Switching from a brand-name drug to a generic version is supposed to be seamless. The FDA says they’re the same-same active ingredient, same dose, same effect. But if you start feeling weird after the switch-headaches, dizziness, nausea, or worse-you’re not imagining it. And you’re not alone. Thousands of people report changes after switching, even when the science says it shouldn’t happen. The problem? Most don’t know how to report it. Or worse, they think it doesn’t matter. It does.
Why Side Effects Happen After Switching to Generics
Generic drugs are required to be bioequivalent to the brand-name version. That means they deliver the same active ingredient at the same rate and amount, within a narrow range (80%-125% of the brand). But bioequivalence doesn’t mean identical. The inactive ingredients-fillers, dyes, binders, coatings-can be different. And those matter. For some people, especially those with sensitivities or allergies, a different dye or preservative can trigger a reaction. A 2018 study found that patients switching to certain generics reported more side effects like swelling or fatigue than those staying on brand or authorized generics, even though the active drug was identical. It’s not always the drug. Sometimes, it’s perception. A 2021 Kaiser Family Foundation survey showed 42% of patients believe generics are less effective than brand-name drugs. That belief can make you more likely to notice and report side effects-even if they’re unrelated to the medication. But that doesn’t mean you should ignore them. If something changed after the switch, it’s worth reporting.What Counts as a Side Effect Worth Reporting
Not every mild symptom needs a report. But the FDA wants to hear about anything new, unexpected, or serious. Here’s what to look for:- Serious side effects: Hospitalization, life-threatening reactions, permanent disability, birth defects, or events requiring medical intervention to prevent lasting harm.
- Unexpected side effects: Symptoms not listed on the drug’s label. Even if they seem minor, if they’re new and you didn’t have them before, report them.
- Worsening symptoms: If you were stable on the brand and now your condition is getting worse-like higher blood pressure, more seizures, or worse depression-it counts.
- Reactions that disappeared after switching back: If you went back to the brand and the side effect vanished, that’s strong evidence it’s linked to the generic.
Don’t wait for something to be “bad enough.” The FDA’s system relies on people speaking up. One report might seem small. But 50 reports of the same issue? That’s a signal.
How to Report: The Simple 5-Step Process
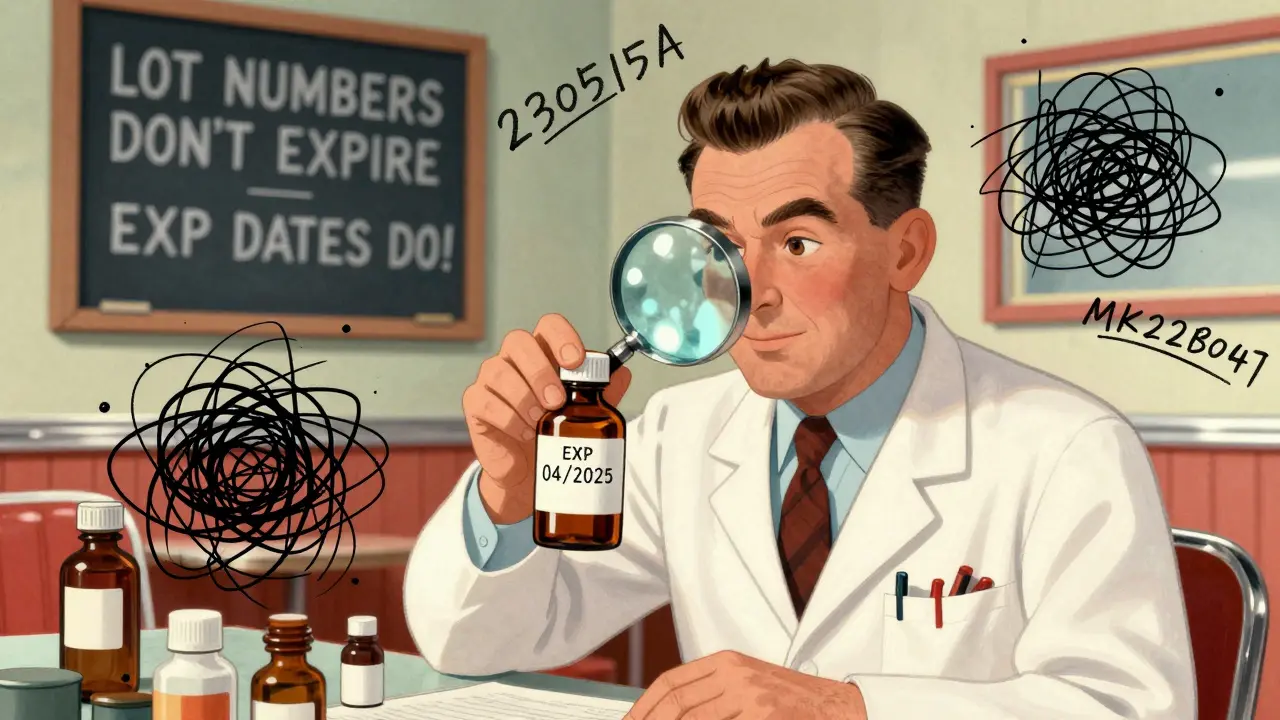
Reporting isn’t complicated. You don’t need a doctor to do it for you, though they can help. Here’s how to do it yourself:- Write down what happened. Note the date you switched, what symptoms started, how bad they were, and when they got better or worse. Include how long you’d been on the brand version before switching.
