Renal Dosing Calculator
How Kidney Function Affects Your Medications
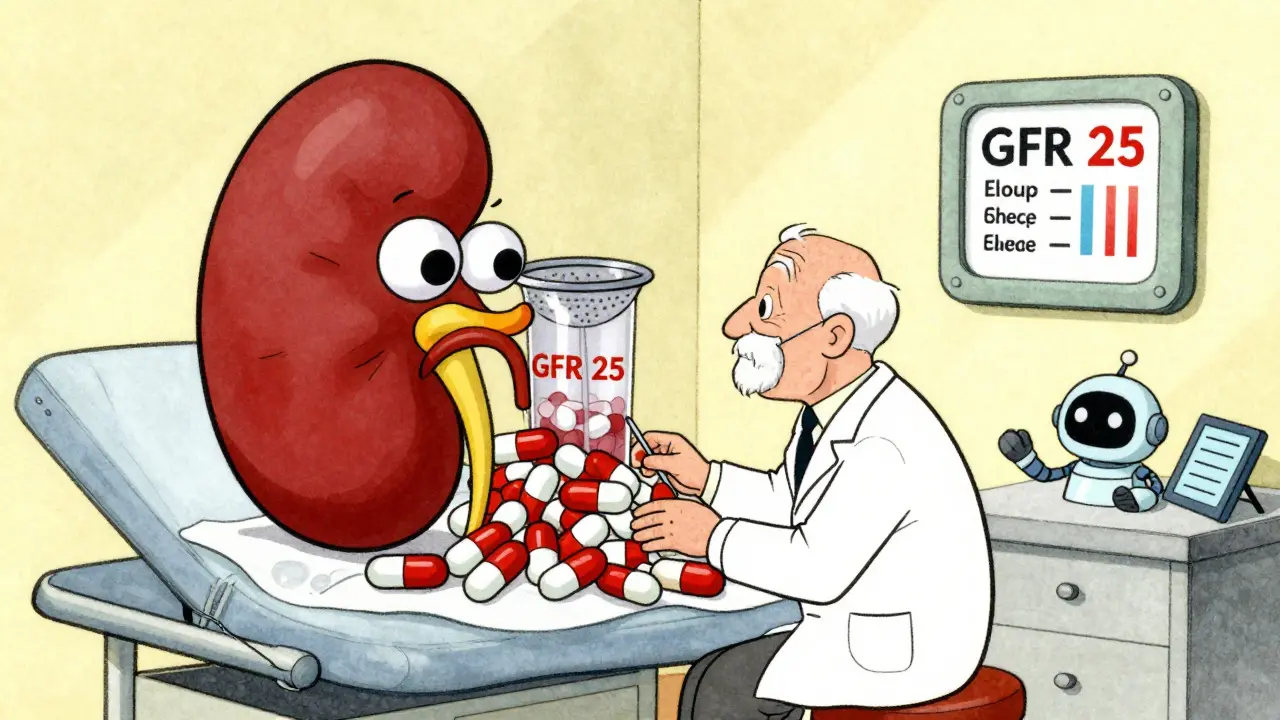
Your kidneys filter drugs from your blood. As kidney function declines (low GFR), drugs can build up to toxic levels. This tool estimates your Glomerular Filtration Rate (GFR) and shows how it affects dosing for common medications.
Your Estimated GFR
Mild impairment: 60-89 mL/min
Moderate impairment: 30-59 mL/min
Severe impairment: <30 mL/min
Dosing Recommendation
Have you ever taken a pill and wondered why it made you dizzy one day but not the next? Or why your grandma gets sick from a drug that barely affects you? It’s not luck. It’s not magic. It’s pharmacokinetics-the science of how your body moves, changes, and gets rid of drugs. This isn’t just for doctors and pharmacists. If you take any medication, even over-the-counter ones, understanding this process can help you avoid dangerous side effects and get the most out of your treatment.
What Happens When You Swallow a Pill?
