Every year, thousands of people in the U.S. die from accidental drug overdoses. Many of these deaths aren’t caused by reckless behavior-they happen because someone lost track of what they took, when, and how much. A simple medication log can change that. It’s not just for people on opioids. If you take any prescription, over-the-counter, or even herbal meds regularly, a log helps you avoid dangerous mix-ups, double-dosing, or mixing substances that shouldn’t be combined.
Why a Medication Log Works
Think of your medication log like a GPS for your body. It shows you where you’ve been, what you’ve taken, and where you might be heading. Without it, you’re guessing. Maybe you took your pain pill at 2 p.m. but forgot by 7 p.m. and took another. Or maybe you mixed your sleep aid with alcohol because you didn’t remember you’d already taken a benzodiazepine that morning. These aren’t rare mistakes-they’re common. The CDC says opioid overdoses often happen when people take more than prescribed, combine drugs, or use substances with unknown strength-like pills laced with fentanyl. A personal log doesn’t replace your doctor’s records, but it fills the gaps. Prescription Drug Monitoring Programs (PDMPs) track what doctors prescribe, but they don’t know if you actually took it, crushed it, or mixed it with something else. Your log does.What to Include in Your Log
A good medication log doesn’t need to be fancy. Just four key pieces of information make it powerful:- Medication name-Use the full name, not just “the blue pill.” Write “oxycodone 5 mg” or “ibuprofen 200 mg.”
- Dosage and time taken-Note the exact amount and the clock time. “Took 10 mg oxycodone at 11:30 a.m.”
- Method of use-Did you swallow it? Crush and snort it? Inject it? The way you take a drug changes how fast it hits your system and how risky it is. SAMHSA warns that injecting or smoking opioids increases overdose risk compared to swallowing.
- Other substances taken-Alcohol, benzodiazepines, sleep aids, even CBD or muscle relaxers. The CDC says combining opioids with these can be deadly. Write them all down.
Optional but helpful: note how you felt. “Dizzy after 30 mins,” “no pain relief,” “nausea.” This helps you spot patterns and tells your doctor if something’s off.
How to Start-Paper or Digital?
You don’t need an app. A notebook and pen work just fine. Many people find paper easier because it’s always there. Keep it in your wallet, purse, or next to your meds. Use a small notepad or even sticky notes stuck to your medicine cabinet. If you prefer digital, try a free notes app on your phone. Set a daily reminder to log your meds. Some apps like Medisafe or MyTherapy send alerts when it’s time to take a pill and let you log intake automatically. But don’t rely on them alone-they can glitch, die with your battery, or get lost if you switch phones. The best system is the one you’ll use every day. Pick the simplest option. Then stick with it.How to Use It to Prevent Overdose
A log isn’t just a record-it’s a tool for safety. Here’s how to use it actively:- Check before you take anything-Before you reach for a pill, look at your log. Did you already take it today? Are you mixing it with something risky?
- Follow “start low, go slow”-If you’re trying a new medication or adjusting your dose, write down every change. Don’t increase unless you’ve waited at least 24 hours and see no bad reactions. SAMHSA says this is the #1 way to avoid accidental overdose.
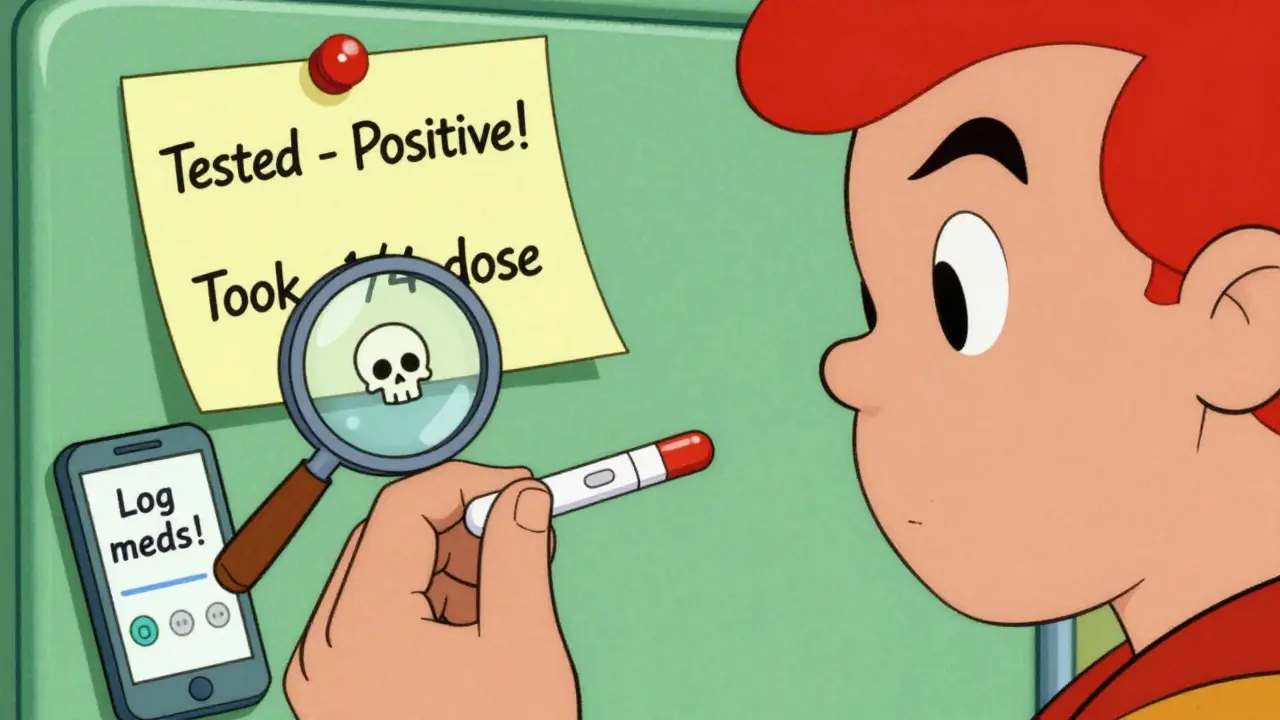