- Find the generic’s details. Check your prescription bottle. You need the manufacturer’s name and the National Drug Code (NDC)-a 10-digit number on the label. Example: “Sandoz, NDC 0781-3121-01, 10 mg tablet.”
- Identify the brand you switched from. Write the exact name (e.g., “Lipitor 20 mg”) and the manufacturer (e.g., “Pfizer”).
- Choose your reporting method. You have three options:
- Online: Go to www.accessdata.fda.gov/scripts/medwatch and fill out the MedWatch form.
- By phone: Call 1-800-FDA-1088 (1-800-332-1088). The line is open 24/7. Have your notes ready.
- By mail: Download Form FDA 3500B from the FDA website, print it, fill it out, and mail it to the address on the form.
If you’re having a medical emergency, call 911 or go to the ER. For urgent safety concerns that aren’t life-threatening, call the FDA’s emergency line: 1-866-300-4374.

What the FDA Does With Your Report
Your report goes into the FDA’s Adverse Event Reporting System (FAERS), which collects about 2 million reports a year. Most come from drug companies, but consumer reports like yours make up 20%-and they’re vital. The FDA doesn’t confirm every report as true. But they look for patterns. If 10 people report the same side effect after switching to the same generic, the FDA investigates. They might contact the manufacturer, review production records, or even issue a safety alert.Manufacturers are required to review all consumer reports and submit serious ones to the FDA within 15 days. Non-serious ones go into periodic safety reports. Your report could trigger a change in labeling, a manufacturing adjustment, or even a recall.
When to Involve Your Doctor
You don’t need a doctor to file a report. But they can help you understand if your symptoms are actually linked to the medication. If you’re on a drug with a narrow therapeutic index-like warfarin, levothyroxine, or certain seizure meds-small changes in absorption can be dangerous. Your doctor can order blood tests to check levels and confirm if the generic is behaving differently.Also, doctors often file reports too. If you tell them, they may submit one on your behalf. But don’t assume they will. Studies show only 12% of patients who experience side effects after switching to generics report them through official channels. Most just talk to their pharmacist or doctor and never file anything formal.
Why Most People Don’t Report-And Why You Should
A 2022 survey found that 42% of people who had side effects after switching to generics didn’t report them because they thought the process was “too complicated.” Others didn’t know where to start. Some blamed themselves: “Maybe it’s just stress.” Or they assumed, “It’s just a generic-it doesn’t matter.”Here’s the truth: Your report matters. The FDA doesn’t have a way to automatically track which reports come from generic switches. That’s why your details-brand name, generic name, manufacturer, date of switch-are so important. Without them, your report might get lost in the noise.
And it’s not just about you. One report might lead to a change that helps someone else avoid the same problem. A patient in 2021 reported headaches after switching to a generic version of Topamax. That report, combined with others, led the FDA to review the formulation. Within a year, one manufacturer changed its coating to reduce irritation. That change didn’t come from a lab study. It came from patient reports.
What’s Changing-And What’s Coming
The FDA is trying to make reporting easier. In 2022, they updated the MedWatch form to cut completion time by 35%. They’ve also started using AI to scan reports faster, spotting patterns 40% quicker than before. But there’s a gap: the FDA admits it doesn’t systematically track reports tied to generic switches. A 2023 government report found that current forms don’t ask the right questions to identify switch-related events.That’s changing. By Q2 2025, the FDA plans to add a new field to reporting forms: “Did you recently switch from a brand-name drug to a generic?” That will make it easier to spot trends and fix problems before they affect more people.
Final Thoughts: Your Voice Has Power
You’ve been told generics are just as good. And for most people, they are. But medicine isn’t one-size-fits-all. Your body reacts to things in ways science can’t always predict. If you notice a change after switching, document it. Talk to your doctor. And then-report it. It takes 15 minutes. It’s free. And it might save someone else from the same problem.Don’t wait for someone else to speak up. You’re the one who lived it. That’s the most important data point the FDA has.
Do I need a doctor to report side effects from a generic medication?
No, you don’t need a doctor to file a report. You can report side effects yourself using the FDA’s MedWatch website, by phone at 1-800-FDA-1088, or by mail using Form FDA 3500B. However, your doctor can help you determine if your symptoms are likely linked to the medication and may choose to file a report on your behalf with clinical details from your medical record.
What if I don’t know the manufacturer or NDC of my generic medication?