When you take a drug, whether it’s a pill, injection, or patch, your body doesn’t just let it sit there. It starts moving it around, changing it, and eventually flushing it out. This four-step journey is called ADME: Absorption, Distribution, Metabolism, and Excretion. Each step has a direct impact on whether the drug works well-or causes harm.Let’s start with absorption. This is how the drug gets into your bloodstream. If you swallow a pill, it has to survive your stomach acid, pass through your gut lining, and avoid being broken down before it even gets started. Only about 40-60% of most oral drugs actually make it into your blood. That’s because of something called first-pass metabolism. Your liver gets the first shot at breaking down the drug before it reaches the rest of your body. Some drugs, like nitroglycerin, are given under the tongue so they skip this step and work faster.
Not all drugs are absorbed the same way. Some rely on passive diffusion-just drifting through cell membranes. Others need special transporters. One of these, called P-glycoprotein, can block up to 70% of certain drugs from entering your cells. If you’re on digoxin for heart problems, this transporter can make a big difference in how much of the drug actually works.
Where Does the Drug Go After It Enters Your Blood?
Once in your bloodstream, the drug doesn’t just hang out in your veins. It spreads out into your tissues. How far it goes depends on something called volume of distribution (Vd). A low Vd means the drug stays mostly in your blood-like warfarin, which clings to proteins. A high Vd means it dives deep into your fat and organs-like lithium, which gets into your brain and kidneys.Here’s the catch: most drugs bind to proteins in your blood. Warfarin, for example, is 98% stuck to albumin. Only the 2% that’s floating free can actually do its job. If another drug comes along and kicks warfarin off those proteins-say, an antibiotic like sulfamethoxazole-your free warfarin level spikes. That’s when you risk dangerous bleeding. This is why drug interactions aren’t just a warning on the label. They’re a direct result of how drugs compete for space in your blood.
How Your Liver Changes the Drug
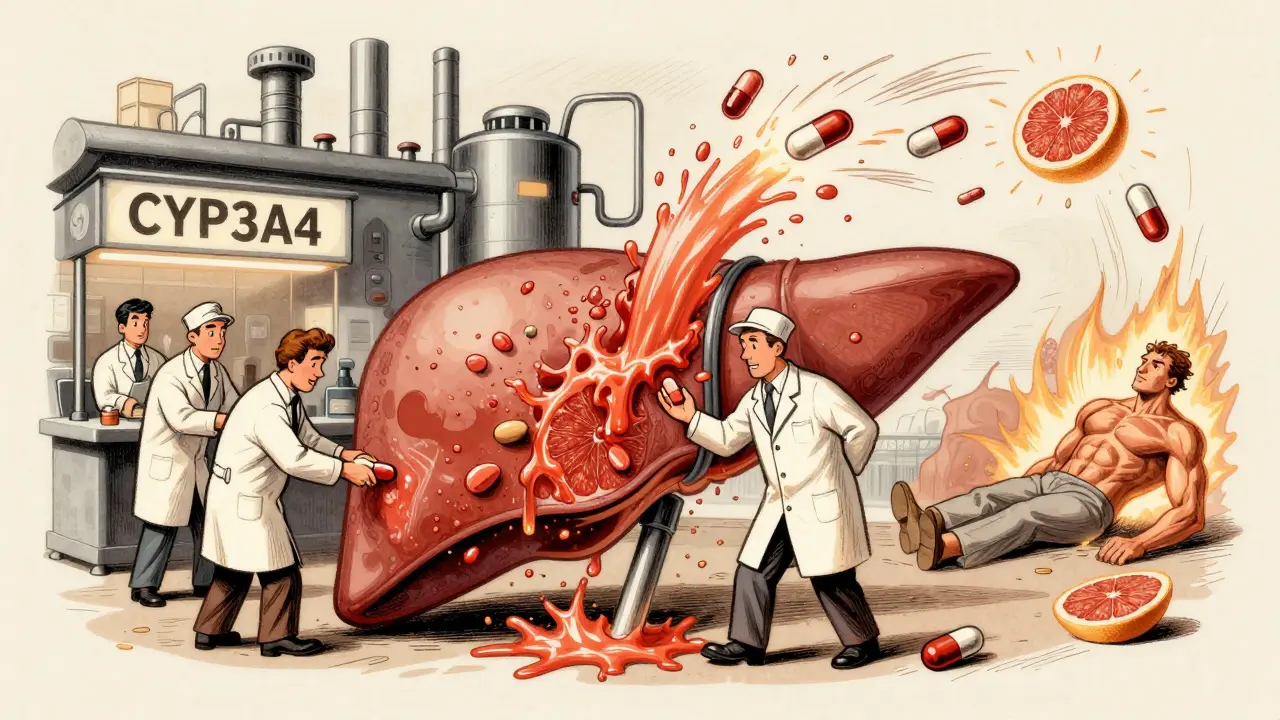
Metabolism is where things get personal. Your liver uses enzymes-mostly from the Cytochrome P450 family-to turn fat-soluble drugs into water-soluble ones so your kidneys can flush them out. The most important enzyme? CYP3A4. It handles about half of all prescription drugs, including statins, antidepressants, and painkillers.But here’s the problem: your version of CYP3A4 might be very different from your neighbor’s. Genetics play a huge role. About 3-10% of white people have a slow version of CYP2D6. That means codeine, which needs to be turned into morphine by this enzyme, won’t work for them. For others, the enzyme works too fast. They get too much morphine too quickly and risk overdose.
