Heartburn vs. Severe Stomach Pain Checker
When a burning sensation climbs up your chest and a sharp ache twists in your belly, you might wonder whether it’s just heartburn or something more serious like severe stomach pain. Knowing the difference can save you from unnecessary panic and help you seek the right treatment faster.
Key Takeaways
- Heartburn is an acid‑related burn that usually starts behind the breastbone and rises after meals.
- Severe stomach pain often points to deeper issues such as ulcers, gallstones, or pancreatitis.
- Location, timing, and accompanying symptoms are the best clues to tell them apart.
- When pain is sudden, intense, or linked with fever, vomiting, or black stools, seek medical help immediately.
- Lifestyle tweaks-like avoiding trigger foods, eating smaller meals, and managing stress-can reduce both conditions.
What Exactly Is Heartburn?
Heartburn is a burning sensation that occurs when stomach acid flows back into the esophagus, the tube that connects the throat to the stomach. It’s technically a symptom of gastro‑esophageal reflux disease (GERD), but occasional acid reflux can happen to anyone.
The classic sign is a hot, uncomfortable feeling behind the breastbone that may rise toward the throat, often after a big or spicy meal, when you lie down, or when you’re under stress.
What Does Severe Stomach Pain Look Like?
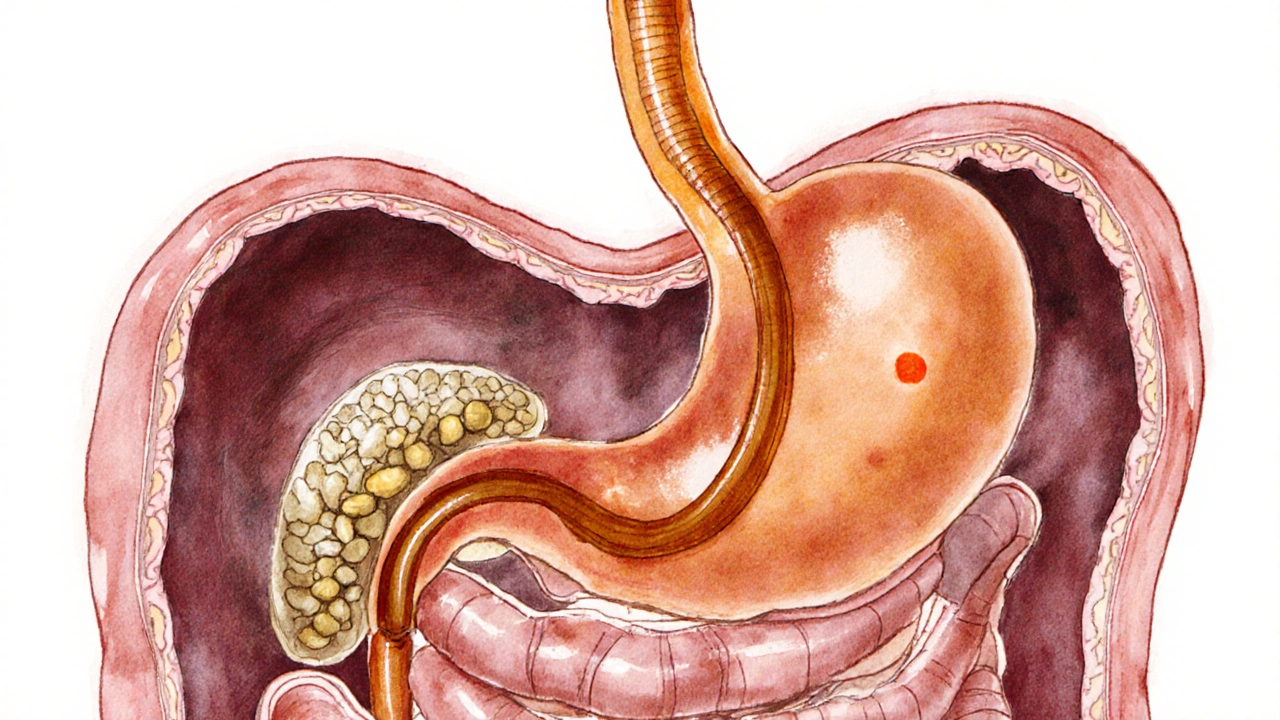
Severe stomach pain is a deep, often cramping or stabbing discomfort that originates in the abdomen. It can be constant or come in waves and may radiate to the back, chest, or shoulder.
Unlike heartburn, the pain usually sits lower in the belly and can be linked to a variety of organs: the stomach, gallbladder, pancreas, or intestines. Common causes include peptic ulcers, gallstones, pancreatitis, and even infections.
