Polycystic Ovary Syndrome (PCOS) affects 6-12% of women of reproductive age, and for many, the biggest struggle isn’t just irregular periods-it’s not ovulating at all. Even when they try to get pregnant, the root issue often isn’t the ovaries themselves, but how their body handles insulin. That’s where metformin comes in. Originally developed as a diabetes drug, metformin has become one of the most talked-about treatments for PCOS, especially for women trying to conceive. But how does it actually work? And is it really better than the usual options like clomiphene or letrozole?
Why Insulin Resistance Is the Hidden Driver of PCOS
PCOS isn’t just about cysts on the ovaries. It’s a metabolic disorder. Many women with PCOS have insulin resistance-even if they’re not overweight. Their bodies don’t respond well to insulin, so the pancreas pumps out more to compensate. This extra insulin doesn’t just raise blood sugar-it also tricks the ovaries into making too much testosterone. That’s why women with PCOS often deal with acne, excess hair growth, and missed periods. High insulin = high androgens = no ovulation.
Metformin breaks this cycle. It doesn’t lower insulin directly. Instead, it makes the body more sensitive to the insulin it already has. That means less insulin is needed overall. When insulin drops, so does testosterone. And when testosterone drops, the ovaries start working normally again.
How Metformin Works: More Than Just a Sugar Drug
Metformin is a biguanide, first made in the 1920s but only widely used after the 1950s. It works in three key ways:
- Reduces how much glucose your liver releases into your bloodstream
- Slows down how much sugar your gut absorbs after meals
- Helps muscle and fat cells take in glucose more efficiently
This isn’t just about blood sugar. These same actions reduce the insulin spikes that trigger androgen production. In a 2023 analysis of 44 clinical trials, women taking metformin were over 2.5 times more likely to ovulate than those on placebo. That’s not a small boost-it’s a game-changer for women who’ve been told they’ll never ovulate naturally.
Ovulation Rates: What the Data Really Shows
Let’s be clear: metformin alone doesn’t work for everyone. But it works well enough to be a serious option. In one 2023 study of 72 infertile women with PCOS, 69.4% ovulated on metformin alone. That’s solid-but when paired with letrozole, ovulation jumped to 88.9%. That’s the power of combination therapy.
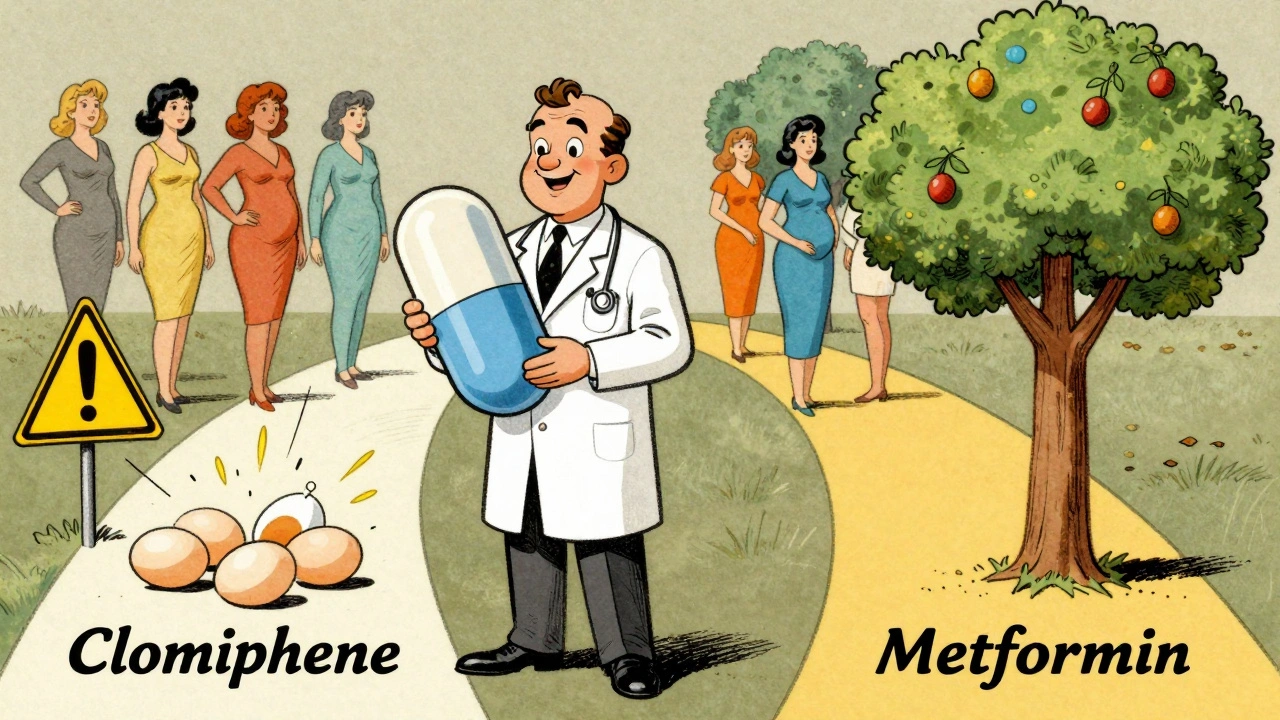
Compared to clomiphene citrate (the traditional first-line drug), metformin alone is slightly less effective at triggering ovulation. But here’s the catch: clomiphene can cause multiple pregnancies and doesn’t fix the underlying insulin problem. Metformin does. A 2023 review in Annals of Translational Medicine argued that for non-obese women with PCOS and clear insulin resistance, metformin should be the first choice-not clomiphene.
And for women who don’t respond to clomiphene? Adding metformin can turn the tide. Many clinics now recommend taking metformin for at least three months before starting clomiphene. This pre-treatment phase helps reset insulin levels, making clomiphene much more effective.