Some drugs don’t just get broken down-they turn into new active compounds. Diazepam (Valium) breaks down into desmethyldiazepam, which lasts up to 100 hours. That’s why elderly patients feel sleepy for days after one dose. Their livers can’t clear it fast enough. And if you’re taking another drug that blocks CYP3A4-like grapefruit juice, clarithromycin, or even some antifungals-you can accidentally triple or quadruple your drug levels. That’s how a routine statin turns into a muscle-destroying nightmare.
How Your Kidneys Flush It Out
Excretion is the final step. Most drugs leave your body through your kidneys. Your kidneys filter blood at a rate called glomerular filtration rate (GFR). Normal GFR? 90-120 mL/min. But if you’re over 65, have diabetes, or have kidney disease, that number can drop below 30. And if your doctor doesn’t adjust your dose? You’re at risk.Vancomycin, a powerful antibiotic, is a classic example. Standard doses can cause kidney damage in people with low GFR. One patient in a Reddit thread shared how their 78-year-old relative developed acute kidney failure after taking vancomycin at the usual dose. Their creatinine clearance was only 25 mL/min-far below what’s safe. The dose wasn’t adjusted. The damage was preventable.
Some drugs are also cleared through bile and poop, but kidneys handle about 80% of the load. That’s why doctors check your creatinine levels before prescribing anything. It’s not just a routine test. It’s a safety check.
Why Side Effects Aren’t Random
Side effects aren’t accidents. They’re predictable outcomes of pharmacokinetics. When drug levels go too high, you get toxicity. Too low, and the drug doesn’t work. The gap between effective and toxic is narrow for some drugs-like lithium, warfarin, or phenytoin.Take phenytoin. At therapeutic levels (10-20 mcg/mL), it controls seizures. But at 20 mcg/mL or higher, 30% of patients develop side effects: shaky hands, slurred speech, even confusion. That’s not bad luck. That’s a pharmacokinetic failure. The drug built up because the liver couldn’t break it down fast enough, or the kidneys couldn’t flush it out.
Age is a huge factor. People over 65 have 30-50% less liver function and 30-40% lower kidney clearance. That’s why older adults are three times more likely to have bad reactions to drugs. It’s not that they’re fragile. It’s that their bodies process drugs slower.
