Every year, millions of people are harmed by medications that weren’t properly monitored. Not because the drugs are inherently dangerous, but because medication safety systems are fragmented, underused, or unknown. If you’re a healthcare worker, a patient, or even a caregiver, staying informed isn’t optional-it’s a lifeline. The good news? There’s a global network working to make medicines safer, and you can tap into it. Here’s how.
Follow the Major Global Players
The World Health Organization (WHO) is the backbone of global medication safety. Every year, they release updates on drug risks, new guidelines, and safety campaigns. In May 2025, WHO released a major guideline on controlled medicines like opioids and benzodiazepines, stressing that access and safety must go hand in hand. Don’t just read their reports-subscribe to their Medicines Safety email alerts. These aren’t marketing fluff; they’re direct updates from the people tracking drug risks in over 150 countries. The Uppsala Monitoring Centre (UMC), based in Sweden, runs the WHO Programme for International Drug Monitoring. They connect national reporting systems across the globe. Their work powers the annual #MedSafetyWeek, which happens every November. In 2025, it’s running from November 3-9, marking its 10th anniversary. This isn’t just a social media trend-it’s a coordinated global effort where hospitals, pharmacies, and patients are urged to report side effects. Sign up on the UMC website by August 2025 to get free campaign toolkits, posters, and digital resources to share in your workplace.Use Official Reporting Tools
Reporting a side effect isn’t just a formality-it’s data that saves lives. Less than 10% of adverse reactions are reported globally. That means for every 10 people who have a bad reaction, nine go silent. You can change that. In the UK, the Yellow Card scheme run by the MHRA lets you report reactions to medicines, vaccines, herbal products, and even e-cigarettes. Download their free app. It takes less than five minutes. You can report from your phone while waiting in line or after a doctor’s visit. The same system exists in other countries under different names: Canada’s MedEffect, Australia’s TGA, and the U.S. FDA’s MedWatch. Find your country’s system and bookmark it. Don’t wait for a serious reaction to report. Even minor issues like dizziness after a new blood pressure pill or a rash from an antibiotic matter. These reports help regulators spot patterns. In 2024, a spike in reports about a specific diabetes drug led to a label update that prevented dozens of hypoglycemia cases.Learn from the Best Practices
The Institute for Safe Medication Practices (ISMP) doesn’t just warn-they fix. Every two years, they release Targeted Medication Safety Best Practices for Community Pharmacy. The 2025-2026 edition is packed with actionable steps: double-checking weight-based dosing for kids, managing returns of unused meds, and verifying vaccine storage. These aren’t vague suggestions. They’re step-by-step checklists with worksheets you can print and use tomorrow. Pharmacists on Reddit shared real wins: one used the weight-dosing protocol to catch a 10x overdose error on a child’s antibiotic. Another cut medication return errors by 40% using the ISMP return-to-stock checklist. If you work in a pharmacy, clinic, or hospital, print these. Put them on the wall. Train your team. ISMP says early adopters cut errors by 15-22% in just six months.
Watch for Annual Campaigns and Events
