If you open your pill bottle and the pills don’t look right - different color, shape, size, or just plain unfamiliar - stop. Don’t take it. Don’t guess. Don’t wait to see what happens. A pharmacy error isn’t just a mistake; it’s a potential emergency.
Every year in the U.S., over 1.5 million people get the wrong medication from their pharmacy. Some of these errors are caught before they cause harm. Others lead to hospital visits, long-term damage, or worse. The good news? You have power. You have rights. And you have clear steps to take right now.
Stop Taking the Medication Immediately
The first thing you do - the only thing that matters right now - is to stop taking the pills. Even if you feel fine. Even if the label says it’s for your condition. If it doesn’t match what you expected, it’s not safe.
Pharmacies fill hundreds of prescriptions a day. Mix-ups happen. A pill that looks like your blood pressure medicine might actually be a diabetes drug. Or worse - it could be a powerful opioid meant for someone else. Taking the wrong drug can trigger dangerous reactions: dizziness, rapid heartbeat, seizures, organ damage. Some medications interact badly with others you’re already taking. You don’t need to wait for symptoms to appear. If it’s wrong, it’s a risk.
Contact Your Doctor Right Away
Call your prescribing doctor as soon as you realize the mistake. Don’t wait. Don’t text. Call. Explain exactly what happened: “I got pills that don’t match my prescription. Here’s what they look like.”
Your doctor needs to know because:
- They may need to adjust your treatment plan immediately.
- They might order blood tests to check for side effects.
- They could tell you to go to the ER if the medication is dangerous.
Some medications - like insulin, blood thinners, or seizure drugs - can cause irreversible harm within hours. Your doctor is your first line of defense. They’ll tell you whether you need urgent care or can wait for a follow-up.
Call the Pharmacy - Ask for the Manager
Don’t just complain to the cashier. Ask to speak with the head pharmacist or pharmacy manager. This isn’t about blaming someone - it’s about fixing the problem and protecting others.
When you call, say clearly: “I received the wrong medication. I need to speak with the person responsible for filling this prescription.”
Ask for:
- A written explanation of what went wrong.
- Confirmation that the error has been logged in their system.
- A replacement with the correct medication, free of charge.
Pharmacies are required by law to investigate every dispensing error. But they won’t take it seriously unless you escalate it. If they refuse to talk to a manager, hang up and call again. Or go in person.
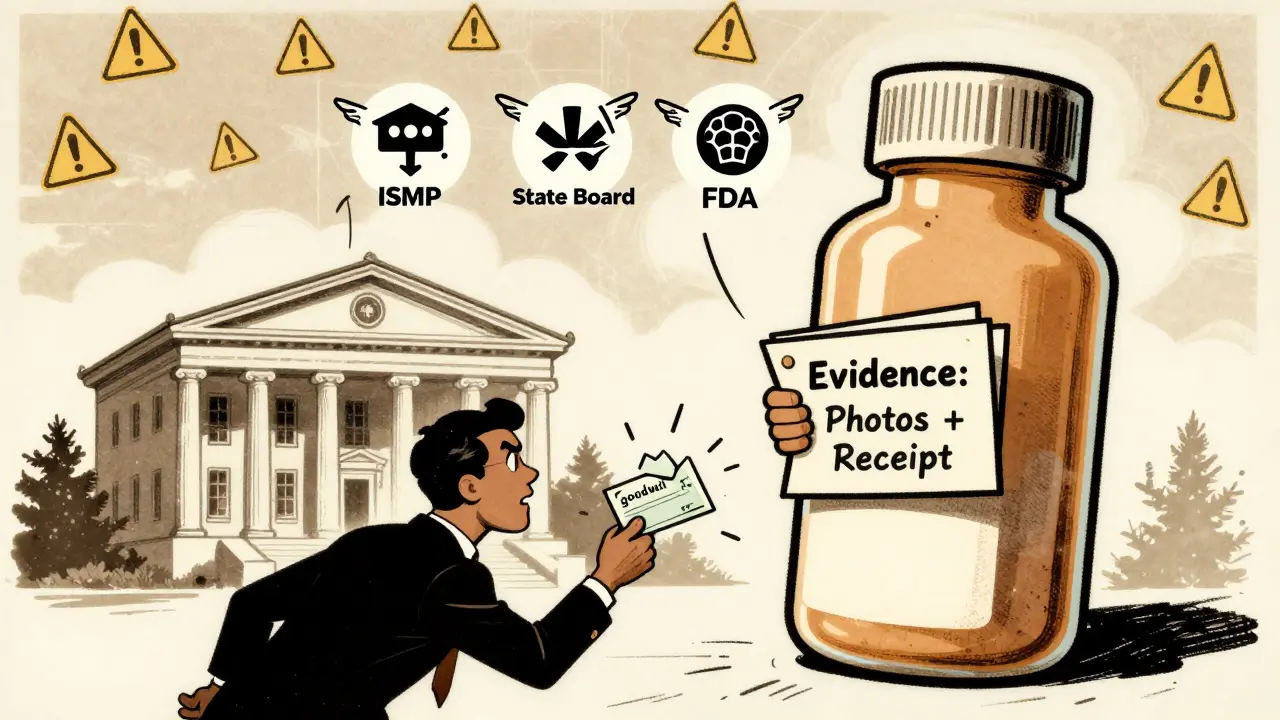
Save Everything - Don’t Throw Anything Away
This is critical. Every single item related to the error must be kept. That includes:
- The incorrect pills - in the original bottle.
