- Emotional regulation: Both disorders can serve as coping strategies for anxiety, stress, or boredom. The urge to pick may arise after a distressing obsession resolves, offering a brief emotional reset.
- Comorbid anxiety and depression: Mood disturbances amplify the urge to perform compulsive behaviors, creating a feedback loop that reinforces both OCD and skin‑picking.
How the DSM‑5 Describes the Relationship
The Diagnostic and Statistical Manual of Mental Disorders (DSM‑5) treats excoriation disorder as a separate entity, but clinicians are encouraged to note any co‑existing OCD symptoms. The manual’s cross‑referencing highlights that BFRBs often appear alongside anxiety disorders, providing a diagnostic clue for practitioners when patients present with skin lesions without a dermatologic cause.
Key Differences Between OCD Rituals and Skin‑Picking
| Feature | OCD | Excoriation Disorder |
|---|---|---|
| Primary Drive | Reduce anxiety from obsessions | Alleviate tension or gain sensory gratification |
| Typical Behaviors | Washing, checking, ordering | Picking at pimples, scabs, healthy skin |
| Awareness | Often recognize behavior as excessive | May deny or rationalize as “just a habit” |
| Physical Damage | Usually minimal, unless self‑harm present | Visible lesions, scarring, infection risk |
| First‑Line Treatment | Cognitive‑behavioral therapy (CBT) with exposure‑response prevention | Habit reversal training (HRT) and CBT variants |
Treatment Overlap: What Works for Both?
Because the brain circuits overlap, many interventions that help OCD also reduce skin‑picking. The most evidence‑based approaches include:
- Cognitive‑behavioral therapy (CBT): Traditional CBT focuses on identifying irrational thoughts and challenging them. When paired with exposure‑response prevention (ERP), patients practice resisting the compulsion while tolerating anxiety.
- Habit reversal training (HRT): A core component of CBT for BFRBs, HRT teaches patients to recognize the urge, substitute a competing response (e.g., clenching fists), and reinforce the new habit.
- Selective serotonin reuptake inhibitors (SSRIs): Medications like fluoxetine and sertraline increase serotonin levels, which can dampen the intensity of both obsessions and urges to pick.
- Mindfulness‑based strategies: Grounding exercises help patients observe urges without acting on them, reducing the automaticity of the behavior.
- Dermatologic adjuncts: Topical emollients, silicone gels, and occlusive bandages create physical barriers that make picking harder, complementing psychological work.
Importantly, treatment should be tailored. A patient whose OCD revolves around contamination may benefit most from ERP, while a skin‑picker whose primary trigger is boredom may see faster gains with HRT plus mindfulness.
Common Pitfalls and How to Avoid Them
Even with evidence‑based options, clinicians and patients can stumble:
- Misdiagnosis as purely dermatologic: Dermatologists sometimes treat the lesions without addressing the underlying compulsive behavior, leading to recurrence.
- Over‑reliance on medication: SSRIs help but rarely eliminate the urge; combining meds with therapy yields the best outcomes.
- Ignoring comorbidities: Depression or ADHD can amplify picking episodes, so screening for these conditions is essential.
- Skipping habit‑trigger assessment: Many patients pick while watching TV or scrolling on phones. Identifying context allows targeted interventions.
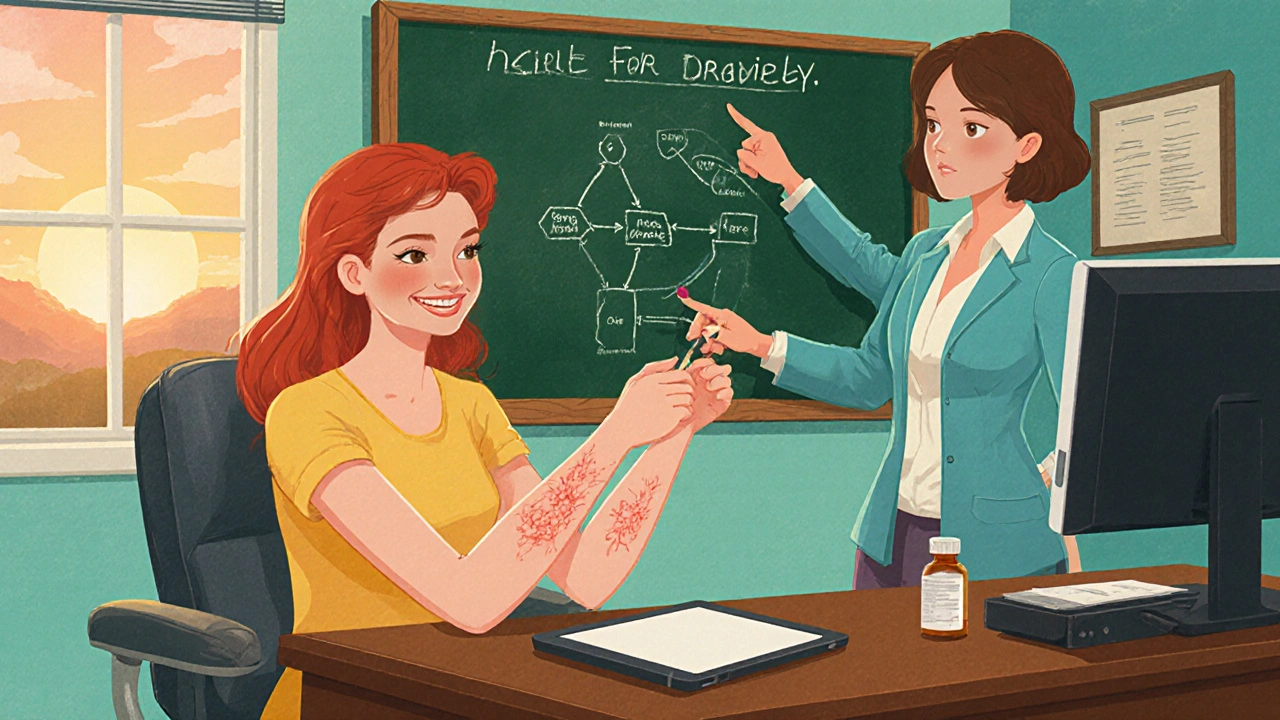
Real‑World Example: Jane’s Journey