Mark your calendar. There are two big moments each year you can’t miss. World Patient Safety Day is on September 17. In 2025, the focus is on newborn safety-something many overlook. WHO releases new data, toolkits, and videos. Hospitals host events. You can join virtually. Even if you’re not in pediatrics, the lessons apply: clear labeling, avoiding drug interactions, and listening to families. #MedSafetyWeek in November is the other. It’s when the global community comes together. The UMC releases new data on reporting trends, shares stories from frontline workers, and launches digital tools. In 2024, a beta version of an AI-powered symptom checker integrated with national reporting systems helped users in 15 countries report reactions faster. That tool will be fully live in 2025.Know the Tools That Work
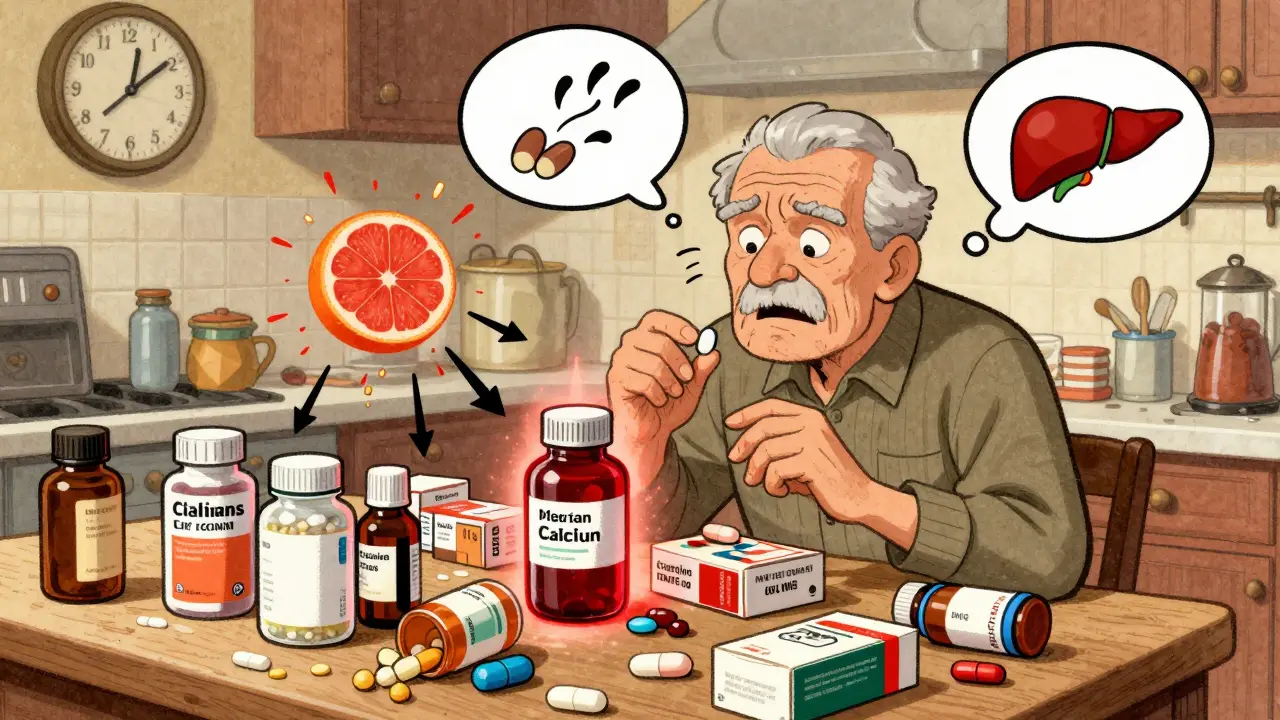
Not all safety resources are created equal. Some are flashy but useless. Others are quiet heroes. Medi-Span, a clinical decision support tool used in hospitals from Saudi Arabia to Germany, reduced medication errors by 40% in pilot sites. It’s not free, but if your workplace uses it, learn how to use its alerts. It flags dangerous interactions, outdated dosing, and duplicate prescriptions in real time. US Pharmacopeia (USP) sets global standards. Their 2025-2030 cycle is pushing for better electronic health record interoperability and standards for pharmacogenomics-testing how your genes affect drug response. These aren’t just for labs. If your doctor talks about genetic testing before prescribing, this is why. ECRI and ISMP’s Top 10 Patient Safety Issues is another must-read. The 2025 list includes AI in clinical settings, cyberattacks on health data, and social media misinformation. The last one is critical. False claims about vaccines or “miracle cures” are driving real harm. In areas with high social media use, false reports spiked adverse event claims by 18%. Learn to spot misinformation. Check WHO’s fact-checking page before sharing anything.
Bridge the Gaps in Your System
Here’s the hard truth: reporting systems don’t talk to each other. A nurse in the UK told a forum that her hospital has Yellow Card, a local incident system, and an internal app-none sync. She spends hours entering the same data three times. If you’re in charge of safety at your clinic or pharmacy, run a gap analysis. Ask: Where do reports get lost? Are staff trained? Is reporting easy or a chore? Use the ISMP worksheet. Fix one thing. Maybe it’s putting a QR code on the counter that links directly to your country’s reporting app. Maybe it’s a monthly 10-minute huddle to review a recent case. Small changes add up.What’s Coming Next
The future of medication safety is smarter-but not automatic. By 2027, tools like Medi-Span will use machine learning to predict risks before they happen. WHO aims to help 50 low-income countries build stronger reporting systems by 2030. But progress depends on you. If you’re a patient, report every odd reaction. If you’re a provider, use the tools. If you’re an administrator, invest in training. Medication safety isn’t a government job. It’s a shared responsibility. And right now, the system is only as strong as the people who use it.How do I report a side effect if I’m not a healthcare professional?
You don’t need to be a doctor to report. Most countries have public reporting systems like the UK’s Yellow Card app, Canada’s MedEffect, or the U.S. FDA’s MedWatch. Just go to your national health agency’s website, find the reporting page, and fill out the form. Include the medicine name, dose, when you took it, and what happened. Even if you’re unsure, report it. These reports help regulators spot patterns.
Why is less than 10% of side effects reported?