- Use drug-checking strips-If you’re using pills or powders from unknown sources, test them. Fentanyl test strips are cheap and easy to use. Write the result in your log: “Tested pill-positive for fentanyl. Took 1/4 dose only.”
- Stagger your use-If you’re using with others, make sure someone knows what you took. Share your log with a trusted friend or family member. They can help you spot if you’re taking too much.
- Review weekly-Every Sunday, look back. Did you take more than prescribed? Did you mix alcohol with painkillers? Did you feel unusually drowsy? Adjust your habits based on the data.
Common Mistakes to Avoid
Even people who log their meds mess up. Here’s what not to do:- Writing “took pain med” instead of the name and dose-Vague entries are useless. You need specifics.
- Only logging when you remember-If you skip days, the log becomes unreliable. Make it part of your routine, like brushing your teeth.
- Not recording alcohol or OTC drugs-Many overdoses happen because people forget their Tylenol or wine counts. Include everything.
- Using the log only when something goes wrong-Waiting until you feel bad means it’s too late. Use it daily, even when you’re fine.
- Sharing it with someone who judges you-Your log is for your safety, not for guilt trips. Only share with people who support you.
Who Benefits Most?
Anyone taking multiple medications can use a log-but these groups benefit the most:- People on opioids for chronic pain
- Those recovering from opioid use disorder
- Older adults taking 5+ daily medications
- People using street drugs or pills bought online
- Anyone who’s had a near-overdose or knows someone who has
It’s not just for “addicts.” It’s for anyone who wants to stay alive while managing their health.
What to Do If You Miss a Day
You’re human. You’ll forget sometimes. That’s okay. Don’t throw the log away. Just write “Missed log on [date].” Then restart the next day. The goal isn’t perfection-it’s awareness. One missed entry won’t undo your progress. Consistency over weeks and months will.
When to Show Your Log to a Doctor
Bring your log to every appointment. Not just when you’re in trouble. Show it when you’re feeling fine. Doctors rarely ask for it-but they need it. A 2022 CDC guideline says clinicians should review a patient’s full medication history before prescribing opioids. Your log gives them the real picture, not just what’s in the pharmacy system. If your doctor dismisses it, say: “I’m trying to stay safe. This log helps me avoid mistakes. Can we use it together?” Most will be glad you’re taking control.Final Thought: It’s Not About Control-It’s About Survival
A medication log isn’t about being “responsible” or “following rules.” It’s about staying alive. People who use drugs and keep logs are 30% less likely to overdose, according to harm reduction studies cited by the National Harm Reduction Coalition. That’s not magic. That’s data. You don’t need to be perfect. You just need to be consistent. Write it down. Check it before you take anything. Share it with someone who cares. That’s how you stop a mistake from becoming a tragedy.Do I need a special app to keep a medication log?
No. A simple notebook, sticky notes, or even your phone’s notes app work just fine. Apps like Medisafe can help with reminders, but they’re not required. The key is consistency-not technology.
Can a medication log help if I use street drugs?
Yes. In fact, it’s even more critical. Street drugs often contain fentanyl or xylazine, which are much stronger than expected. Logging what you took, when, and how much helps you avoid accidental overdose. Always test drugs with fentanyl strips and write the result in your log.
