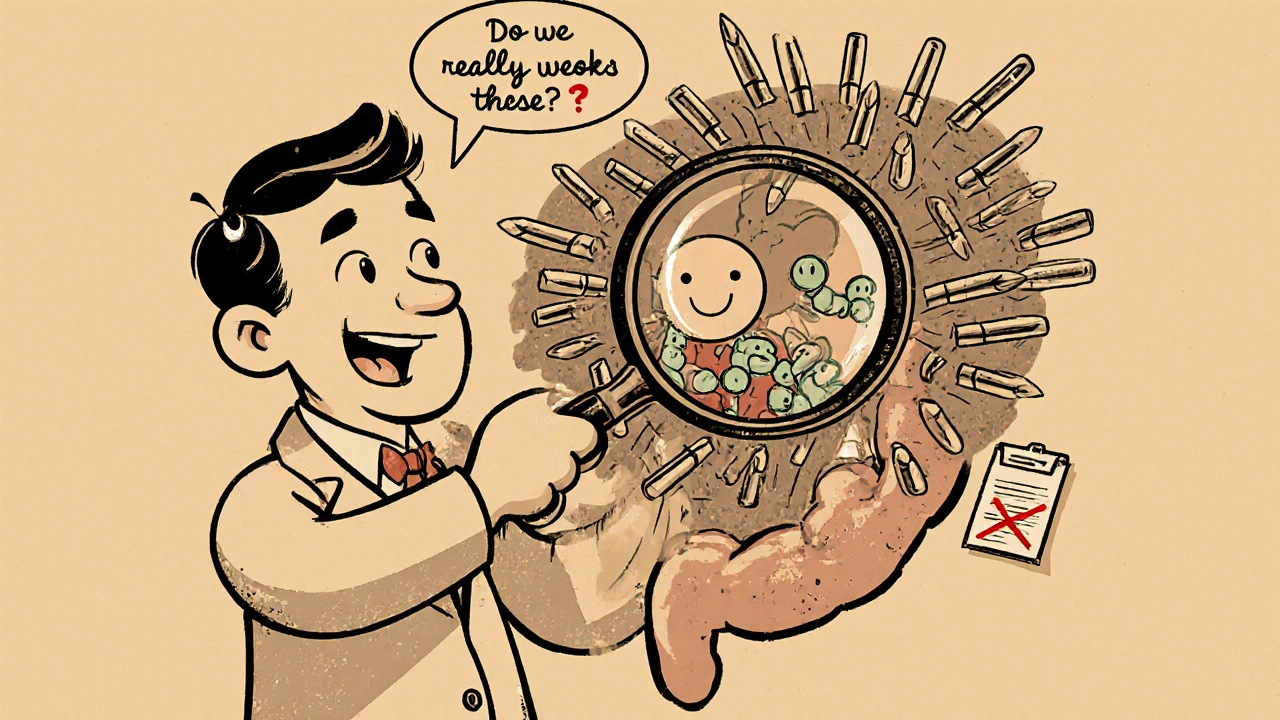
Appropriate Antibiotic Use: Stop Misuse, Save Lives
When you take an antibiotic, a medicine designed to kill or slow the growth of bacteria. Also known as antibacterial agents, they’re lifesavers—when used correctly. But every time you take one for a cold, skip a dose, or save leftovers for next time, you help create drug-resistant bacteria that no medicine can touch. This isn’t science fiction. The CDC says more than 2.8 million antibiotic-resistant infections happen in the U.S. every year, and over 35,000 people die from them. That’s not just a statistic—it’s your neighbor, your parent, your kid.
Antibiotic resistance, the ability of bacteria to survive and multiply despite antibiotic treatment doesn’t happen because your body gets used to the drug. It happens because the bacteria do. When you don’t finish a full course, the strongest bugs survive and pass on their defenses. And when you take antibiotics for viral infections like the flu or most sore throats, you’re not helping—you’re just feeding the problem. Even antibiotic storage, how you keep liquid antibiotics like amoxicillin or Zithromax at home matters. If you don’t refrigerate them when needed, or leave them in a hot car, they lose strength. That means the bacteria you’re trying to kill might not get enough to die, and again—they learn to fight back.
It’s not just about taking them right. It’s about not taking them at all when they won’t work. Most coughs, colds, and ear infections are viral. Antibiotics won’t touch them. Yet doctors still get pressured to prescribe them. And patients still expect them. That cycle keeps the problem alive. But you can break it. Ask your doctor: "Is this really a bacterial infection?" "What happens if I don’t take this?" "Are there other ways to feel better?" You’re not being difficult—you’re being smart.
And don’t forget the side effects. Antibiotics don’t just kill bad bacteria—they wipe out the good ones in your gut. That’s why diarrhea, yeast infections, and even long-term digestive issues show up after a course. Some, like metronidazole, can even cause nerve damage if used too long. That’s why antibiotic overuse, the unnecessary or excessive use of antibiotics isn’t just a public health issue—it’s a personal risk.
The posts here aren’t just about how to take antibiotics. They’re about how to think about them. You’ll find guides on storing liquid antibiotics for kids so they stay effective, what to do if you miss a dose, how certain drugs like rifampin can make antibiotics useless by interfering with their metabolism, and why using them for non-bacterial conditions does more harm than good. You’ll see real examples of what works, what doesn’t, and what’s often misunderstood.
You don’t need to be a doctor to use antibiotics responsibly. You just need to know the facts. And what you’re about to read will give you exactly that—no fluff, no fearmongering, just clear, practical info that helps you protect yourself, your family, and the next generation from the growing threat of untreatable infections.
Antibiotic Stewardship: How Using Antibiotics Right Reduces Side Effects
Antibiotic stewardship reduces harmful side effects by ensuring antibiotics are only used when needed, at the right dose and duration. Learn how proper use prevents C. diff, protects your microbiome, and saves lives.