Many people think if a drug makes them feel sick, they’re allergic to it. That’s not always true-and confusing the two can actually put your health at risk. You might avoid a life-saving antibiotic because you think you’re allergic to penicillin, when in reality, you just had nausea or a headache. Or worse, you might keep taking a drug that’s slowly damaging your liver, thinking it’s "just a side effect." Understanding the difference between side effects and allergic reactions isn’t just academic-it’s critical for your safety, your treatment options, and your wallet.
What Are Medication Side Effects?
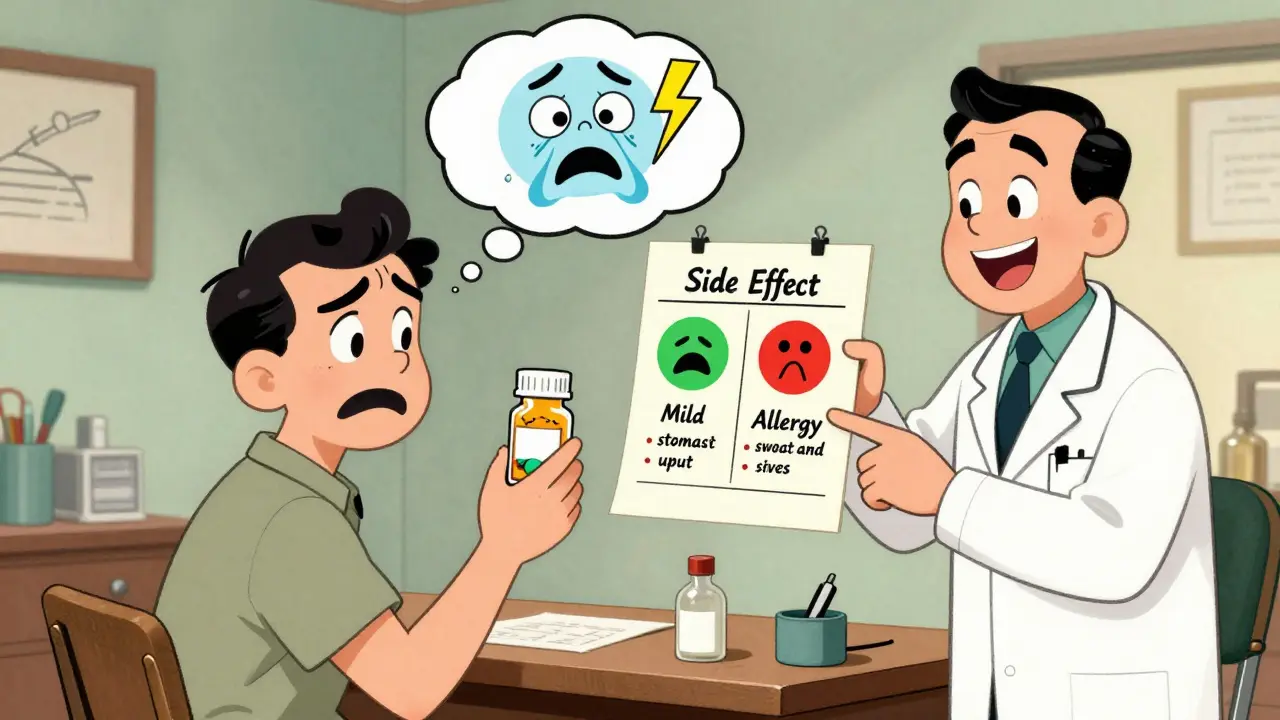
Side effects are predictable, known reactions that happen because of how a drug works in your body. They’re not your immune system going haywire-they’re just the drug doing something it wasn’t meant to do, but still within its normal range of action. Think of it like a car that’s designed to go 60 mph but sometimes shakes a little at 55. It’s not broken; it’s just not perfect.The FDA requires drug makers to list side effects in the prescribing information, along with how often they occur. For example, statins-used to lower cholesterol-cause muscle aches in about 5 to 10% of users. Metformin, a common diabetes drug, gives 20 to 30% of people stomach upset. These numbers aren’t guesses; they come from clinical trials and real-world monitoring systems like the FDA’s Adverse Event Reporting System.
Side effects usually show up within hours or days of starting the drug. They’re often mild and go away on their own as your body adjusts. In fact, 70 to 80% of common side effects fade within two to four weeks. That’s why doctors often tell you to give a new medication a few weeks before deciding if it’s right for you.