Spotting the Differences: A Quick Comparison
| Feature | Heartburn | Severe Stomach Pain |
|---|---|---|
| Typical location | Behind breastbone, rises to throat | Lower abdomen, may radiate to back or shoulder |
| Common triggers | Spicy/fatty foods, caffeine, lying down | Alcohol, high‑fat meals, gallstones, ulcers |
| Accompanying symptoms | Sour taste, belching, hoarseness | Nausea, vomiting, fever, bloating |
| Pain quality | Burning, aching | Sharp, cramping, stabbing |
| When it worsens | After meals, when lying flat | During the night, after fatty meals, or with physical activity |
Common Causes Behind Each Symptom
Heartburn often stems from a relaxed lower esophageal sphincter (LES) that lets acid escape. Risk factors include obesity, smoking, pregnancy, and certain medications such as NSAIDs.
Severe stomach pain can be more varied. Here are the top culprits:
- Peptic ulcer: A sore in the stomach lining often caused by Helicobacter pylori infection or prolonged NSAID use.
- Gallbladder disease: Gallstones can block bile flow, leading to intense right‑upper‑quadrant pain.
- Pancreatitis: Inflammation of the pancreas, frequently linked to heavy alcohol use or gallstones.
- Food poisoning or viral gastroenteritis: Usually accompanied by diarrhea and vomiting.
- Irritable bowel syndrome (IBS): Chronic cramping pain with changes in bowel habits, often stress‑related.
When to See a Doctor
If you’re unsure whether you’re dealing with simple heartburn or something more severe, watch for red‑flag symptoms. Call your doctor or head to urgent care if you experience any of the following:
- Sudden, excruciating pain that doesn’t ease after 15‑20 minutes.
- Pain that spreads to the back, jaw, or left arm (could signal cardiac issues).
- Vomiting blood, coffee‑ground material, or material that looks like fresh blood.
- Black, tarry stools (sign of internal bleeding).
- Fever over 101°F (38.3°C) combined with abdominal pain.
- Persistent vomiting, especially if you can’t keep fluids down.
These signs may indicate ulcer perforation, gallbladder attack, pancreatitis, or even a heart attack, all of which need prompt medical attention.

Self‑Care Steps You Can Try at Home
For mild cases, lifestyle tweaks often do the trick. Here’s a practical checklist:
- Eat smaller, more frequent meals. Large meals stretch the stomach and push acid upward.
- Avoid trigger foods: citrus, tomato‑based sauces, chocolate, mint, fried or fatty foods, and caffeine.
- Stay upright for at least two hours after eating. Gravity helps keep acid where it belongs.
- Raise the head of your bed 6‑8 inches if night‑time reflux is a problem.
- Limit alcohol and quit smoking; both weaken the LES.
- Consider over‑the‑counter antacids for occasional heartburn, but avoid long‑term reliance without a doctor’s advice.
- If you suspect ulcer pain, talk to a clinician about a short course of proton‑pump inhibitors or H.pylori testing.
Preventing Future Episodes
While occasional heartburn is common, repeated bouts or chronic stomach pain deserve a deeper look. Regular check‑ups can catch problems early. Your doctor may recommend:
- Testing for H. pylori infection if ulcers are suspected. \n
- Ultrasound or CT imaging to evaluate gallbladder or pancreatic health.
- Blood work to rule out anemia, liver dysfunction, or inflammation markers.
- Dietary counseling for tailored meal plans that keep acid low and nutrients high.
Adopting a balanced diet rich in fiber, lean proteins, and healthy fats-not only supports digestion but also lowers the risk of reflux and ulcer formation.
Bottom Line
Understanding the difference between stomach pain and heartburn hinges on where the discomfort lives, what makes it worse, and what other signs appear. Heartburn burns in the chest after meals, while severe stomach pain sits lower and may signal gallstones, ulcers, or pancreatitis. When in doubt, especially with alarming symptoms, don’t wait-get professional care.
Frequently Asked Questions
Can heartburn cause severe stomach pain?
Heartburn itself usually produces a mild to moderate burning sensation. If you feel a deep, cramping pain in the abdomen, it’s likely coming from a different source such as an ulcer or gallbladder issue.
Is it safe to use antacids for severe stomach pain?
Antacids can neutralize acid temporarily, but they won’t treat underlying problems like ulcers or pancreatitis. Using them repeatedly without a doctor’s guidance may mask serious conditions.
What foods should I avoid to reduce heartburn?
Common triggers include citrus fruits, tomatoes, chocolate, mint, fried foods, fatty cuts of meat, caffeine, and carbonated beverages. Keeping a food diary helps pinpoint personal triggers.
When does stomach pain indicate an emergency?
Seek emergency care if the pain is sudden and severe, if you have a fever, vomiting blood, black stools, or if the pain spreads to the back, jaw, or left arm. These signs could mean a perforated ulcer, gallbladder attack, pancreatitis, or a cardiac event.
Can stress make both heartburn and stomach pain worse?
Yes. Stress can increase stomach acid production and slow digestion, amplifying both reflux symptoms and abdominal cramps. Incorporating relaxation techniques like deep breathing or yoga can help reduce flare‑ups.