Drug interactions are another major cause. One study found that 20-30% of serious side effects come from two drugs clashing in the liver. Clarithromycin (an antibiotic) blocks CYP3A4, causing simvastatin (a cholesterol drug) to build up. That raises the risk of rhabdomyolysis-from 0.04% to 0.5%. That’s a 12-fold increase. And it’s all because of how the body handles the drugs.
Personalized Dosing Is Here-And It’s Changing Everything
Doctors used to guess doses based on weight and age. Now, they’re using real data. Therapeutic drug monitoring (TDM) measures exactly how much drug is in your blood. For drugs like vancomycin or phenytoin, this is standard practice. But it’s not perfect. One study found that 22% of hospitals draw blood samples at the wrong time-skewing results.Now, AI is stepping in. The FDA approved DoseMeRx in 2021, an AI tool that cuts vancomycin dosing errors by 62%. It uses your weight, age, kidney function, and even your genetics to calculate your perfect dose. No more trial and error.
Genetic testing is also becoming routine. Before prescribing abacavir (an HIV drug), doctors now test for the HLA-B*5701 gene. If you have it, you’re at risk of a life-threatening allergic reaction. Testing prevents 90% of those reactions. For clopidogrel, a blood thinner, CYP2C19 testing tells doctors if the drug will even work for you. If you’re a poor metabolizer, you need a different drug.
What You Can Do Right Now
You don’t need a lab to protect yourself. Here’s what actually works:- Always tell your doctor and pharmacist every medication you take-including vitamins, supplements, and herbal teas.
- Ask: “Could this drug interact with anything else I’m taking?” Especially if you’re on three or more meds.
- If you’re over 65 or have kidney or liver disease, ask if your dose needs to be adjusted.
- Don’t ignore side effects. Dizziness, nausea, or muscle pain aren’t just “annoyances.” They could be early signs of toxicity.
- If you’re on a drug with a narrow window (warfarin, lithium, digoxin), ask about therapeutic drug monitoring.
The goal isn’t to scare you. It’s to empower you. Your body isn’t a black box. It’s a complex, predictable system. When you understand how drugs move through it, you stop being a passive patient. You become a partner in your own care.
What’s Next for Drug Safety?
Researchers are now studying the gut microbiome-trillions of bacteria in your intestines. Turns out, they can break down 15-20% of oral drugs before your liver even gets a chance. That might explain why two people on the same dose have totally different responses.The NIH just launched a $185 million project to fix a big gap: most pharmacokinetic studies still use young, white, male volunteers. But 85% of people taking medications are women, older adults, or people of color. Their bodies process drugs differently. Until we fix that, we’ll keep missing side effects.
By 2030, experts predict we can cut emergency visits from bad drug reactions-from 1.3 million a year down to under 400,000. That’s not science fiction. It’s the next step in medicine: personalized, precise, and powered by pharmacokinetics.
What does pharmacokinetics mean?
Pharmacokinetics is the study of how your body absorbs, distributes, metabolizes, and excretes a drug. It answers the question: "What does your body do to the drug?" This is different from pharmacodynamics, which looks at what the drug does to your body.
Why do some people have worse side effects than others?
Differences in genetics, age, kidney and liver function, and other medications all affect how fast or slow your body processes drugs. For example, 3-10% of people can’t activate codeine properly due to a genetic variation, while others break it down too fast. Older adults and those with kidney disease often build up drugs to toxic levels because their bodies clear them slower.
Can food or supplements affect how my drug works?
Yes. Grapefruit juice blocks CYP3A4, which can cause dangerous spikes in statins, blood pressure meds, and some anxiety drugs. St. John’s wort speeds up drug breakdown, making some medications ineffective. Even high-fiber diets can slow absorption. Always check with your pharmacist before mixing supplements with prescriptions.
How do I know if my drug dose is right for me?
For drugs like warfarin, lithium, or vancomycin, doctors use blood tests to measure drug levels and adjust doses. If you’re on one of these, ask if therapeutic drug monitoring is recommended. For others, side effects are your best clue. If you feel worse after starting a drug, don’t assume it’s "just adjusting." Talk to your provider.
