When you take an H2 blocker like famotidine or cimetidine for heartburn, you’re probably not thinking about your antifungal or antiviral meds. But if you’re on both, you could be risking treatment failure - even if you’re taking them exactly as prescribed. This isn’t theoretical. Real patients have had fungal infections come back, HIV viral loads spike, and antiviral therapies collapse - all because of a simple, overlooked timing issue between acid-reducing drugs and medications that need stomach acid to work.
What H2 Blockers Actually Do
H2 blockers - histamine H2-receptor antagonists - cut stomach acid by blocking the signal that tells acid-producing cells to turn on. The first one, cimetidine (Tagamet), hit the market in 1977. Today, three are still available in the U.S.: famotidine (Pepcid), cimetidine, and nizatidine. Ranitidine (Zantac) was pulled in 2020 after being found contaminated with a cancer-causing chemical.
These drugs raise your stomach pH from around 1-3 (strongly acidic) to 4-6 (mildly acidic). That’s great for reducing ulcers or GERD symptoms. But for some antivirals and antifungals, that change in pH is a dealbreaker. Many of these drugs need that low pH to dissolve properly so your body can absorb them. If the acid isn’t there, the drug just passes through you - useless.
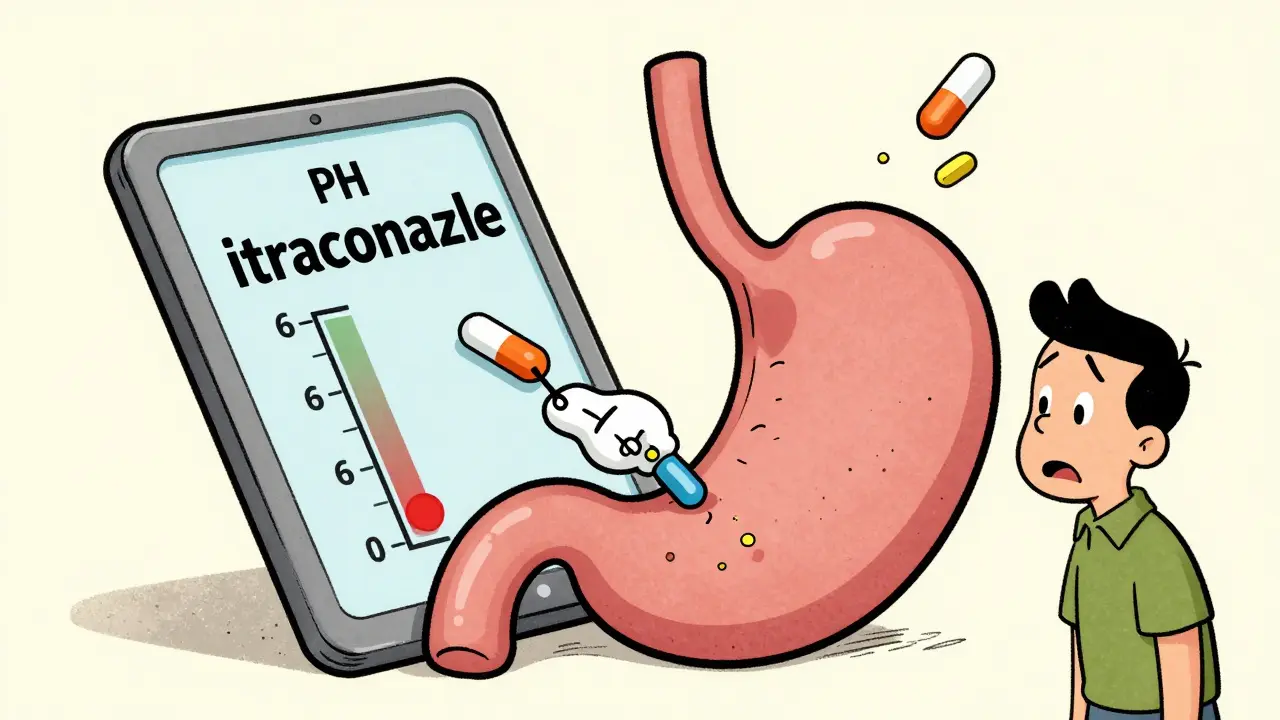
Why Some Antifungals Fail With H2 Blockers
Not all antifungals are affected the same way. The big problem is with itraconazole, a common treatment for fungal lung infections and nail fungus. Studies show that when taken with an H2 blocker, itraconazole absorption drops by 40-60%. That’s enough to let the infection grow back. The reason? Itraconazole tablets need acid to break down. Without it, they just sit there.
But here’s the twist: the liquid form of itraconazole contains citric acid, which helps it dissolve even in higher pH environments. So if you’re on an H2 blocker and need itraconazole, your doctor might switch you to the solution instead of the pill.
