Shoulder pain doesn’t just annoy you-it stops you from reaching for a glass on the top shelf, sleeping on your side, or even hugging your kids. Two of the most common culprits? Rotator cuff injuries and subacromial bursitis. They often show up together, and both can feel like a deep, dull ache that gets worse when you lift your arm. The good news? Most cases don’t need surgery. With the right rehab, you can get back to normal life without cutting into your shoulder.
What’s Really Going On in Your Shoulder?
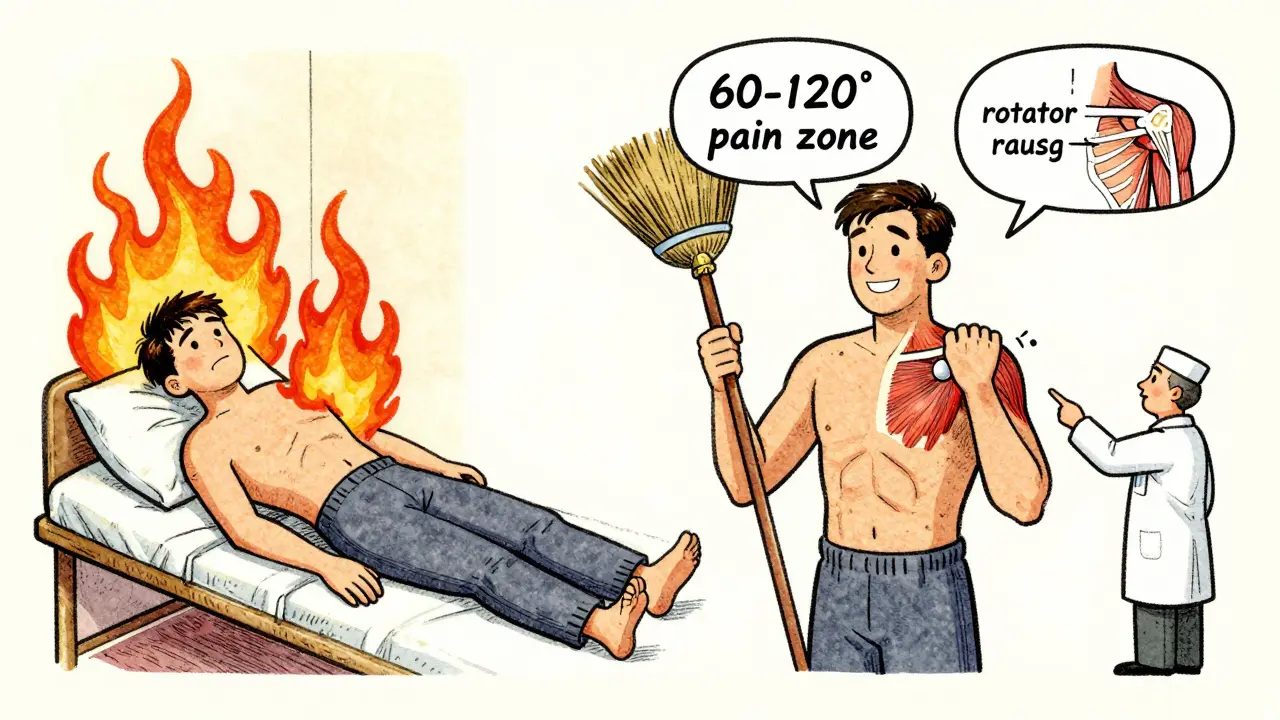
Your shoulder is a ball-and-socket joint, but unlike your hip, it’s not held together by deep bones. Instead, it’s stabilized by four small muscles-the rotator cuff-that wrap around the head of your upper arm bone. These muscles control fine movements and keep the ball centered when you lift your arm. The subacromial bursa is a tiny fluid-filled sac between the rotator cuff tendons and the bony roof of your shoulder (the acromion). It’s supposed to glide smoothly, like a cushion. When it gets inflamed, it swells up, sometimes to three or four times its normal size. That’s bursitis. Now, here’s the twist: bursitis and rotator cuff tendinitis usually happen together. When the bursa swells, it rubs against the tendons. When the tendons get irritated from overuse, they swell and press into the bursa. It’s a cycle. The classic sign? The painful arc-sharp pain when you lift your arm between 60 and 120 degrees, like reaching for a high cabinet. Night pain is another red flag. If you wake up because your shoulder feels like it’s on fire, that’s not just bad luck-it’s inflammation.Who’s Most at Risk?