- The empty bottle - even if it’s empty.
- The prescription label - the one the pharmacy put on the bottle.
- The receipt - with the date, time, and pharmacy name.
- The original prescription from your doctor - if you have a copy.
Do NOT return the wrong medication to the pharmacy. Do NOT flush it. Do NOT give it to someone else. This is evidence. If you need to take legal action later - and many people do - this is what proves the error happened.
Take clear photos of the pills, the label, and the receipt. If you can, record a short video showing the pills next to the label. Studies show that cases with photographic or video evidence are 37% more likely to result in a higher settlement.

Report the Error - To the Right Places
Pharmacies don’t fix problems unless they’re forced to. Reporting the error helps prevent it from happening to someone else.
Use these three reporting channels:
- The Institute for Safe Medication Practices (ISMP) - They run a confidential national reporting system. You can report online at ismp.org. They’ve collected over 100,000 reports since 1991. Your identity stays private.
- Your state’s pharmacy board - Every state has one. In Georgia, you report to the Georgia Composite Medical Board. In Washington, it’s the Washington State Department of Health. Search “[Your State] pharmacy board complaint.”
- The FDA’s MedWatch program - File a report at fda.gov/medwatch. The FDA received over 92,000 medication error reports in 2022, and 38% came from community pharmacies.
Don’t assume someone else will report it. If you don’t, the error might happen again tomorrow.
Know Your Legal Rights
A pharmacy error isn’t just a bad day - it can be medical negligence. If you were harmed, you may be entitled to compensation.
Here’s what you need to know:
- You have 1 to 3 years to file a claim, depending on your state. In Georgia, it’s 2 years from the date you discovered the error.
- Most cases settle out of court - about 70% - with payouts ranging from $50,000 to $500,000.
- Catastrophic injuries (permanent disability, organ damage, death) have led to verdicts over $10 million.
Do not give a recorded statement to the pharmacy’s insurance company. Do not sign anything they give you. Do not accept a “goodwill” payment without talking to a lawyer first. These offers are often far below what you’re owed.
Consult a medical malpractice attorney who specializes in pharmacy errors. Many work on contingency - you pay nothing unless they win.
What Causes These Errors?
It’s not just “human error.” The system is broken in ways most people don’t realize.
Common causes include:
- Similar-looking or sounding drug names (e.g., Celebrex vs. Celexa).
- Handwritten prescriptions that are hard to read.
- High workload - pharmacists filling 200+ prescriptions a day.
- Lack of double-checks for high-risk medications.
- Outdated systems - only 62% of U.S. pharmacies use barcode scanning, which cuts errors by 85%.
The Veterans Health Administration cut medication errors by 55% between 2018 and 2022 by fixing the system - not blaming staff. That’s the model. But most pharmacies still rely on tired, overworked pharmacists to catch mistakes no human can catch consistently.
How to Prevent This in the Future
You can’t control the pharmacy - but you can control what you do when you pick up your prescription.
Always:
- Check the label against your doctor’s prescription before leaving the pharmacy.
- Ask the pharmacist: “Is this what my doctor ordered?”
- Compare the pills to your last fill - color, shape, markings.
- Use one pharmacy for all your prescriptions - it helps them track your history and catch conflicts.
- Ask for a printed copy of your prescription from your doctor - keep it in your wallet.
If you’re on high-risk medications - blood thinners, insulin, seizure drugs - ask for a double-check. Most pharmacies will do it if you ask.
Long-Term Risks of Ignoring a Pharmacy Error
Some people think, “I didn’t feel sick, so it’s fine.” That’s dangerous.
Studies show patients who experience a medication error have a 28% higher risk of dying within five years. For those who took the wrong heart or blood pressure medication, the risk jumps to 42%.
Why? Because the wrong drug can cause hidden damage - kidney stress, liver overload, irregular heart rhythms - that doesn’t show up until it’s too late.
And the cost to the system? Preventable pharmacy errors cost the U.S. healthcare system $8.4 billion a year. That’s not just money - it’s lives.
Real Cases - What Happens When People Act
A woman in Atlanta noticed her diabetes pills were blue instead of white. She called her doctor, who ordered a blood test. Her blood sugar had spiked dangerously. She saved her own life.