Some side effects can be managed. Taking metformin with food cuts GI issues in 60% of people. Drinking plenty of water while on NSAIDs like ibuprofen helps protect your kidneys. Sometimes, lowering the dose helps. You don’t have to quit the drug-you just tweak how you use it.
What Is a True Drug Allergy?
A drug allergy is different. It’s your immune system mistaking the medication for a dangerous invader-like a virus or bacteria-and launching a full attack. This isn’t about how the drug works. It’s about your body’s overreaction to it. And once your immune system decides a drug is a threat, it remembers. Next time you take it-even years later-it reacts again.True allergies are rare. Only about 5 to 10% of all reported bad reactions to drugs are actual allergies. But they’re serious. The most dangerous type is anaphylaxis-a sudden, life-threatening reaction that can cause swelling of the throat, trouble breathing, a drop in blood pressure, and loss of consciousness. It usually happens within minutes to two hours after taking the drug.
Other allergic reactions include hives, itching, rash, fever, and swelling of the face or tongue. Delayed reactions, like a widespread rash that shows up a week after starting a drug, are often T-cell mediated and still count as allergies. These can be mistaken for a virus or skin infection, but they’re immune-driven.
Penicillin is the most common trigger, accounting for 80% of severe drug allergies. Sulfonamides, NSAIDs like aspirin and ibuprofen, and certain seizure meds also top the list. But here’s the kicker: if you say you’re allergic to penicillin, there’s an 80 to 90% chance you’re wrong. Studies show most people who report a penicillin allergy don’t test positive when properly evaluated.
Key Differences at a Glance
| Feature | Side Effect | Allergic Reaction |
|---|---|---|
| Immune System Involved? | No | Yes |
| How It Happens | Drug’s normal pharmacological action | Immune system overreacts to drug as foreign |
| Timing | Hours to days after starting; often improves over time | Minutes to 2 hours (immediate) or days to weeks (delayed) |
| Dose-Dependent? | Usually yes-higher dose = worse effect | No-even tiny amounts can trigger it |
| Can It Be Managed? | Yes-dose change, timing, other meds | No-must avoid completely |
| Common Examples | Statin muscle pain, metformin nausea, lisinopril cough | Penicillin hives, anaphylaxis, sulfonamide rash |
| Testing Available? | No-diagnosed by pattern and timing | Yes-skin tests, blood tests (IgE, BAT) |
Why Mislabeling Matters
When you call a side effect an allergy, you’re not just being inaccurate-you’re limiting your care. If you’re labeled as allergic to penicillin, doctors can’t use it, even though it’s often the safest, cheapest, and most effective antibiotic. Instead, they reach for broader-spectrum drugs like vancomycin or fluoroquinolones. These drugs are more expensive, more likely to cause side effects, and increase your risk of deadly infections like MRSA.A 2021 JAMA Internal Medicine study found that people mislabeled as penicillin-allergic had a 69% higher chance of developing MRSA. Each mislabeled allergy adds about $4,000 in extra healthcare costs per person annually. That’s not just a number-it’s more hospital stays, longer recovery times, and unnecessary risks.
And it’s not just penicillin. People often say they’re allergic to ibuprofen because it gave them a headache, or to statins because they felt tired. Those aren’t allergies. They’re side effects. But once they’re written into your chart, they stick. Many patients never get retested, even decades later.
How Do You Know Which One You Had?
The key is timing and symptoms. Ask yourself:- When did the reaction happen? If it was within 15 minutes of taking the drug and included swelling, trouble breathing, or hives-it’s likely an allergy.
- Did you have a rash, fever, or blistering skin 7 to 14 days after starting the drug? That’s a delayed allergic reaction.
- Was it nausea, dizziness, or a headache that started after a few days and got better with time? That’s probably a side effect.
- Did the reaction happen only once, or every time you took the drug? Allergies repeat. Side effects might not.
Doctors use tools like the PEN-FAST rule to quickly screen for low-risk penicillin allergies. If you’ve never had swelling, breathing trouble, or anaphylaxis, and it’s been more than 10 years since the reaction, you might be cleared without testing. But if there’s any doubt, skin testing or a supervised oral challenge is the gold standard. Skin tests for penicillin are 97% accurate at ruling out true allergies.
What Happens If You’re Wrong?
If you’ve been told you’re allergic to a drug but never got tested, you’re likely avoiding something you could safely take. A 2022 study in the Annals of Internal Medicine found that 40% of people who thought they had drug allergies had their treatment limited because of it-meaning they missed out on better, safer options.On the flip side, if you ignore a real allergy and take the drug again, you could end up in the ER-or worse. Anaphylaxis kills 0.3 to 1% of people who experience it, even with treatment. That’s why it’s better to be cautious and get tested.