You don’t have to be an athlete to get this. In fact, most people who suffer from these issues aren’t lifting weights. They’re the 55-year-old who paints houses, the 60-year-old who gardens, or the 45-year-old who finally started playing tennis again after 20 years. After age 40, your tendons naturally lose elasticity. By 50, about 1 in 5 people have some rotator cuff damage. By 80, it’s more than half. Workers who do overhead tasks-carpenters, electricians, painters-have a 32% higher chance of shoulder problems than the average person. Throwers-baseball pitchers, tennis players-have a 45% lifetime risk. Even typing with your arms elevated for hours can trigger it. It’s not about being weak. It’s about repetition, poor posture, and time.How Doctors Diagnose It
No single test confirms it. Doctors start with your story: When did it start? What makes it worse? Do you wake up at night? Then they move your arm. If you can’t lift it past 90 degrees without pain, or if you feel a click or grind, that’s a clue. They’ll check your strength-can you resist them pushing your arm down? Can you rotate your hand outward against pressure? Imaging isn’t always needed right away. But if pain lasts more than 6 weeks, or if you’re over 60 and have sudden weakness, they’ll order an ultrasound or MRI. Ultrasound can show a bursa thicker than 2 mm-normal is under 1 mm. MRI picks up tendon tears, fluid buildup, and bone spurs. A 2022 study in the Journal of Bone and Joint Surgery found that even people with full-thickness rotator cuff tears on MRI didn’t always have pain. So, the image doesn’t tell the whole story. Your symptoms do.First Steps: What to Do Right Now
If you just started hurting, here’s what works:- Stop the aggravating moves. No overhead reaching, no heavy lifting, no pushing carts or opening heavy doors with your arm extended.
- Ice it. Use a cold pack wrapped in a towel for 15 minutes, 3-4 times a day. Do this for the first 3-5 days. Cold reduces swelling and numbs the pain.
- Talk to your doctor about NSAIDs. Ibuprofen (400-600 mg) three times a day for 7-10 days can help. Don’t take it longer than that without checking in-long-term use can hurt your stomach or kidneys.
- Don’t immobilize it. Contrary to old advice, keeping your arm in a sling for days makes stiffness worse. Gentle movement is better.
Physical Therapy: The Real Game Changer
This is where most people get better. And it’s not just stretching. It’s retraining how your shoulder moves. The best rehab has three phases:- Reduce pain and swelling (Weeks 1-2): Pendulum exercises. Lean over, let your arm hang loose, and gently swing it in small circles-clockwise and counterclockwise. Do this 5-10 minutes, three times a day. It keeps the joint moving without stressing the tendons.
- Restore motion (Weeks 3-6): Use a broomstick or towel to help lift your arm. Lie on your back, hold the stick with both hands, and slowly raise it overhead. Don’t force it. Just move as far as you can without pain. Do this daily.
- Strengthen (Weeks 6-12): Start with resistance bands. Do external rotations (pulling the band away from your body at your side), scapular squeezes (pulling shoulder blades together), and wall slides (sliding your arms up a wall while keeping contact). Do 2-3 sets of 15 reps, every other day. Keep the resistance light-think 30-50% of your max. Too much too soon = setback.