Jane, a 28‑year‑old graphic designer, was first diagnosed with OCD at 22 after a series of hand‑washing rituals. Two years later, she started noticing small scabs on her forearms that she couldn’t stop scratching. A dermatologist dismissed them as eczema, but the lesions kept worsening. When a mental‑health therapist took a comprehensive history, she recognized the skin‑picking as excoriation disorder co‑occurring with OCD. Jane began a combined treatment plan: weekly CBT with ERP for contamination fears, daily HRT exercises for picking, and a low‑dose SSRI. Within three months, her hand‑washing reduced from 30 times a day to 8, and the scabs healed completely. Jane’s story illustrates how addressing both disorders together fast‑tracks recovery.
Practical Checklist for Anyone Suspecting a Link
- Track urges: Keep a log of when picking occurs and what thoughts preceded it.
- Seek a dual‑assessment: Ask both a psychiatrist/psychologist and a dermatologist about your symptoms.
- Explore CBT‑ERP: Even if you think your compulsions are only skin‑related, ERP can reduce overall anxiety.
- Consider HRT: Learn a “competing response” like squeezing a stress ball when the urge hits.
- Talk to your doctor about SSRIs: They may lower the intensity of both obsessions and picking urges.
Future Directions in Research
Scientists are probing deeper into why OCD and excoriation disorder co‑exist. Two promising avenues are:
- Neurofeedback training: Real‑time fMRI feedback could teach patients to down‑regulate hyperactive CSTC circuitry.
- Genomic profiling: Large‑scale genome‑wide association studies (GWAS) aim to pinpoint overlapping genetic variants, opening doors to personalized medication.
While these remain experimental, they hint at a future where treatment is even more precise.
Frequently Asked Questions
Can skin‑picking be a symptom of OCD?
Yes. When the urge to pick is driven by an intrusive thought or a need to reduce anxiety, it qualifies as an OCD‑related compulsion rather than a simple habit.
How is excoriation disorder diagnosed?
A clinician uses DSM‑5 criteria: recurrent skin‑picking, attempts to stop or decrease the behavior, marked distress or impairment, and the behavior isn’t better explained by another medical condition.
Do SSRIs help with skin‑picking?
Research shows modest improvement in both OCD and BFRBs when SSRIs are combined with therapy. They rarely eliminate the urge on their own.
Is habit reversal training effective for OCD?
HRT is specifically built for body‑focused repetitive behaviors. When OCD includes a physical compulsion like skin‑picking, HRT can be a valuable complement to ERP.
What should I do if my dermatologist says "just stop picking"?
Ask for a referral to a mental‑health professional who specializes in OCD or BFRBs. The urge is often driven by underlying anxiety, and a therapist can teach strategies to manage it.
Understanding the bridge between OCD and excoriation disorder turns a confusing pattern into a treatable condition. By recognizing the shared brain pathways, seeking combined care, and applying evidence‑based therapies, individuals can break the cycle and reclaim healthier skin and mind.






Jeremy Lysinger
Great rundown-definitely a spot-on guide for anyone battling both OCD and skin‑picking!
Nelson De Pena
Thanks for the thorough breakdown. The CSTC circuit you mentioned is indeed a common thread linking the two disorders. Functional MRI studies have repeatedly shown hyperactivity in this loop during both compulsive hand‑washing and picking episodes. It’s also worth noting that SSRIs tend to dampen that over‑activation, which explains their cross‑diagnostic utility. Your table comparing features makes the distinction crystal clear.