Fluconazole? No problem. It dissolves easily in water, no acid needed. Voriconazole and posaconazole? Mixed bag. Voriconazole’s absorption isn’t affected much by pH, but it’s metabolized by liver enzymes that cimetidine can block - leading to dangerous buildup. Posaconazole’s label says to take it at least 2 hours before or after an H2 blocker. Isavuconazole? One of the safest. It doesn’t rely on acid and barely touches liver enzymes.
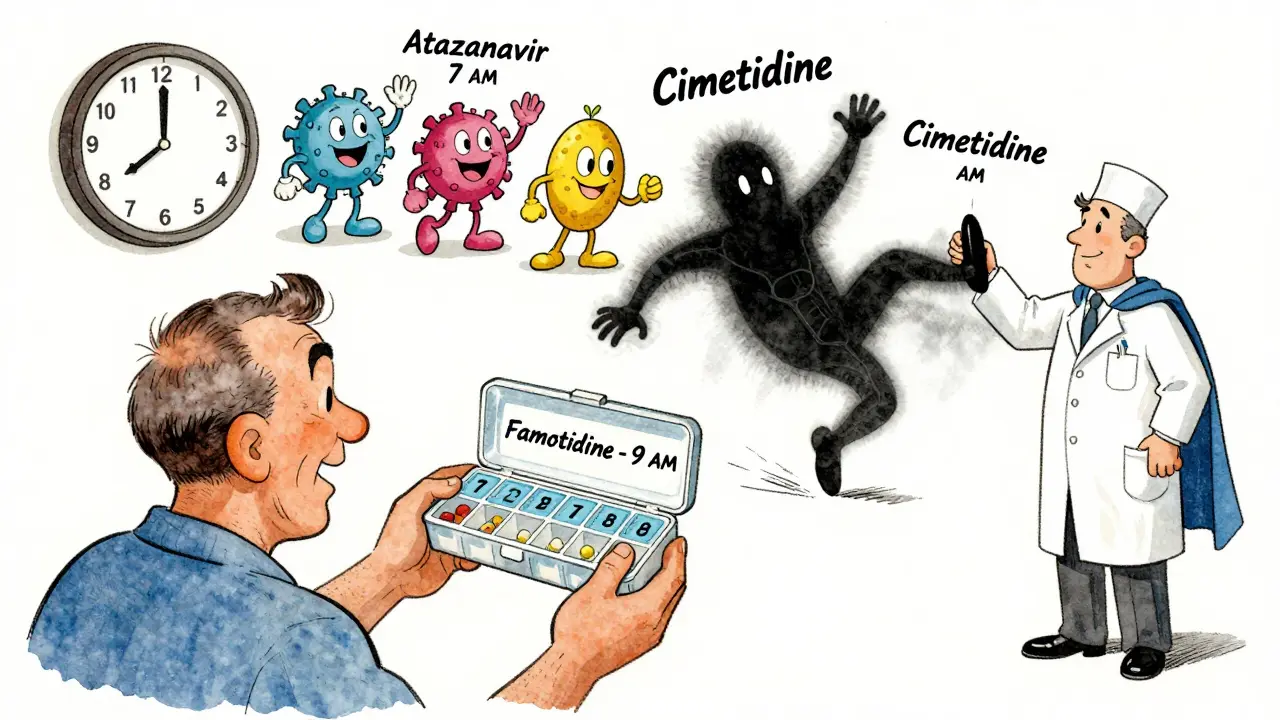
Antivirals That Can’t Handle Less Acid
Antivirals aren’t off the hook either. Take atazanavir, an HIV drug. A 2022 FDA review found that when taken with famotidine, atazanavir exposure dropped by up to 77%. That’s not a small drop - it’s enough to let the virus replicate and develop resistance. The FDA’s official advice? Take atazanavir at least 2 hours before the H2 blocker. That gives it time to absorb in a more acidic stomach before the blocker kicks in.
Dasatinib, used for certain leukemias and sometimes off-label for viral complications, has the same issue. So do other antivirals with low solubility: rilpivirine, nelfinavir, and some hepatitis C drugs. In total, 68% of antiviral labels now include warnings about acid-reducing agents. That’s not a coincidence - it’s a pattern. And many patients never hear about it.