When Injections Help (and When They Don’t)
If pain doesn’t improve after 4-6 weeks of rehab, your doctor might suggest a corticosteroid injection. This is a mix of a strong anti-inflammatory (like triamcinolone) and a numbing agent (lidocaine), injected under ultrasound guidance into the space under your acromion. It works for 65-75% of people. Relief usually starts in 3-7 days and lasts 4-12 weeks. But here’s the catch: it doesn’t fix the problem. It just gives you breathing room to do rehab without pain. Don’t get more than 2-3 injections a year. More than that raises your risk of tendon rupture by 8%. A 2024 FDA-approved device called AcuNav V now makes these injections 94% accurate-down from 72%-so you’re less likely to hit the wrong spot. And here’s something new: platelet-rich plasma (PRP) injections are now recommended as a second-line option after steroids fail. A 2024 trial showed PRP had a 68% success rate for long-term relief, compared to 52% for repeat steroid shots. It’s not magic, but it’s promising for people who want to avoid surgery.Surgery: The Last Resort
Only 20% of people ever need it. Surgery is usually reserved for:- Complete rotator cuff tears that don’t improve after 3-6 months of rehab
- Severe bone spurs pinching the tendon
- Young, active people with trauma-related tears

What Not to Do
Don’t be a weekend warrior. You spend Monday to Friday sitting at a desk, then on Saturday you play 9 holes of golf or lift heavy boxes. That’s a recipe for flare-ups. 35% of repeat visits are from people who return to activity too soon. Don’t ignore pain during rehab. Use a 0-10 scale. If your pain goes above a 5 during exercise, back off. Pushing through sharp pain can make things worse. Dull ache? That’s okay. Shooting pain? Stop. Don’t skip the home exercises. A 2023 study found patients who used a phone app to remind them to do their exercises completed 82% of their routines. Those without reminders? Only 54%. That 28% gap meant faster recovery for app users.Real Stories, Real Results
A 54-year-old carpenter from Minnesota had bursitis so bad he couldn’t hold a hammer. He did 14 weeks of physical therapy-daily pendulum swings, scapular squeezes, and band rotations. He’s back on the job, no surgery. A 37-year-old college tennis player had tendinitis after a bad serve. She did daily cryotherapy (ice massage) and eccentric strengthening (slowly lowering a weight). She was back on the court in 10 weeks. A 68-year-old retired teacher with a full-thickness tear chose not to have surgery. After 6 months of rehab, her pain dropped from 8/10 to 2/10. She can now reach for her coffee mug without wincing.What’s Changing in 2026
Rehab is getting smarter. Wearable sensors are now being tested to give real-time feedback on your form during exercises. If your shoulder blade doesn’t move right during a wall slide, the device buzzes. Companies are racing to get FDA clearance for these tools. For older adults, blood flow restriction training-using a cuff to lightly restrict blood flow while doing light resistance-is showing a 30% faster recovery in people over 60. It’s safe, low-impact, and doesn’t require heavy weights. Medicare now pays 4.7% more for supervised physical therapy and 2.3% less for steroid injections. That’s pushing clinics to get patients into rehab sooner.How to Stay Pain-Free
Even after you feel better, don’t stop. Keep doing your scapular squeezes twice a week. Stretch your chest and shoulders daily. Avoid carrying heavy bags on one shoulder. Sit with your arms supported when you’re at a computer. And if you feel that familiar ache coming back? Don’t wait. Go back to your pendulum exercises. Early action stops flare-ups from becoming injuries. Your shoulder doesn’t need to be perfect. It just needs to move without pain. And with the right rehab, it can.How long does shoulder bursitis take to heal?
Most people see improvement in 4-6 weeks with consistent rehab. Full recovery usually takes 8-12 weeks. If you’re over 60 or have a full-thickness tear, it may take 4-6 months. The key is sticking to your exercises-even when it feels better.
Can I still work out with shoulder bursitis?
Yes-but not the way you used to. Avoid overhead presses, bench presses, and heavy rows. Stick to low-impact cardio like walking or cycling. Do your rehab exercises daily. Once pain drops below a 3/10, you can slowly add back light resistance. Never push into sharp pain.
Is heat or ice better for shoulder pain?
Use ice for the first 3-5 days to reduce swelling. After that, heat can help loosen stiff muscles before stretching. But if your shoulder feels hot, swollen, or inflamed, stick with ice. Heat can make inflammation worse.
Do I need an MRI for shoulder pain?
Not always. If your pain is mild and improves with rest and rehab, an MRI isn’t needed. But if you’ve had pain for more than 6 weeks, are over 60, or have sudden weakness, an MRI or ultrasound helps rule out a tear or other structural damage.
Can shoulder bursitis come back?
Yes, in 15-20% of cases, especially if you return to the same activities without fixing your posture or movement patterns. That’s why maintenance exercises matter. Do scapular squeezes and shoulder mobility drills 2-3 times a week, even after you’re pain-free.
What’s the difference between a rotator cuff tear and bursitis?
Bursitis is inflammation of the fluid sac. A rotator cuff tear is a rip in the tendon itself. Bursitis hurts when you lift your arm. A tear often causes weakness-you might not be able to lift your arm at all, even if it doesn’t hurt. An MRI can tell the difference.