What if I forget to log my meds one day?
Don’t panic. Just write “Missed log on [date]” and start again the next day. One missed entry doesn’t ruin the system. What matters is that you keep going. Consistency over time saves lives.
Should I share my log with family or friends?
If you trust them, yes. Sharing your log with a safe person means they know what you’ve taken-and can help if something goes wrong. It’s part of the “never use alone” harm reduction strategy. Just make sure they won’t judge you.
Can a medication log replace a Prescription Drug Monitoring Program (PDMP)?
No. PDMPs track what doctors prescribe across pharmacies. Your log tracks what you actually took, when, and how. They work together. Your log fills in the gaps that PDMPs can’t see-like missed doses, crushed pills, or mixing with alcohol.
How often should I review my medication log?
Check it before every dose. Review it weekly to spot patterns-like taking more than prescribed or mixing substances. If you notice red flags (like increased drowsiness or missed days), talk to your doctor or a harm reduction counselor.








Jodi Harding
This is the kind of shit that actually saves lives. No fluff. Just facts. Write it down. Period.
It’s not about trust. It’s about survival.
Danny Gray
You know what’s really ironic? The same people who scream about personal responsibility when it comes to taxes or voting suddenly act like addicts are just too dumb to remember to take their pills. But hey, let’s blame the medicine, not the system that made them dependent in the first place.
Still… I guess a log beats hoping your memory doesn’t betray you when you’re high and paranoid. Weird how the most basic tools are the ones we’re too proud to use.
Zoe Brooks
I started logging my meds after my cousin almost didn’t make it. Not because I’m ‘responsible’-I’m just tired of watching people disappear because nobody kept track.
Now I use a sticky note on my mirror. Every morning, I write it down. Every night, I check it. It’s not perfect. But it’s mine. 💙
Kristin Dailey
America’s falling apart because people won’t take responsibility. This log is just a Band-Aid on a bullet wound.
Wendy Claughton
I love how something so simple can be so powerful. 📓
I use a little notebook in my purse-same one I use for grocery lists. I write: ‘Oxycodone 5mg, 10:15 a.m., with coffee, no alcohol.’
It’s not about being perfect. It’s about being alive. And honestly? It makes me feel like I’m in control of something for once. 🙏
Aysha Siera
They want you to log everything… but who’s really watching? The government? The pharmaceutical companies? They’re already tracking your prescriptions, your phone, your searches. Now they want your personal log too? Sounds like a data grab disguised as safety.
rachel bellet
The efficacy of this intervention is contingent upon adherence metrics and behavioral compliance thresholds. Non-compliance, particularly with regard to concurrent substance documentation, introduces significant confounding variables into risk stratification models. Furthermore, the absence of standardized ontological frameworks for medication entry compromises longitudinal data integrity.
TL;DR: If you don’t log it right, it’s useless.
Pat Dean
You people are pathetic. You need a notebook to remember you took a pill? You’re not sick-you’re weak. This is why America’s collapsing. No discipline. No grit. Just apps and sticky notes.
Eric Gebeke
I’ve been on opioids for 12 years. I don’t need a log. I know my body. I know my limits.
...
Okay fine. I started logging last month. I didn’t realize I was mixing alcohol with my pain meds twice a week. I’ve cut it out. This thing saved me. I’m not proud. But I’m alive.
Jake Moore
I’m a pharmacist. I’ve seen too many overdoses from people who thought they ‘remembered’ what they took.
One guy took his 10mg oxycodone at 8 a.m., forgot, took another at 1 p.m., then had a beer and a Xanax because he was ‘anxious.’ He woke up in ICU.
Your log isn’t for the doctor. It’s for the version of you that’s tired, confused, or in pain. That version doesn’t know what’s safe anymore. Your past self does.
Start today. It’s not about control. It’s about not dying alone.
Joni O
i started logging after i almost passed out from mixing my anxiety med with wine. i didn’t even realize i’d taken it that morning. now i use my phone’s notes app and set a reminder at 8am and 8pm. i still forget sometimes. but i don’t beat myself up. i just write ‘missed’ and move on. this isn’t about being perfect. it’s about being here tomorrow. 💛
Dayanara Villafuerte
Wow. Someone actually wrote something useful for once. 🙄
And yes, fentanyl strips are free at the corner pharmacy in Seattle. Go get them. Log them. Don’t be a hero. Live to regret something else tomorrow.
Tyler Myers
This is all a distraction. The real problem is the FDA allowing these drugs in the first place. They’re pushing this log nonsense so you don’t ask why your pain meds are laced with rat poison. You’re being manipulated into compliance while the real criminals profit.
Still… I log mine. Just in case.