When your pharmacist hands you a different pill than what your doctor prescribed, it’s not a mistake-it’s Medicare Part D substitution. But not all substitutions are allowed, and not all plans let you switch freely. If you’re on Medicare and take prescription drugs, understanding how substitution works could save you hundreds-or even thousands-of dollars a year.
What Exactly Is Medicare Part D Substitution?
Medicare Part D substitution happens when a pharmacist gives you a different drug than the one your doctor wrote on the prescription. This usually means swapping a brand-name drug for a generic version, or switching between two drugs in the same therapeutic class. It’s legal, common, and often encouraged-if your plan allows it and your doctor hasn’t said "do not substitute." But here’s the catch: it’s not automatic. Every Medicare Part D plan has its own formulary-a list of drugs it covers-and each drug is placed on a specific tier. The tier determines how much you pay. Generics are usually on Tier 1 with the lowest copay. Brand-name drugs? They’re often on Tier 3 or 4, meaning you pay more. If your plan allows substitution, the pharmacist can swap your brand-name drug for a generic on a lower tier-unless your doctor wrote "dispense as written" or "no substitution."How Formularies Control What You Can Switch To
Your plan’s formulary is the rulebook for substitution. In 2025, most Part D plans use a five-tier system:- Tier 1: Preferred generics (lowest cost)
- Tier 2: Non-preferred generics
- Tier 3: Preferred brand-name drugs
- Tier 4: Non-preferred brand-name drugs
- Tier 5: Specialty drugs (highest cost)
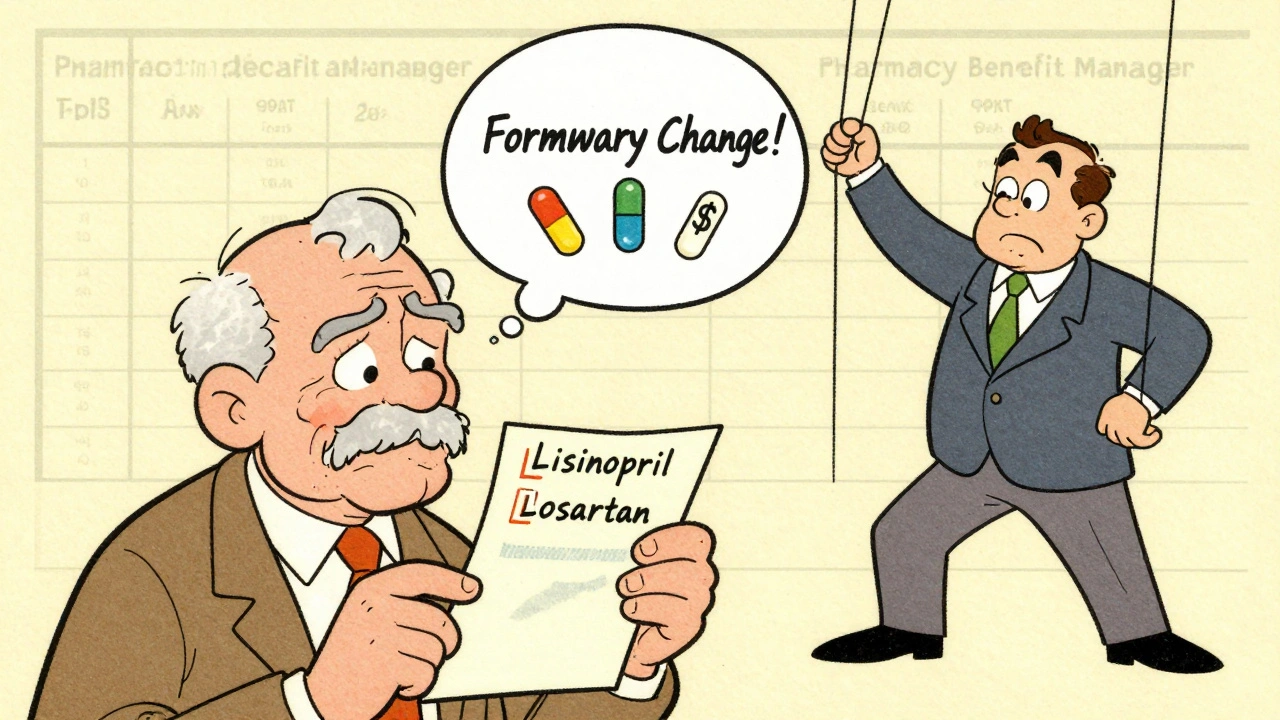
Pharmacy Benefit Managers (PBMs) like CVS Caremark, OptumRx, or Express Scripts create these formularies for Medicare plans. They decide which drugs get covered, which ones get preferred status, and which substitutions are allowed. That means two people on different Part D plans could have completely different options for the same condition.