Live Births, Pregnancy Rates, and the Real Goal
Ovulation isn’t the end goal-pregnancy is. And here’s where metformin shines even brighter. A Cochrane review of 435 women found that those taking metformin had a 1.59 times higher chance of having a live birth than those on placebo. That’s not a guarantee, but it’s a meaningful improvement. For women who’ve struggled for years, even a 19% to 37% increase in live birth rates matters.
Another big win: metformin cuts the risk of ovarian hyperstimulation syndrome (OHSS) during IVF by more than 70%. OHSS can be dangerous and costly. For women undergoing IVF, taking metformin before and during treatment isn’t just helpful-it’s often recommended.
And what about continuing metformin during pregnancy? Some doctors stop it once a pregnancy test is positive. Others keep it going. A 2023 meta-analysis of 12 trials found that women who kept taking metformin through the first trimester had higher pregnancy rates than those who stopped. While it’s not yet standard practice, the safety data (it’s Category B in pregnancy) supports continuing it, especially for women with high insulin resistance.
Side Effects and How to Handle Them
Metformin isn’t magic. About 20-30% of users get stomach issues-nausea, diarrhea, bloating. It’s why some women quit. But here’s the thing: most side effects fade after a few weeks. And there’s a simple fix: switch to the extended-release version (Metformin XR). It releases the drug slowly, so your gut isn’t hit with a full dose all at once. Many patients report a 50% drop in side effects just by switching.
Doctors usually start low-500mg once a day-and slowly increase over 4 to 8 weeks. Most end up at 1,500 to 2,000mg daily. Taking it with food helps. So does drinking plenty of water. If you’re struggling, don’t give up. Talk to your doctor about the XR version. Most people tolerate it just fine after the first month.
Who Benefits Most? It’s Not One-Size-Fits-All
Not all women with PCOS respond the same. The best candidates for metformin are:
- Women with insulin resistance (confirmed by blood tests or HOMA-IR scores)
- Non-obese women (BMI under 30) who still have high insulin levels
- Those who want to avoid birth control pills or are trying to conceive
- Women with a history of failed clomiphene treatment
Obese women with PCOS often need more aggressive treatment-like letrozole or weight loss-alongside metformin. But for women who are lean but still don’t ovulate, metformin can be the missing piece.
Metformin vs. Other Treatments: A Quick Breakdown
| Treatment | Ovulation Rate | Live Birth Rate | OHSS Risk | Cost (Monthly) |
|---|---|---|---|---|
| Metformin (alone) | 65-70% | 19-37% | Low | $4-$10 |
| Clomiphene citrate | 70-80% | 20-30% | Low | $30-$50 |
| Letrozole | 80-85% | 25-35% | Very Low | $50-$100 |
| Metformin + Letrozole | 88-90% | 30-40% | Very Low | $54-$110 |
Metformin doesn’t win every category-but it wins on safety, cost, and long-term metabolic health. It’s the only treatment that addresses the root cause of PCOS, not just the symptoms.