TONY ADAMS
Man, I thought my shoulder was just old, turns out I was just dumb. Did the pendulum thing for a week and now I can reach my damn top shelf again. No surgery, no BS.
Ashley Karanja
This is one of the most clinically nuanced yet accessible breakdowns I’ve read on shoulder pathology. The emphasis on scapular kinematics over isolated rotator cuff strengthening is backed by robust biomechanical literature-particularly the 2023 MSPT study cited. The neuromuscular re-education component is underappreciated in primary care. Also, the data on PRP vs. corticosteroids aligns with recent meta-analyses in AJSM. Kudos to the author for highlighting functional outcomes over imaging artifacts. This is how evidence-based rehab should be communicated.
Karen Droege
OH MY GOD I’M CRYING. I was this 54-year-old carpenter. I couldn’t lift my coffee cup. I thought I was done. I did the scapular squeezes while watching Netflix. I did the band rotations while waiting for my damn tea to brew. And now? I’m building a deck. I’m hugging my grandkids. I’m not just pain-free-I’m alive again. Thank you for writing this. I’m printing it and taping it to my toolbox.
Geoff Miskinis
Typical American overmedicalization. You don’t need a 12-week rehab protocol to fix a tendon issue-you need discipline. I’ve been lifting since I was 14. I didn’t need ultrasound-guided injections or PRP. I just stopped being lazy. Also, why are we paying Medicare to incentivize PT over surgery? That’s socialist nonsense disguised as healthcare reform.
shivam utkresth
From India, I’ve seen this exact thing with our construction workers. They never rest. They think pain is normal. I told my uncle to do the pendulum exercise while sitting on his charpai. He did it for 10 minutes before chai every day. Two months later, he was painting walls again. No doctor. No MRI. Just consistency. This post nails it.
Henry Jenkins
Interesting how the article downplays the role of posture in desk workers. I’ve been a software engineer for 18 years, and I’ve seen 12 coworkers with this exact pain. None of them had overhead labor. But all of them had forward head posture, rounded shoulders, and spent 8+ hours with arms elevated typing or using a trackpad. The real culprit isn’t just aging or repetition-it’s the modern workstation. We need ergonomic interventions before rehab. I’d love to see a follow-up on workstation redesign as primary prevention. Also, why is there no mention of thoracic spine mobility? If your mid-back is stiff, your shoulder has no choice but to compensate. That’s biomechanics 101.
George Rahn
Let me be blunt: Western medicine has turned a simple physiological response into a billion-dollar industry. We’ve replaced discipline with devices, wisdom with wearables, and resilience with rehab schedules. The rotator cuff isn’t a fragile toy-it’s a product of evolution. We’ve been engineered to move, not to be coddled. The fact that a 68-year-old retired teacher healed without surgery isn’t a miracle-it’s proof that the body knows how to heal if you stop interfering with gimmicks. PRP? Cortisone? Please. The real treatment is patience, cold showers, and not whining about pain. This isn’t medicine. It’s therapy for the weak.
Aurelie L.
I had this. Stopped. Did nothing. It went away. Don’t make it a thing.
Ashley Porter
Just read the 2022 JBJS study again-turns out 40% of asymptomatic people over 60 have full-thickness tears on MRI. So if your MRI shows a tear but you don’t have pain… you’re fine. The real diagnosis is your symptoms, not your scan. This is why I hate overtesting. The image is just a photo. The pain is the story.
SWAPNIL SIDAM
Bro, I’m 28, work in a call center, and my shoulder started hurting after I started holding the phone between my ear and shoulder. I did the towel stretch for 3 weeks. Now I don’t even think about it. No meds. No PT. Just moved better. Thanks for this.
Rakesh Kakkad
As a physician practicing in rural India, I have observed that the majority of patients with shoulder pain present only after chronic disability has set in. The emphasis on early, consistent, low-intensity rehabilitation as outlined here is not merely clinically sound-it is culturally transformative. In our context, where access to imaging and surgical care is limited, this protocol represents not just an alternative, but a lifeline. The inclusion of pendulum exercises and scapular retraction as foundational interventions aligns with the principles of low-resource, high-impact care. This article is a model for global health dissemination. I will distribute it to every community health worker in my district.