Are generic drugs processed the same way as brand-name ones?
Yes. Generic drugs must prove they deliver the same amount of active ingredient into your bloodstream as the brand-name version. But inactive ingredients (fillers, coatings) can affect absorption speed. For drugs with a narrow therapeutic window-like seizure meds or thyroid hormones-some patients do better on one brand. If you notice a change after switching, tell your doctor.
Is pharmacokinetics only for serious medications?
No. Even common drugs like ibuprofen, acetaminophen, or antihistamines are affected by pharmacokinetics. Taking too much acetaminophen can cause liver damage because your liver can’t process it fast enough. If you drink alcohol regularly or have liver disease, your risk goes up. Understanding how your body handles even simple drugs helps you avoid harm.






Kylie Robson
Pharmacokinetics isn't just a buzzword-it's the bedrock of clinical decision-making. First-pass metabolism, volume of distribution, CYP polymorphisms-these aren't abstract concepts. They're the reason your 70-year-old aunt gets sedated on 5mg of lorazepam while you need 15mg to feel a thing. The liver's CYP3A4 and CYP2D6 isoforms are the gatekeepers, and genetic variability explains why 30% of the population are poor or ultrarapid metabolizers. This isn't placebo territory. It's biochemistry with real-world consequences.
And let's not ignore transporter proteins like P-gp. That's why digoxin levels fluctuate wildly between patients even on identical doses. The FDA's Therapeutic Drug Monitoring guidelines exist for a reason. You're not just taking a pill. You're engaging with a dynamic, individualized pharmacological system.
Most patients don't realize that grapefruit juice inhibits CYP3A4 with the potency of a pharmaceutical-grade inhibitor. It's not anecdotal. It's in the prescribing info for 85+ drugs. Yet people still drink it with their statins. That's not ignorance-it's systemic failure in patient education.
And the microbiome? Still an emerging frontier. Gut bacteria metabolize 15-20% of oral drugs. That's why two people on the same regimen have wildly different outcomes. Fecal transplants aren't just for C. diff anymore. They're pharmacokinetic wildcards.
We're moving toward precision dosing. AI-driven platforms like DoseMeRx are already reducing vancomycin toxicity by 62%. But until we standardize genetic screening across all prescribers, we're just band-aiding a broken system.
And yes-generics are bioequivalent. But bioequivalent doesn't mean identical. The excipients matter. For phenytoin or levothyroxine, switching brands can trigger toxicity or underdosing. That's not hype. That's documented in the literature.
Stop treating meds like candy. Your body isn't a black box. It's a finely tuned, genetically coded machine. Ignore pharmacokinetics at your peril.
Todd Scott
It's fascinating how much of medicine still operates on guesswork, especially when you consider how much we actually know about drug metabolism. I remember when my uncle was on warfarin and his INR kept spiking-turns out he started taking a new herbal supplement for arthritis. Turns out it was blocking his CYP2C9 enzyme. He didn't even think to mention it because he called it ‘all natural.’
And that’s the problem. People think ‘natural’ means ‘safe’ or ‘doesn’t interact.’ But St. John’s wort? It’s a potent inducer of CYP3A4 and P-glycoprotein. It can drop blood levels of birth control, antidepressants, even cyclosporine. I’ve seen patients go into rejection after transplant because their doctor didn’t ask about supplements.
Then there’s age. We treat elderly patients like they’re just ‘slower,’ but it’s not just about metabolism. It’s reduced renal clearance, lower albumin, increased fat mass. A standard dose of diazepam can linger for days because the metabolites accumulate. That’s not ‘old age’-that’s pharmacokinetics in action.
And don’t get me started on how little training primary care docs get in this. I’ve had patients on five meds, no one checking for interactions, no TDM, no genetic screening. We’re flying blind. AI tools like DoseMeRx are a start, but they’re not in every clinic. We need mandatory pharmacokinetics modules in med school. Not as an elective. As a core.