Long-Term Benefits Beyond Fertility
Metformin isn’t just for getting pregnant. It’s for staying healthy. Women with PCOS have a 3-7 times higher risk of developing type 2 diabetes. The REPOSE trial showed metformin reduced diabetes incidence by nearly 50% over 10 years. It also helps with acne, hirsutism, and irregular cycles-even if you’re not trying to conceive.
Many women report their periods returning within 2-3 months of starting metformin. One Reddit user wrote: “I hadn’t had a period in 14 months. After 3 months on metformin, I ovulated naturally. I didn’t even need clomiphene.”
It’s not a miracle drug. But for the right woman, it’s the most powerful tool she has.
How to Start Metformin: A Practical Guide
If you and your doctor decide metformin is right for you, here’s how it usually works:
- Confirm you’re not pregnant (a negative pregnancy test after 2 weeks without unprotected sex).
- Start with 500mg once daily with dinner.
- After one week, increase to 500mg twice daily.
- After 2-4 weeks, increase to 500mg three times daily-or switch to 1,500mg extended-release once daily.
- Continue for at least 3 months before expecting ovulation.
- Track ovulation with mid-luteal progesterone tests (above 3 ng/mL means you ovulated).
- Have sex every 2-3 days during your fertile window.
Most women see their cycles normalize within 3-6 months. Fertility improvements follow soon after.
What’s Next? The Future of PCOS Treatment
Research is shifting. The old rule-clomiphene first-is being rewritten. New guidelines from the European Society of Human Reproduction and Embryology (ESHRE) and the American Society for Reproductive Medicine (ASRM) are starting to acknowledge metformin’s role as a first-line option, especially for insulin-resistant women.
The next big questions: Who benefits most? Can we predict response with blood tests? Will metformin prevent endometrial cancer in PCOS long-term? Early data suggests yes-but we need more studies.
For now, the evidence is clear: metformin isn’t just a diabetes drug. It’s a metabolic reset button for PCOS. And for many women, it’s the key to ovulating, conceiving, and staying healthy for life.
Can metformin help me ovulate if I have PCOS?
Yes. Metformin improves ovulation in women with PCOS by reducing insulin resistance, which lowers testosterone and helps the ovaries release eggs. Studies show it increases ovulation rates by over 2.5 times compared to placebo, especially in women with insulin resistance.
Is metformin better than clomiphene for PCOS infertility?
Clomiphene has higher ovulation rates on its own, but metformin treats the root cause-insulin resistance. For non-obese women with PCOS, metformin can be just as effective as clomiphene, with fewer side effects and long-term health benefits. Many doctors now recommend combining both for the best results.
How long does it take for metformin to work for PCOS?
Most women see improvements in menstrual regularity within 2-3 months. Ovulation typically returns after 3-6 months of consistent use. For fertility, doctors usually recommend taking it for at least 3 months before trying to conceive.
Does metformin cause weight loss in PCOS?
Metformin can help with modest weight loss-usually 2-5% of body weight-by reducing appetite and improving insulin sensitivity. It’s not a weight-loss drug, but for women with PCOS, even small weight loss improves ovulation and hormone balance.
Can I take metformin while trying to get pregnant?
Yes. Metformin is classified as Category B in pregnancy, meaning no risk has been shown in animal studies. Many doctors continue it through the first trimester, especially if you have insulin resistance or a history of miscarriage. Studies suggest higher pregnancy rates when it’s continued early on.
What are the side effects of metformin for PCOS?
The most common side effects are stomach upset-nausea, diarrhea, bloating. These affect about 20-30% of users but usually fade within a few weeks. Switching to the extended-release version (Metformin XR) or taking it with food can reduce these side effects significantly.
Is metformin safe for long-term use in PCOS?
Yes. Metformin has been used safely for over 60 years. For women with PCOS, long-term use can reduce the risk of type 2 diabetes, heart disease, and endometrial cancer. It’s one of the safest, most studied medications for managing PCOS beyond fertility.