Therapeutic Interchange: When You Get a Different Drug, Not Just a Generic
Sometimes, substitution isn’t just about swapping a brand for a generic. It’s about switching from one brand to another brand in the same drug class-called therapeutic interchange. For example, if your doctor prescribed Lisinopril for high blood pressure, your plan might allow substitution with Losartan, another blood pressure drug in the same family.This kind of substitution usually requires step therapy or prior authorization. Step therapy means you have to try a cheaper drug first. If it doesn’t work, your doctor can request to switch you to the original drug. Prior authorization means your doctor has to call or submit paperwork to prove the original drug is medically necessary.
These rules exist because insurers want to control costs. But they can create delays. If you’re on a drug that works well and suddenly get switched, you might have side effects or find it less effective. That’s why it’s critical to know your plan’s rules before you enroll.
The $2,000 Out-of-Pocket Cap Changes Everything in 2025
One of the biggest changes in 2025 is the new $2,000 annual cap on out-of-pocket drug costs. Before this, beneficiaries hit the "donut hole"-a coverage gap where they paid 100% of drug costs until they qualified for catastrophic coverage. That gap created a mess for substitution. People would avoid switching drugs mid-year because they didn’t want to reset their spending.Now, once you hit $2,000 in out-of-pocket costs (including what you paid, what your plan paid, and what manufacturers paid), you enter catastrophic coverage. After that, you pay nothing for covered Part D drugs for the rest of the year. That means substitution becomes less risky. If you’re close to the cap, switching to a cheaper drug might not matter-you’re about to pay nothing anyway.
But here’s the flip side: if you’re still early in the year and under the cap, switching to a higher-cost drug could push you closer to the limit faster. That’s why knowing your plan’s tiers and your current spending matters.
What You Can Do to Avoid Surprises
You don’t have to guess how substitution works. Here’s what to do before you fill your next prescription:- Check your plan’s formulary. Every plan publishes its drug list online. Search for each of your medications. Note the tier and whether generics are allowed.
- Call your pharmacy. Ask: "If I fill this prescription today, will you substitute it?" They’ll know your plan’s rules.
- Ask your doctor to write "dispense as written" if you’re sensitive to changes. This blocks substitution unless you approve it.
- Review your plan every year during Open Enrollment (Oct 15-Dec 7). Formularies change. A drug you got last year might be moved to a higher tier-or dropped entirely.
- Use Medicare’s Plan Finder tool. Enter your drugs and zip code. It shows you which plans cover them at the lowest cost.
Many people don’t realize that switching plans mid-year is possible if you have a qualifying event-like moving, losing other coverage, or getting into a nursing home. But for most, Open Enrollment is your only chance to fix a bad substitution situation.
Real-Life Scenarios: What Happens When Substitution Goes Wrong
Maria, 72, takes Metformin for diabetes. Her plan switched her from the brand-name Glucophage to a generic. She had no issues. But last year, her plan dropped the generic and switched her to another brand-Sitagliptin-without telling her. She didn’t notice until her blood sugar spiked. Her doctor had to file a prior authorization to get her back on the original drug. It took three weeks.James, 68, takes a specialty drug for rheumatoid arthritis. His plan wouldn’t cover it unless he tried a cheaper biologic first. He refused because he’d already tried it-and it didn’t work. He had to appeal. The plan denied him twice. He finally got approval after his doctor wrote a letter explaining his medical history.