And the research gap? Yeah. 85% of patients are women, older adults, people of color. But most PK studies? Young white men. That’s not science. That’s bias dressed up as methodology. Until we fix that, we’re just guessing for half the population.
It’s not enough to say ‘take your meds.’ We need to teach people how their body works with them. Not as patients. As partners.
Andrew Gurung
OMG I CANNOT BELIEVE PEOPLE STILL THINK DRUGS WORK THE SAME FOR EVERYONE 😭
Like bro, I took 200mg of sertraline and felt fine, but my cousin took 50mg and had a seizure. It’s not ‘mental health stigma’-it’s CYP2D6 ultra-rapid metabolism. Your body turns it into serotonin like a damn factory. And then you wonder why people ‘overreact’ to meds? It’s not drama. It’s biochemistry.
And grapefruit juice?? 😤 I told my dentist I don’t drink it before my statin. He laughed. Then I Googled it and showed him the FDA warning. He apologized. 🤷♂️
Also, generics? Nah. I switched from brand-name Lamictal to generic and got a rash that looked like I got attacked by fire ants. Took 3 weeks to clear. My neurologist said ‘it’s probably coincidence.’ COINCIDENCE?? I’m not a lab rat.
And why does no one talk about the microbiome?? My gut bacteria are probably turning my meds into poison. I’ve been doing probiotics and now I feel like a new person. Science is late to the party, as usual.
Also, why are we still using creatinine clearance? It’s 1970s tech. We need real-time metabolite tracking. Like a Fitbit for your liver. I’m starting a GoFundMe.
PS: If you think ‘just take your pills’ is enough-you’re part of the problem. 💀
Paula Alencar
It is with profound respect for the complexity of human physiology that I feel compelled to underscore the urgency of integrating pharmacokinetic literacy into public health education. The notion that medications are inert substances, uniformly effective and universally tolerated, is not only scientifically inaccurate-it is dangerously misleading.
When we fail to recognize that genetic polymorphisms in cytochrome P450 enzymes govern the metabolic fate of over half of all clinically prescribed agents, we are not merely overlooking a biochemical detail; we are perpetuating a systemic failure in patient safety. The case of codeine, which requires conversion to morphine via CYP2D6, illustrates this with tragic clarity: individuals who are poor metabolizers derive no analgesic benefit, while ultrarapid metabolizers may experience life-threatening respiratory depression-even at therapeutic doses.
Moreover, the decline in hepatic and renal function with aging is not merely an incidental consequence of time, but a quantifiable, predictable alteration in volume of distribution, protein binding, and clearance kinetics. To administer the same dosage regimen to a 25-year-old and a 75-year-old without adjustment is not clinical practice-it is negligence dressed in tradition.
Therapeutic drug monitoring, genetic testing for HLA-B*5701 prior to abacavir administration, and AI-driven dosing algorithms are not futuristic concepts-they are evidence-based imperatives. Yet their adoption remains fragmented, uneven, and inaccessible to vast swaths of the population.
Let us not mistake convenience for competence. The responsibility for safe pharmacotherapy does not rest solely with the prescriber. It begins with the patient’s understanding. We must advocate for curricula in high schools, community centers, and pharmacies that demystify ADME-not as jargon, but as the architecture of survival.
Nikki Thames
You know what’s really sad? That we’re still talking about this like it’s new. People have been dying from drug interactions since the 1950s. Thalidomide. Reye’s syndrome. The phenylbutazone carnage. We’ve known for decades that bodies aren’t interchangeable.
And yet, doctors still write scripts like they’re ordering coffee. ‘Two of these, no sugar.’ No. Your liver doesn’t work like mine. Your kidneys aren’t mine. Your genes aren’t mine.
And why do we still let people take supplements without asking? St. John’s wort, goldenseal, kava-these aren’t harmless teas. They’re enzyme modulators. They’re silent saboteurs. And no one ever asks. Not the pharmacist. Not the doctor. Not even the patient.