Check the prescription bottle-the manufacturer’s name and the 10-digit National Drug Code (NDC) are printed on the label. If you no longer have the bottle, call your pharmacy. They can look up the exact generic product you received, including the manufacturer and NDC. You can also check your online pharmacy account or request a printout from your pharmacist.
Can I report side effects even if I’m not sure they’re caused by the generic?
Yes. The FDA encourages reporting of any new or unexpected side effect, even if you’re unsure of the cause. The system is designed to detect patterns-not confirm individual cases. If multiple people report similar symptoms after switching to the same generic, the FDA investigates. Your report could be the first clue in identifying a larger issue.
Are authorized generics safer than regular generics?
Authorized generics are made by the brand-name company and are identical in formulation to the brand version, just sold under a different label. Studies suggest patients report fewer side effects with authorized generics compared to traditional generics, likely because the inactive ingredients are the same. If you’ve had issues with a regular generic, ask your pharmacist if an authorized generic is available for your medication.
What if my side effects are mild but annoying-should I still report them?
Yes. Mild but unexpected side effects-like persistent headaches, unusual fatigue, or skin rashes-should be reported if they weren’t listed on the drug’s label. These reports help the FDA identify previously unknown reactions. What seems minor to you could be a warning sign for others. The FDA tracks all reports, not just serious ones.
How long does it take for the FDA to respond after I report a side effect?
The FDA doesn’t respond individually to every report. Instead, they analyze reports in bulk to look for patterns. If your report is part of a growing trend, you may see a safety alert, label update, or manufacturing change months or even years later. Your report contributes to long-term safety monitoring, not immediate personal feedback.





Shawna B
I switched to a generic lisinopril last month and got a weird rash. Didn't think much of it till I read this. Now I'm gonna report it.
Robert Altmannshofer
Bro, I used to think generics were just cheap knockoffs. Then I switched to a generic for my thyroid med and started feeling like a zombie. Turned out the filler was giving me hives. Got my doc to switch me back - and filed a report. Don't sleep on the little stuff. Your body knows.
Precious Angel
Of course the FDA doesn't track this properly. Big Pharma owns them. They want you to think generics are 'just as good' so they can keep charging you $500 for the brand while the generic makers use cheap dyes that cause inflammation, anxiety, even seizures. They don't care about you. They care about profit. I've been screaming this for years and nobody listens. Now I know why.
Craig Ballantyne
While the bioequivalence parameters are statistically sound, the variability in excipient profiles across manufacturers introduces pharmacokinetic heterogeneity that may be clinically significant in narrow-therapeutic-index agents. The absence of standardized labeling for inactive ingredients in dispensing records remains a systemic gap in post-marketing surveillance.
Bethany Hosier
Thank you for this meticulously documented and profoundly necessary guide. As a former clinical pharmacist with over two decades of experience, I have witnessed firsthand the silent epidemic of unreported adverse events tied to generic substitutions. The regulatory framework is fundamentally flawed in its assumption of interchangeability. Patients are not data points - they are individuals with unique physiological responses. Reporting is not merely a civic duty; it is an act of medical sovereignty. I urge every reader to document, to persist, and to demand transparency - for your own sake, and for those who will come after you.
Kathleen Koopman
OMG YES I switched to a generic for my anxiety med and started having panic attacks 😰 I thought I was losing my mind. Then I switched back and boom - gone. I reported it last week!! 🙌
Lyn James
It's not about the drug. It's about the soul. You think your body reacts to chemicals? No. It reacts to the *meaning* of the switch - the betrayal of trust, the corporate greed disguised as cost-saving, the quiet erosion of dignity in healthcare. You don't just take a pill - you enter into a covenant with your own well-being. When that covenant is broken by a faceless corporation replacing your trusted brand with a cheap substitute, your body screams - not because of the dye, but because your spirit knows you've been deceived. And you have a right to rage. You have a right to report. You have a right to be heard.
gladys morante
I’ve been on the same generic for 5 years and never had a problem. Everyone else is just overreacting. Why can’t people just be grateful they’re not paying $200 a pill? You’re all so dramatic. It’s just a pill.
Melania Dellavega
I used to think side effects were all in my head - until I started journaling. I wrote down every symptom after switching to a generic metformin - the brain fog, the nausea, the weird metallic taste. I showed it to my doctor. We switched me back. The symptoms vanished in 48 hours. I reported it. I didn’t do it for a reward. I did it because someone else shouldn’t have to suffer the same confusion. Sometimes healing isn’t about more medicine - it’s about being believed.
Nancy M
In my village in rural Alabama, everyone uses generics. We don’t have the luxury of brand names. But when my cousin started having tremors after switching, we went to the pharmacy - asked for the NDC, wrote it down, called the FDA. No one laughed. No one said it was ‘in her head.’ We did what we had to. This isn’t just about science. It’s about dignity. And dignity doesn’t come with a price tag.