Some people do get desensitized-gradually exposed to small doses of the drug under medical supervision. It works about 70 to 80% of the time, but only for essential drugs like antibiotics or chemotherapy. It’s not a cure. It’s a temporary workaround.
What’s New in Testing?
Testing has gotten better. In 2023, the FDA approved a new blood test called the basophil activation test (BAT) for penicillin allergy. It’s more accurate than skin tests alone, especially for people with skin conditions that make skin testing hard. It detects immune cells that react to the drug, giving results with 85% sensitivity and 95% specificity.Genetic testing is also emerging. For example, if you’re prescribed abacavir (an HIV drug), doctors now check for the HLA-B*57:01 gene. People with this gene have an 8% risk of a life-threatening reaction. If you don’t have the gene, the risk drops to 0.4%. This isn’t science fiction-it’s standard care now.
What Should You Do?
If you think you have a drug allergy:- Don’t assume. Write down exactly what happened: symptoms, timing, dose, how long it lasted.
- Ask your doctor if it was likely an allergy or a side effect.
- Request a referral to an allergist if you’ve been labeled allergic to penicillin, sulfa, or NSAIDs.
- Get tested. Even if it’s been years, the results can change your care forever.
- Update your medical records. If you’re cleared, make sure your chart says "not allergic"-not "allergy suspected" or "history of reaction."
If you’ve been told you have a side effect, but it’s unbearable, talk to your doctor about alternatives, dose changes, or timing. Don’t just quit the drug. Work with your provider to find a solution.
Knowing the difference between side effects and allergies isn’t just about avoiding discomfort. It’s about avoiding unnecessary risks, saving money, and getting the right treatment when you need it most. Don’t let a label from 10 years ago dictate your health today.
Can you outgrow a drug allergy?
Yes, especially with penicillin. About 80% of people who had a true penicillin allergy as a child lose the sensitivity within 10 years. That’s why retesting is so important-even if you were told you were allergic decades ago, you might be able to safely take it now.
Is a rash always a sign of allergy?
No. Many rashes from drugs are side effects, not allergies. For example, amoxicillin can cause a non-allergic rash in up to 90% of kids with mono. That rash isn’t dangerous and doesn’t mean you’re allergic to penicillin. True allergic rashes are usually itchy, raised, and appear quickly. A flat, non-itchy rash that shows up a week later is often a delayed reaction but still requires evaluation.
Can you have an allergic reaction the first time you take a drug?
Yes. Unlike food allergies, which often need prior exposure, drug allergies can happen the first time. Your immune system might have been sensitized by a similar molecule in the environment or a past infection. That’s why even first-time users can have severe reactions.
Do all drug allergies show up right away?
No. Immediate reactions (IgE-mediated) happen within minutes to two hours. But delayed reactions, like Stevens-Johnson syndrome or drug rash with eosinophilia, can take days or even weeks to develop. These are still true allergies and require immediate medical attention.
If I’m allergic to penicillin, am I allergic to all antibiotics?
No. Penicillin allergies are specific to the penicillin family-amoxicillin, ampicillin, and similar drugs. You’re not automatically allergic to unrelated antibiotics like azithromycin, doxycycline, or ciprofloxacin. Cross-reactivity is low with other classes. Testing can confirm what you can safely take.
Can I take an antihistamine if I have a drug allergy?
Antihistamines can help with mild symptoms like itching or hives, but they won’t stop anaphylaxis. If you have trouble breathing, swelling in your throat, or dizziness, you need epinephrine and emergency care. Never rely on antihistamines alone for a suspected allergic reaction.
What’s Next?
If you’ve ever been told you have a drug allergy, especially to penicillin, sulfa, or NSAIDs, ask your doctor about getting tested. It’s quick, safe, and can open up better treatment options. Many hospitals now offer drug allergy clinics. Even if you’ve been avoiding a drug for years, it’s never too late to find out if you’re truly allergic-or just had a side effect.And if you’re a patient or caregiver, don’t accept vague labels. Push for specifics: What happened? When? How bad? Was it tested? Your health depends on getting the right answer.






Shawn Raja
So let me get this straight - we’re telling people to stop calling a headache an allergy because it’s ‘not immune-related’? Cool. So next time my boss says I’m allergic to meetings, I’ll just tell him it’s a side effect of corporate drudgery. At least that’s scientifically accurate.