These aren’t rare cases. In 2025, nearly 1 in 4 Medicare Part D beneficiaries reported a drug substitution they didn’t expect. Many said it caused confusion, delays, or worse health outcomes.
What About Insulin and Other High-Cost Drugs?
The Inflation Reduction Act didn’t just cap out-of-pocket spending-it also capped insulin costs at $35 per month for all Part D plans. That’s a game-changer. Even if your plan doesn’t cover your insulin brand, you still pay no more than $35. Some plans, like Humana’s, even offer this cap before you hit the $2,000 limit.Other drugs are getting similar protections. For example, certain vaccines and diabetes supplies are now fully covered with no cost-sharing. But these protections don’t apply to all drugs. Substitution still matters for most prescriptions.

Why Some Plans Don’t Allow Substitution at All
Not every plan lets pharmacists substitute drugs. Some plans, especially Medicare Advantage plans with drug coverage (MA-PDs), tie substitution to their medical benefits. If your plan covers both your doctor visits and your prescriptions, they might limit substitution to keep you in a specific network of providers or drugs.Also, some plans intentionally restrict substitution to keep you on a drug that earns them rebates from manufacturers. This isn’t illegal, but it’s not always in your best interest. That’s why reviewing your plan’s formulary every year is non-negotiable.
What Happens If You Get a Substituted Drug and It Doesn’t Work?
If a substituted drug causes side effects or doesn’t control your condition, you have rights:- You can ask your doctor to request a formulary exception-a formal request to cover your original drug.
- You can file an appeal if the plan denies your request.
- You can switch plans during Open Enrollment or during a Special Enrollment Period if your drug is removed from the formulary.
Don’t wait until your medication runs out. Start the process early. It can take up to 72 hours for a formulary exception to be approved. If you’re in a health crisis, you can request an expedited review.
Final Takeaway: Know Your Plan, Know Your Drugs
Medicare Part D substitution isn’t a mystery-it’s a system built to save money. But it only works if you’re in control. The rules vary by plan, by drug, and by your spending level. The $2,000 cap in 2025 makes substitution less risky, but it doesn’t remove the need to be proactive.Don’t assume your pharmacist knows what’s best. Don’t assume your doctor’s prescription will be filled as written. And don’t wait until you’re out of pills to realize your plan changed its rules.
Check your formulary. Ask questions. Speak up. Your health-and your wallet-depend on it.
Can my pharmacist substitute my Medicare Part D drug without telling me?
Yes, unless your doctor wrote "dispense as written" or "no substitution" on the prescription. Pharmacists are allowed to substitute generic versions or equivalent drugs if your plan permits it. But they must inform you if a substitution occurs. If you’re not told, ask your pharmacist for a copy of the original prescription and the substituted drug’s label. You have the right to know what you’re taking.
What if my plan drops my drug from the formulary?
If your drug is removed from your plan’s formulary, you’ll get a notice at least 60 days before the change takes effect. You can request a one-time refill of your current prescription, file a formulary exception, or switch plans during Open Enrollment. If you’re in the middle of treatment and the drug is essential, you can request an expedited exception. Don’t stop taking your medication-act quickly.
Do I have to pay more if I get a brand-name drug instead of a generic?
Yes, almost always. Brand-name drugs are on higher tiers, meaning you pay more in coinsurance or copayments. For example, a generic might cost $10, while the brand version costs $50 or more. The difference adds up fast-especially if you take multiple drugs. That’s why substitution to generics is encouraged: it lowers your out-of-pocket costs and helps your plan stay affordable.
Can I switch plans mid-year if substitution issues arise?