Many people don’t know they can report. Others think it’s not important, or that the reaction was too minor. Some assume the doctor already knows. But doctors don’t see every patient’s reaction. Pharmacists don’t always get feedback. Without reports, regulators can’t detect dangerous trends. That’s why campaigns like #MedSafetyWeek exist-to remind everyone: your report matters.
Are global medication safety systems the same everywhere?
No. High-income countries like the U.S., UK, and Germany have strong systems with hundreds of reports per million people. Low-income countries may have fewer than 10 reports per million. The WHO is working to fix this, but progress is slow. If you’re in a country with weak reporting, your report has even more impact. It helps fill a critical gap.
Can AI really help with medication safety?
Yes-but it’s not magic. AI tools like those in Medi-Span already flag dangerous drug combinations and dosing errors. Newer systems, tested in 15 countries in 2024, use AI to help patients describe symptoms and auto-fill reports. These tools reduce human error and speed up reporting. But they can’t replace human judgment. Always double-check alerts, especially for older patients or those on multiple meds.
What should I do if I see false medical information online?
Don’t share it. Report it to the platform. Then, go to WHO’s Mythbusters page or your national health agency’s fact-checking site to find the truth. Misinformation about vaccines and painkillers has led to real harm-like people avoiding needed meds or overdosing on unproven remedies. Be a source of accurate info, not a vector for risk.
How often should I check for updates on medication safety?
Set up email alerts from WHO and your national regulator. Check them monthly. For major updates-like new drug warnings or safety campaigns-mark your calendar. #MedSafetyWeek and World Patient Safety Day are key moments. If you’re in healthcare, review ISMP’s Best Practices every two years. Stay proactive. Safety isn’t something you check once-it’s something you maintain.









Cara Hritz
so i just tried to report my rash from that new blood pressure pill and the website crashed??? like wtf is wrong with these systems?? i mean i get it’s important but if the tool to report side effects is broken then we’re all just wasting time 😒
Sai Keerthan Reddy Proddatoori
they dont want you to know. the pharma giants own the WHO. why do you think they push these apps? so you think you’re helping but really you’re feeding data to the machine that controls your meds. next they’ll say your body is the problem, not the drug. #WakeUp
Candy Cotton
While I appreciate the sentiment behind this article, it is fundamentally flawed in its assumption that global regulatory frameworks are even remotely comparable in efficacy. The United States FDA maintains the most rigorous, data-driven, and transparent pharmacovigilance system on the planet. To equate it with the underfunded, under-resourced, and often non-functional systems in developing nations is not merely inaccurate-it is an affront to American scientific integrity.
Jeremy Hendriks
Medication safety isn’t about apps or alerts. It’s about power. Who gets to decide what’s dangerous? The FDA? WHO? A pharmacist in Lagos with no internet? We talk about reporting like it’s a civic duty, but the real question is: who listens? And more importantly-who benefits when you report? The system doesn’t change because we speak. It changes because someone with a budget decides to care. We’re all just shouting into a void dressed up as a database.
Aliyu Sani
bro i been workin in a pharmacy in lagos for 7 yrs and yea we got no yellow card, no medwatch, just a notebook and prayers. but i still write down every weird reaction-dizziness, rashes, even when folks say 'my head feel funny' after taking paracetamol. one day i saw 3 people with same rash from same batch of antibiotics. i called the ministry. they said 'we get 2 reports a month.' i said 'we had 12 this week.' they never called back. but i keep writin. someone gotta.
Kiranjit Kaur
OMG YES!! 🙌 I used the Yellow Card app last week after my ankle swelled up from that new joint pill-took 2 mins and I felt like a superhero 💪✨. If we all just do one tiny thing, it adds up!! Let’s make safety a team sport!! 🌍❤️ #MedSafetyWeek2025
Jim Brown
The architecture of safety is not in the tool, but in the epistemic humility of those who wield it. To report a side effect is to acknowledge the limits of our knowledge, the fragility of our physiology, and the moral weight of collective ignorance. The fact that we reduce this to a mobile app interface is not progress-it is the commodification of vigilance. We must not mistake the container for the content. The cure lies not in more data, but in deeper reverence for the body’s silent testimony.
Gabriella da Silva Mendes
Look, I get it, we’re all supposed to be little safety heroes now. But let’s be real-this whole thing feels like a distraction. The real problem? The U.S. drug pricing system is a scam, and no amount of Yellow Card reports is gonna fix that. I report my side effects, sure. But then I have to choose between my meds and my rent. So yeah, I’m ‘lazy.’ I’m not lazy-I’m exhausted. And no, I don’t care about #MedSafetyWeek when my insulin costs $500. 🙄