Dan Nichols
Penicillin allergy misdiagnosis is a national scandal. 80 percent false positives means millions of people are getting worse antibiotics because someone wrote ‘allergic’ in a chart after a rash in 1998. No one ever follows up. No one ever checks. The system is broken and we’re all paying for it in higher bills and MRSA rates. It’s not just ignorance - it’s negligence wrapped in bureaucracy.
Shweta Deshpande
This post made me feel so seen. I thought I was allergic to ibuprofen because I got a headache once - turns out I was just dehydrated and stressed. My doctor finally helped me figure it out after I kept pushing back. Don’t assume your body is broken. Sometimes it’s just trying to tell you to drink more water or sleep better. You’re not broken - you’re just learning. And that’s okay.
Jessica Knuteson
Side effects are pharmacological. Allergies are immunological. That’s the whole thing. Everything else is just noise. The fact that people conflate them shows how little basic biology people actually understand. Not blaming anyone - just stating a fact.
Ashley Porter
The BAT test is legit. I had a false penicillin label for 12 years. Got the basophil activation test done last year - negative. Now I’m on amoxicillin for my sinus infection. No drama. No hives. Just a clean script and a 70% cheaper bill. If you’ve been told you’re allergic, get tested. It’s not a big deal. It’s a life upgrade.
SWAPNIL SIDAM
My cousin got a rash after amoxicillin when he had mono. Everyone said he was allergic. He avoided all penicillin for 15 years. Then he got a bad tooth infection and his dentist said ‘try amoxicillin anyway’ - no reaction. Turns out it was the virus, not the drug. Sometimes your body is just having a bad day.
Geoff Miskinis
It’s fascinating how Americans treat drug allergies like religious dogma. You say you’re allergic to penicillin? Fine. But you’re not a martyr - you’re a statistical outlier who never got tested. Meanwhile, in Europe, they do oral challenges like it’s Tuesday. We’ve turned medical caution into performative caution. Pathetic.
Sally Dalton
I just had my first skin test for penicillin and it was so easy! Like a tiny prick and then you wait 15 mins. No pain. No drama. I’ve been saying I’m allergic since I was 8 because my mom said so. Turns out I’m not. I cried a little. Not because I was scared - because I realized I’d been denying myself good medicine for over 20 years. Thank you for this post. I’m updating my chart right now.
Betty Bomber
My mom’s chart says ‘allergic to NSAIDs’ because she got a stomach ache once. She’s been on opioids for arthritis for 7 years. She could’ve been on celecoxib. She’s not allergic. She’s just unlucky with timing. Why do we let old notes dictate new lives?
Mohammed Rizvi
My uncle got anaphylaxis from penicillin at 19. 30 years later, he got tested. Still allergic. But here’s the twist - he’s now on a desensitization protocol for his pneumonia. They’re giving him microdoses under supervision. He’s been doing it for 6 weeks. He’s not cured. But he’s breathing. And that’s more than most people get when they’re labeled ‘allergic’ and left to rot with vancomycin.
eric fert
Let’s be real - this whole thing is a corporate distraction. Big Pharma doesn’t want you knowing side effects are normal because then you’d stop taking drugs too soon. And they sure as hell don’t want you getting tested for allergies because then you’d stop paying $500 for a useless antibiotic that’s just a rebranded version of penicillin from the 1940s. They profit from confusion. They profit from fear. They profit from you never asking questions. So yes, get tested. But don’t think this is about your health. It’s about who gets paid when you do.
I’ve been on statins for 12 years. Muscle pain? Check. Fatigue? Check. Nausea? Triple check. But I kept taking it because my doctor said ‘it’s just a side effect.’ Now I’ve got rhabdo. Guess what? That wasn’t just a side effect. That was negligence. And now I’m here. And you’re reading this. So what’s your excuse?
Don’t trust your doctor. Don’t trust your chart. Don’t trust the FDA’s list. Ask. Push. Demand. Test. Because if you don’t, someone else will decide what’s safe for your body - and they’ll be wrong. Again.
And if you think this is dramatic - you haven’t seen the ER report from last month. The one where a woman died because they gave her vancomycin instead of penicillin because her chart said ‘allergy.’ She had a 98% chance of surviving with the right drug. She died because of a typo in 1999. And now her kid’s asking why the system didn’t save her. What do you tell them?
I’m not angry. I’m just done pretending this is about science. It’s about money. And we’re all just collateral.