Wilson Roberto
Reading this piece reminded me of the age‑old debate about whether compulsions are merely habits or deeper expressions of the self. When an obsession fuels a skin‑picking urge, the boundary between thought and action blurs, suggesting a shared phenomenology. The article’s emphasis on emotional regulation aligns with existential views that we seek meaning even in self‑destructive loops. Moreover, the suggestion to log urges reflects a mindfulness tradition that observes without judgment. Neurofeedback, although still experimental, could be the modern analogue of ancient contemplative practices. By training the brain to notice its own circuitry, we may cultivate a meta‑awareness that weakens the habit‑loop. It also raises ethical questions about how far we should intervene in someone’s internal experience. Ultimately, integrating psychotherapy with neuro‑technology could reshape our understanding of agency.
Narasimha Murthy
While the philosophical framing is engaging, the article overlooks a critical methodological limitation: most imaging studies rely on small, self‑selected samples. This raises concerns about the generalizability of the CSTC hyperactivity claim across diverse populations. Additionally, the emphasis on SSRIs glosses over the substantial side‑effect profile that many patients experience. A more rigorous meta‑analysis would strengthen the argument rather than relying on anecdotal case studies.
Samantha Vondrum
Thank you for highlighting those methodological concerns. It is indeed essential to acknowledge sample size and side‑effect considerations when evaluating treatment efficacy. Future research should aim for larger, more heterogeneous cohorts and transparently report adverse events. Such rigor will ultimately benefit clinicians and patients alike by providing clearer guidance.
Kelvin Egbuzie
Oh, sure, because having a perfectly polished paper solves the lived reality of someone stuck in a picking cycle 🙄. While the call for larger studies sounds noble, the funding pipelines for BFRB research are about as robust as a tissue paper bridge.
Katherine Collins
i guess the article could've been shorter lol.
Taylor Nation
You’re right that brevity can be powerful, but condensing the neurobiology into a few lines risks oversimplifying a complex issue. A balanced approach that maintains depth while staying concise would serve both newcomers and seasoned clinicians.
Nathan S. Han
The intertwining of obsessive‑compulsive disorder and excoriation disorder reads like a narrative of two twin fires feeding off one another, each flare illuminating the other's shadows. From a neurobiological perspective, the cortico‑striato‑thalamo‑cortical loop acts as the shared hearth where repetitive behaviors are kindled. When the loop misfires, the brain's error‑monitoring systems send distress signals, prompting compulsions that momentarily quench the anxiety. In the case of skin‑picking, that quenching takes the form of tactile stimulation, a fleeting release that the mind misinterprets as relief. This mechanistic overlap explains why selective serotonin reuptake inhibitors, which elevate serotonin across vast neural networks, can dampen both the intrusive thoughts of OCD and the urge to pick. Yet pharmacology alone is like handing someone a match without teaching them to build a fire safely; behavioral strategies remain indispensable. Cognitive‑behavioral therapy, especially exposure‑response prevention, trains the individual to sit with discomfort without resorting to ritualized actions. Habit reversal training, on the other hand, introduces a competing response that redirects the motor pattern toward a benign alternative, such as clenching fists or squeezing a stress ball. When combined, these modalities create a two‑pronged attack: one targeting the cognitive narrative, the other reshaping the physical habit loop. The article wisely recommends tailoring treatment to the dominant symptom-an approach that honors the uniqueness of each client’s presentation. Moreover, integrating dermatologic interventions, like silicone gels, serves as a physical barrier that can break the feedback loop between visual cues and picking behavior. Still, clinicians must remain vigilant for comorbid conditions, such as depression or ADHD, which can exacerbate both disorders. Ignoring these co‑occurring diagnoses would be akin to treating a fire while ignoring the underlying dry timber. Future directions, such as real‑time fMRI neurofeedback, promise a frontier where patients might learn to observe their own neural activity and intervene before the compulsion erupts. Genomic profiling, meanwhile, may one day allow us to predict who is most vulnerable to these overlapping disorders and intervene preemptively. In the meantime, a multidisciplinary team-psychiatrists, psychologists, and dermatologists-offers the most comprehensive safety net for those navigating this tangled terrain.
Ed Mahoney
Wow, a novel 16‑sentence dissertation on neural loops-who needs a TL;DR when you’ve got a mini‑thesis sitting in the comments? Maybe next time we can condense the whole neuropsychology textbook into a meme.
Brian Klepacki
The theatrical flair is appreciated, yet the essence remains: without concrete, accessible strategies, the labyrinthine explanations risk alienating those who need help most. Let’s bring the drama back to the bedside, where simple tools can change lives.
Shermaine Davis
I hear you. Simple steps like a daily log or a bandage can really help, and I’m glad we’re all pushing for real help.