Usually, no. You can only switch plans during the Annual Enrollment Period (Oct 15-Dec 7). But there are exceptions: if you move to a new area, lose other coverage, qualify for Extra Help, or enter a nursing home, you may qualify for a Special Enrollment Period. If your drug is removed from your plan’s formulary, you can switch plans outside of Open Enrollment. Always check with Medicare or your plan for eligibility.
Why do some drugs have no generic substitutes?
Some drugs are biologics, complex medications made from living cells-like those for rheumatoid arthritis, cancer, or multiple sclerosis. These drugs don’t have true generics; instead, they have "biosimilars," which are similar but not identical. Many Part D plans cover biosimilars as substitutes, but not always. Even if a biosimilar exists, your plan might not include it on the formulary. Always check your plan’s list before assuming a substitute is available.







James Kerr
Just had to switch my dad’s blood pressure med last month - same tier, same effect, saved us $40 a month. 🙌 Medicare’s weird rules make sense when you see the savings.
Rashmin Patel
OMG YES. My mom got switched from Lisinopril to Losartan without a heads-up and she ended up in the ER with dizziness. 😣 Pharmacies think they’re doctors, but if your doc says ‘do not substitute,’ they should listen. And don’t get me started on how PBMs push cheaper drugs even when they’re useless for certain people. It’s not about cost - it’s about control. And it’s messed up. I’ve been fighting this for 3 years. Every year I have to appeal. Every year they say ‘it’s fine.’ It’s NOT fine. 🤬
sagar bhute
Typical. Another article pretending this system isn’t broken. Pharmacists aren’t ‘helping’ - they’re following corporate scripts written by PBMs who get kickbacks from drug companies. If you’re not on a plan that forces you into biosimilars for RA drugs, you’re lucky. Most people don’t even know they’re being swapped until their symptoms get worse. This isn’t savings. It’s medical roulette.
Rashi Taliyan
My aunt got switched to a generic insulin last year - didn’t realize it until her sugar went wild. She cried for a week. I had to call 6 different offices just to get her old one back. 🥲 They never told her it changed. Never. And now they want us to trust the system? No thanks. I check every pill now. Every. Single. One.
shalini vaishnav
Why are Americans so clueless about this? In India, we know that generics are just as good - no drama. People here treat pharmacy substitutions like a conspiracy. If your doctor prescribed a drug, and it works, fine. But if it doesn’t? Switch. Stop acting like your body is fragile. We’ve had generics for decades. This overprotection is just fear-mongering.
vinoth kumar
Biggest tip I learned: always ask the pharmacist, ‘Is this the exact same as what’s on the script?’ If they say ‘yes’ but the pill looks different, ask for the old one and the new one side by side. I did this last month - turned out they swapped my metformin for a different generic that had a weird coating. Made me nauseous. They fixed it right away. Just ask. No shame.
bobby chandra
Let’s be real - the $2,000 cap is a game-changer. Last year I was hitting the donut hole by June. This year? I switched to a $120 brand-name med in March. Why? Because I knew I’d hit the cap by October. Now I’m paying $0 for everything. That’s not a loophole - that’s strategy. Stop treating substitution like a threat. Treat it like a puzzle. And win.
Archie singh
Formularies are designed to maximize profit not health. PBMs get rebates from brand-name manufacturers to keep you on expensive drugs. That’s why you get switched to a Tier 4 drug instead of a Tier 1 generic. It’s not about cost - it’s about kickbacks. The system is rigged. And no, the $2,000 cap doesn’t fix it. It just makes people feel better while they’re still being manipulated.
Gene Linetsky
Why are people surprised by this? The entire system is built on substitution. It’s how insurance works. If you don’t want to be swapped, pay cash or get a private plan. Medicare is a public program. It’s not meant to give you luxury options. Accept it or opt out.
James Kerr
Actually, that’s a good point. My mom’s plan just dropped her favorite generic. She got a notice. We appealed. Got it back. Took 10 days. But if I hadn’t been on top of it? She’d have been stuck with a $90 alternative. So yeah - stay loud. Stay on it. That’s the only way this system works.