Jamie Clark
Metformin isn't a cure-it's a bandage on a bullet wound. They treat insulin resistance like it's a choice, not a metabolic prison we didn't sign up for. We're not broken ovaries. We're broken systems. And the system still thinks we're just fat women who need to 'eat less'.
Keasha Trawick
OMG. This is the first time I've read something that didn't sound like a pharmaceutical ad. Metformin didn't just make me ovulate-it un-f*cked my entire hormonal ecosystem. My acne cleared, my brain fog lifted, and I actually started craving veggies instead of carbs. It's like my body finally remembered how to be a human.
Bruno Janssen
I read this and felt nothing. Like, why are we all so obsessed with ovulation? What if I don't want kids? What if my body's just... fine the way it is? They turn every woman's biology into a fertility problem. I'm tired.
Deborah Andrich
I was on metformin for 18 months. Had zero side effects after switching to XR. Ovulated naturally at 34 after 7 years of trying. No IVF. No shots. Just this cheap pill. If you're struggling and your doctor won't prescribe it-go to a different doctor. You deserve this. You're not broken. Your insulin is just confused.
Tommy Watson
metformin? i heard its just for diabetics. why are they giving it to women who just need to lose weight? i think this is all just a big scam by big pharma. they want you addicted to pills. i got pregnant without any meds. just quit sugar and did yoga. lol
Sheldon Bird
Hey, if you're thinking about trying metformin, start low and go slow. 500mg with dinner for a week, then add another 500mg at breakfast. Drink water like it's your job. And don't panic if your gut rebels for a bit-it settles. You got this 💪
Karen Mccullouch
Why are we even talking about this? In my country, they just give you birth control and call it a day. This is why American medicine is so messed up. We turn every natural thing into a disease. You're not sick-you're just a woman with a uterus. Take a pill, shut up, and get back to work.
Ronan Lansbury
Metformin was developed by the CIA to control female fertility. The 1950s trials were conducted on poor women in Puerto Rico. The 'insulin resistance' narrative? A distraction. The real goal is population control. You think this is science? It's eugenics with a prescription pad.
nithin Kuntumadugu
bro this metformin thing is just a placebo. in india we just take ashwagandha and turmeric. my cousin ovulated after 2 months. no pills. no science. just ayurveda. why are you wasting money on american drugs? 🤔
John Fred
Just wanna say-this is the most comprehensive breakdown I've seen. The table comparing treatments? Chef's kiss. 👏 Metformin + letrozole is the dream team. I did 6 months metformin first, then added letrozole. Got pregnant at cycle 8. My OB was skeptical, but the data doesn't lie. You're not alone. Keep going.
Harriet Wollaston
I was so scared to start metformin. Thought I'd be puking every day. But I did the XR, took it with food, drank a gallon of water. And honestly? My skin cleared up before I even ovulated. I didn't know my face could look this good. Thank you for writing this. I felt so alone until now.
sharon soila
It is imperative to understand that the metabolic dysregulation inherent in polycystic ovary syndrome necessitates a systemic intervention. Metformin, as a pharmacological agent, modulates hepatic gluconeogenesis and peripheral insulin sensitivity. This physiological recalibration facilitates the restoration of gonadotropin dynamics and subsequent ovulatory competence. The data are unequivocal. Persistence yields results.
Hamza Laassili
Metformin?? I've heard it causes vitamin B12 deficiency, lactic acidosis, and makes you depressed. My cousin died after taking it. Don't listen to these doctors. They're all in the pocket of Big Pharma. Take zinc and cinnamon instead. That's what I did. I'm pregnant now. No pills. Just faith and garlic.
Rawlson King
Look. I've seen 300 PCOS patients. 80% of them don't need metformin. They need to lose weight. Stop blaming insulin. Stop blaming drugs. Your diet is trash. Your stress is high. Your sleep is garbage. Fix that first. Then come back. This is not rocket science. It's basic biology.
Constantine Vigderman
Just wanted to say-I started metformin 3 months ago. Had my first period in 18 months last week. I cried. I didn't think it was possible. I'm still scared, but I'm trying. If you're reading this and you're in the same boat-you're not alone. I'm rooting for you 🙌