It’s not about being ‘careful.’ It’s about accountability. If your body can’t process a drug safely, why are we still pretending it’s your fault you got sick? It’s not your fault. It’s the system’s. The system that treats 70-year-olds like they’re just ‘fragile’ instead of metabolically distinct.
And the microbiome? We’ve known for 15 years gut bacteria alter drug metabolism. But the FDA still doesn’t require microbiome data in trials. Why? Because it’s inconvenient. Because it’s expensive. Because it’s easier to blame the patient.
We don’t need more apps. We need a reckoning.
Chris Garcia
In my homeland of Nigeria, we do not have the luxury of AI dosing tools or genetic screening. But we have something deeper: wisdom passed through generations. My grandmother never read a pharmacokinetics paper, yet she knew that if you took papaya leaf tea with blood pressure medicine, you might faint. She didn’t know CYP3A4-but she knew the body speaks.
Here, we don’t call it ‘pharmacokinetics.’ We call it ‘respect for the medicine.’ If the pill is strong, you take less. If you are old, you wait. If you are weak, you rest. We don’t have labs, but we have intuition honed by survival.
Yet modern medicine treats African bodies as if they are broken versions of Western ones. The NIH study you mention? We’ve been living it for decades. Our people get sick from doses that work fine in the U.S. because the research never included us.
It’s not about technology. It’s about dignity. Your body isn’t a lab rat. It’s a story. And every story deserves to be heard-even if it doesn’t speak English.
Maybe the future isn’t in AI. Maybe it’s in listening.
Gerald Tardif
I’ve been a nurse for 22 years and I still see this every day. Someone comes in with a rash after starting a new med. Doctor says ‘allergy.’ I ask ‘what else are you taking?’ Turns out they started taking turmeric for ‘inflammation.’ Turmeric inhibits CYP2C9 and CYP3A4. That’s why the warfarin spiked. Not an allergy. A drug interaction.
Patients don’t know this stuff. And honestly? Most providers don’t either. I’ve seen residents write prescriptions for simvastatin and clarithromycin together-no idea they’re playing Russian roulette with rhabdomyolysis.
But here’s the good part: when you sit down with a patient and explain it simply-‘your liver is like a factory. This drug is a wrench in the gears’-they get it. They start asking questions. They stop taking random supplements. They tell their doctors about everything.
It’s not about scaring people. It’s about giving them the tools. Knowledge is the quietest form of power. And it’s free.
Robyn Hays
My mom’s on six meds. I started keeping a spreadsheet. Not because I’m a nerd-because I had to. One day she got dizzy and nearly fell. We found out it was because she started taking a new magnesium supplement. It slowed her kidney clearance of digoxin. Her levels went from 0.8 to 1.9. Toxic.
But here’s the thing: no one told her to stop the magnesium. Not the pharmacist. Not the doctor. She just thought ‘more minerals = better.’
So I started asking questions for her. ‘What does this interact with?’ ‘Is there a blood test for this?’ ‘Is this dose right for her age?’ Turns out, most of her meds could be lowered. One was even unnecessary.
It’s exhausting. But I’d rather be the annoying daughter than the one who lost her mom to a preventable reaction.
And honestly? I think every family should do this. Keep a list. Talk to the pharmacist. Don’t assume ‘it’s fine.’ It’s not fine until you know why.
Liz Tanner
my grandma took lisinopril and got so dizzy she fell and broke her hip. they said it was 'old age' but i looked it up-her creatinine was low, her dose wasn't adjusted. she was on the same dose as someone half her size. it wasn't luck. it was negligence.
i started asking every doctor: 'is this dose right for her kidneys?' now they just hand me the chart and say 'good question.'
we don't need fancy tech. we just need to stop pretending everyone's the same.
Babe Addict
Pharmacokinetics? More like pharmacofake. The whole thing is a scam designed to sell more drugs. Did you know the FDA approves drugs based on 12-week trials? But people take them for YEARS. So they just make up numbers. 'Oh, 90% effective!' But what about the 10% who get liver failure? They call it 'rare.'