A man in Ohio took someone else’s ADHD medication for three days. He had panic attacks, chest pain, and couldn’t sleep. He reported the error, got a settlement, and pushed his pharmacy to install barcode scanners.
A child in Texas was given a cancer drug meant for an adult. She had a seizure and spent three days in the hospital. Her parents sued. They won $75,000 - not because they wanted money, but because they wanted to make sure no other child got that pill again.
You are not alone. And you are not powerless.







Monte Pareek
Look I've worked in retail pharmacy for 12 years and let me tell you this is the single most important thing people dont do
Check the pills before you leave the counter
Not after you get home not after you open the bottle but right there when the pharmacist hands it to you
Pharmacists are overworked yes but theyre not mind readers
If you dont compare the pill to your last script the system fails
And dont just glance at the label look at the shape color markings everything
Ive seen people take wrong meds because they trusted the label
Labels get misprinted pills get swapped in the bin
Its not about blaming the pharmacy its about being your own safety net
And if youre on insulin or blood thinners ask for a double check
Most places will do it if you ask
Its not a hassle its a lifesaver
And dont forget to use one pharmacy always
It builds a history and catches interactions
Simple habits prevent disasters
Connie Zehner
OMG I CANT BELIEVE THIS HAPPENED TO ME LAST YEAR 😭
I TOOK SOMEONE ELSE'S OPIOID FOR 3 DAYS AND THOUGHT I WAS HAVING A PANIC ATTACK BUT IT WAS JUST THE DRUG 😵💫
MY DOCTOR SAID I COULD HAVE DIED AND NOW I CRY EVERY TIME I SEE A PHARMACY
PLS LIKE AND SUBSCRIBE TO MY SAFETY CHANNEL
Dev Sawner
The premise of this article is fundamentally flawed. The notion that individual vigilance can mitigate systemic failures is a neoliberal fantasy. The real issue lies in the commodification of healthcare where pharmacists are incentivized to maximize throughput over safety. The 200 prescriptions per day metric is not anecdotal-it is structural. The solution is not to ask patients to become amateur pharmacists but to demand universal regulatory reform: mandatory barcode scanning in all pharmacies, reduced workload caps, and independent oversight bodies with punitive authority. Until then, we are merely rearranging deck chairs on the Titanic.
Sahil jassy
Bro this is gold
Always check your pills
One pharmacy only
Ask for double check if you on heavy meds
Save everything
Thats all you need
Kelly Mulder
While the article's practical advice is commendable, it exhibits a disturbingly reductive epistemology. The invocation of 'photographic evidence' as a determinant of legal outcome suggests a dangerous conflation of performative documentation with substantive justice. Furthermore, the normalization of contingency-based legal representation implicitly endorses the commodification of bodily integrity. One cannot help but observe the rhetorical sleight-of-hand that positions the patient as both victim and proactive agent-thereby absolving the institutional architecture of culpability. The true tragedy is not the error, but the normalization of its inevitability.
Kitt Eliz
YAS QUEEN 💪🔥
This is the exact kind of empowerment we need in healthcare
YOU GOT THIS
Be your own advocate 🙌
Pharmacy errors are NOT your fault but your awareness is your superpower 🦸♀️
Save the pills take pics report it push back
You are not broken you are bold
And if you need a hype squad I got you
Tag me when you file your report I’ll send you confetti 🎉
anthony funes gomez
When we speak of medication error, we are not merely discussing a procedural lapse-we are confronting the ontological rupture between the body as a site of biological function and the body as a node within a mechanized, profit-driven logistics network. The pill, once a symbol of healing, has become a token in a distribution algorithm that privileges efficiency over embodiment. The pharmacist, once a guardian of pharmacopeia, is now a node in a chain of optimization. The patient, therefore, is not merely a recipient but a reluctant failsafe. To demand that the patient become the final arbiter of safety is not empowerment-it is the abdication of institutional responsibility onto the vulnerable. The system does not need more vigilance-it needs dismantling.
Marsha Jentzsch
Wow, you’re so lucky you even HAVE a doctor to call and a pharmacy that didn’t just give you a free sample of someone else’s antidepressant and tell you to 'be more careful next time.'
My cousin got the wrong meds and the pharmacy said 'it’s close enough' and she ended up in the ER for a week and they refused to even apologize.
People like you just don’t understand what it’s like when the system is actively working against you.
And now you’re just giving advice like it’s all on you to fix it? That’s so toxic.
Kathryn Featherstone
I appreciate the detailed steps here. I’ve worked in a community pharmacy and I can say that most of us truly want to get it right. But the pressure is insane. If you’re ever in the store and you see someone double-checking their meds, thank them. It makes our job safer too. We’re not robots. We need your help to catch what we miss. Small acts of collaboration matter more than you know.