Julien Martin
Understanding the pathophysiology behind gastro‑esophageal reflux versus visceral nociception is essential for accurate self‑assessment. When the lower esophageal sphincter fails, acidic gastric contents ascend, producing the characteristic retrosternal burn. Conversely, deep visceral afferents signal ischemic or inflammatory processes in the stomach, gallbladder, or pancreas, often as sharp or cramping sensations. Pay close attention to temporal patterns: reflux typically escalates post‑prandially and when supine, while severe abdominal pain may radiate to the back and persist regardless of position. By correlating location, quality, and associated signs, you can triage effectively and seek timely medical evaluation.
Jason Oeltjen
Honestly it’s obvious that peopel should read the facts and not rely on vague online quizzes, because ignorance leads to bad health choices. If you keep ignoring the red‑flags you’re basically signing up for disaster and that’s just irresponsible. Take the advice seriously and stop making excuses.
Mark Vondrasek
It’s fascinating how quickly we all devolve into amateur diagnosticians when a twinge hits the chest, as if every symptom were a secret code planted by a hidden cabal to keep us guessing. The internet, of course, spawns endless conspiracy threads suggesting that pharmaceutical giants deliberately blur the lines between heartburn and ulcer pain to sell more antacids and PPIs. One moment you’re reading a reputable source, the next you’re told that the very notion of “acid reflux” is a government‑backed myth designed to trap citizens in a cycle of chronic medication. Meanwhile, the real culprits-copper‑coated pills, corporate lobbyists, and the shadowy board of “Gastro‑Health International”-sit smugly in boardrooms plotting the next wave of “research.” In truth, the body’s signals are not a theatrical performance for us to decipher; they’re urgent alerts that something is amiss. If you experience a burning sensation that climbs after a greasy meal, it’s likely just the LES taking a break, not a secret plot. However, if the pain is severe, sharp, or accompanied by fever, you might be confronting a genuine ulcer or even pancreatitis, which, unlike the conspiracy, does require actual medical attention. The absurdity lies in how many people ignore the red‑flag signs because they fear the “big pharma” narrative, only to end up in emergency rooms where they actually need help. So, before you blame shadowy organizations for your discomfort, consider that a straightforward explanation-acid reflux or an ulcer-might be the true answer. And remember, the only real conspiracy here is the one that keeps you from listening to qualified professionals.
Joshua Agabu
I tend to notice the burning more after coffee.
Lolita Rosa
The burning sensation feels like a battle inside my gut, a clash of forces that mirrors the turmoil we sometimes feel about our nation’s future, yet I stay silent, hoping the pain will simply fade like an ignored protest.
Rhiane Heslop
We must acknowledge that pain is a universal language it transcends borders and ideologies it reveals the fragile veil that separates comfort from suffering
Poppy Johnston
Take a moment each day to breathe deeply and note what triggers your discomfort; mindfulness can help you spot patterns and reduce anxiety around the symptoms. Pair this with a balanced diet, and you’ll likely see a gradual improvement. Remember, you’re not alone in this journey, and small lifestyle tweaks often yield big benefits over time.
Eric Parsons
When differentiating reflux from visceral pain, consider the temporal relationship to meals: reflux typically peaks within 30 minutes after eating, especially if the meal is high‑fat or spicy. In contrast, ulcer‑related pain may improve with antacids but often worsens on an empty stomach. Evaluate positional factors; lying flat often aggravates heartburn, whereas severe abdominal pain may intensify with movement or palpation. Pay attention to associated signs such as sour taste, which leans toward reflux, versus fever or black stools, which suggest a more serious gastrointestinal bleed. An appropriate over‑the‑counter trial of an H2 blocker can be diagnostic for mild reflux, but persistent or worsening pain warrants endoscopic assessment. Lifestyle modifications-weight management, smoking cessation, and avoiding trigger foods-are foundational for both conditions. Ultimately, a personalized approach based on symptom pattern and risk factors will guide the most effective management plan.
Mary Magdalen
The line between a harmless heartburn and a lurking ulcer can feel like walking a tightrope over a canyon of uncertainty, where every swallow is a potential misstep and each night of restless sleep paints a vivid mural of dread.
Dhakad rahul
Ah, the drama of the digestive duel! 🌶️ One minute you’re indulging in a feast, the next you’re dueling with a fiery dragon of acid, and the only sword you have is a bland cracker. 🎭
William Dizon
If you’re ever in doubt, it’s safest to consult a healthcare professional rather than rely solely on self‑assessment tools. Early evaluation can prevent complications and give you peace of mind.
Ira Bliss
Absolutely! 👏 Staying proactive about your health is the best gift you can give yourself. 🌟 If you notice any alarming signs, don’t hesitate to reach out to a doctor right away. 🚑
Donny Bryant
Remember, consistency in diet and posture can make a big difference. Keep monitoring your symptoms and act if they change.