And genetics? Please. They test for HLA-B*5701 because they got sued after a bunch of people died. Now it's 'standard.' But for everything else? Nah. Still guessing.
And AI dosing? That’s just Big Pharma’s way of making you think they care. They still charge $1,200 for a 30-day supply of insulin. The 'science' is just a cover.
Take less. Eat real food. Don’t trust the system.
Satyakki Bhattacharjee
People forget that the body is a temple. When you poison it with chemicals, you are not just affecting your liver-you are offending your soul. Why do you think so many get sick? Because they do not live in harmony with nature. Why do you think the elderly suffer? Because they lost their spiritual balance.
God gave us herbs. He gave us water. He gave us rest. But we chase pills like they are magic. This is arrogance. This is sin.
My village in India never used these drugs. We used neem. We used turmeric. We used fasting. We were healthy. Now the young ones take pills like candy. And they wonder why they are weak?
It is not the body that is broken. It is the mind.
Kishor Raibole
Let us be clear: the modern pharmacological paradigm is a monument to reductionist hubris. To reduce the human organism to a series of enzymatic pathways, transporter proteins, and clearance rates is to commit epistemological violence upon the very essence of life.
The body is not a machine. It is a living, breathing, dynamic field of energy, intention, and ancestral memory. To quantify its response to xenobiotics through CYP isoforms is to reduce the sacred to the statistical.
Moreover, the insistence on genetic testing and AI-driven dosing is not progress-it is colonization of the biological self. Who authorized the state, the pharmaceutical conglomerate, or the algorithm to determine your metabolic destiny?
True healing lies not in precision dosing, but in reconnection-with the earth, with silence, with the rhythms of dawn and dusk. No algorithm can calculate the healing power of a mother’s prayer.
Let the pill rest. Let the body breathe. Let the soul speak.
Anna Weitz
I’ve been on 14 different meds over 8 years and every single one gave me side effects. They said it was 'adjustment' or 'anxiety.' But I kept track. Every time I started a new drug, I got brain fog within 72 hours. Always. I stopped taking them all. My brain cleared in 3 weeks.
Turns out I’m a slow metabolizer for like 7 enzymes. No one tested me. No one asked. They just kept adding pills.
Now I’m on zero. And I feel better than I have since I was 18.
They don’t want you to know this. Because if you stop taking meds, they lose money.
And yes. I know I’m the exception. But what if I’m not?
They’re not testing for me. They’re testing for the average. And the average is a lie.
Jane Lucas
i took a new blood pressure med and felt like i was floating. thought it was anxiety. turned out my kidney function dropped and the dose was too high. doctor didn't check my creatinine. i had to beg for the test.
now i ask for it every time. no one else does. weird.
Elizabeth Alvarez
Did you know the FDA allows drug companies to test on prisoners and college students? That’s why the data is skewed. They don’t test on old people, minorities, or women because they’re ‘too complicated.’
And the AI tools? They’re trained on that biased data. So they’re just making the same mistakes faster.
Also-your gut bacteria are being altered by Roundup in your food. That’s why drugs don’t work the same anymore. The microbiome is being poisoned. It’s not genetics. It’s corporate pollution.
And they’re hiding it. They don’t want you to know your body is being slowly destroyed by chemicals you can’t even name.
They’re not trying to help you. They’re trying to sell you a cure for something they created.
Kylie Robson
That’s exactly why I said AI isn’t enough. DoseMeRx is trained on the same flawed data. If the original trials excluded women over 65, the AI will keep prescribing them the same dangerous doses. It’s not magic. It’s garbage in, garbage out.
And don’t get me started on the microbiome studies. They’re still using fecal samples from young, healthy volunteers. Meanwhile, 70% of patients on chronic meds have dysbiosis from antibiotics, PPIs, and sugar. The AI doesn’t account for that.
Until we fix the data, we’re just automating bias.