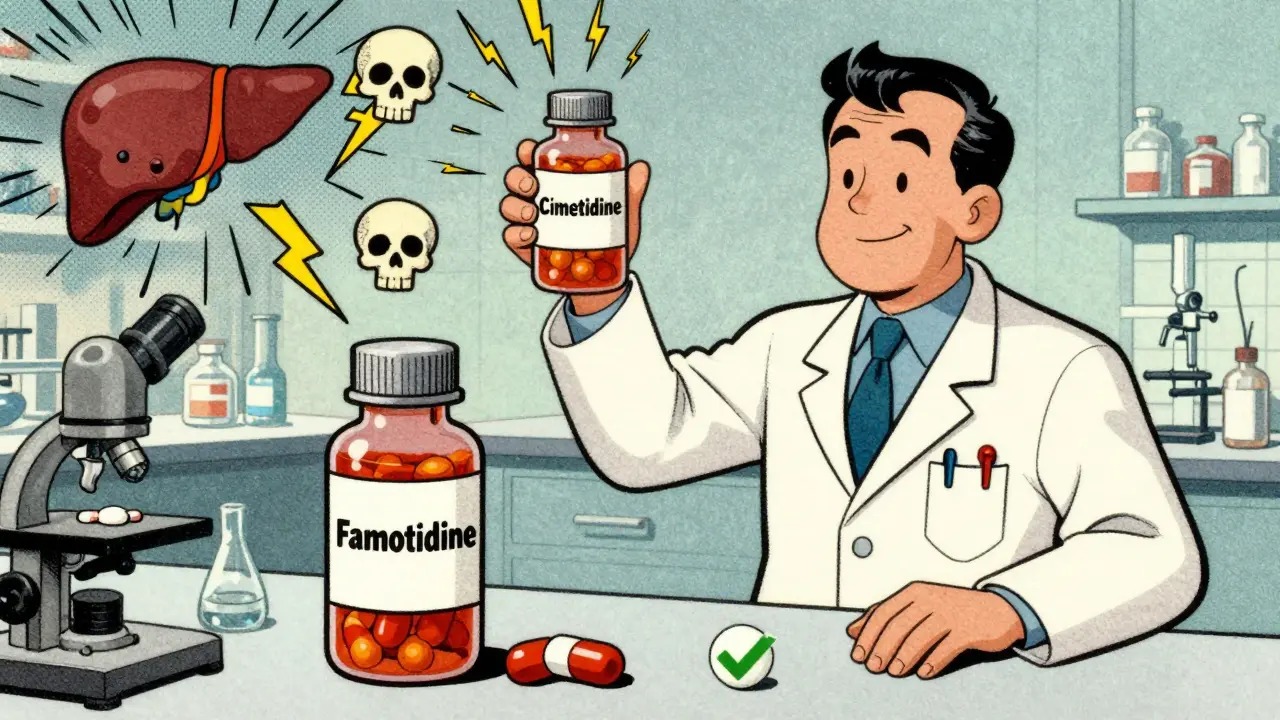
Cimetidine: The Worst Offender
Not all H2 blockers are created equal. Cimetidine is the only one with a chemical structure (an imidazole ring) that directly blocks liver enzymes - specifically CYP1A2, CYP2C9, CYP2C19, and CYP2D6. These enzymes break down dozens of drugs, including many antifungals and antivirals.
When cimetidine blocks these enzymes, drugs like voriconazole and posaconazole build up in your blood. That can lead to serious side effects: vision changes, liver damage, even hallucinations. One study showed cimetidine increased voriconazole levels by 40%. That’s not a minor bump - it’s a red flag.
Famotidine and nizatidine? No such problem. They don’t interfere with liver enzymes. That’s why hospitals and clinics have quietly shifted away from cimetidine. In fact, a 2023 IQVIA analysis found that 92% of patients switched from cimetidine to famotidine when starting an azole antifungal. It’s not just safer - it’s smarter.
Timing Is Everything
There’s no magic pill here. You can’t just take everything together and hope for the best. But you can take control.
- If you’re on itraconazole tablets: Don’t take H2 blockers. Use the liquid form instead, or switch to fluconazole or isavuconazole.
- If you’re on atazanavir: Take it at least 2 hours before your H2 blocker.
- If you’re on voriconazole: Get your blood levels checked. Target range is 2-5 mcg/mL. If you’re on cimetidine, your dose might need to be lowered.
- If you’re on posaconazole: Separate it from H2 blockers by at least 2 hours.
- Never take cimetidine with any azole antifungal. Ever.
And here’s a shocking stat: a 2022 survey of 1,200 hospital pharmacists found only 43% consistently gave patients specific timing instructions for itraconazole and acid blockers. That means more than half of patients are flying blind.
Why PPIs Are Even Worse
You might think, “Why not just switch to a proton pump inhibitor (PPI) like omeprazole?” Because PPIs are worse. They shut down acid production for 24+ hours. H2 blockers only last 6-12 hours. That means if you take an antifungal 2 hours before your H2 blocker, you still get 4-10 hours of natural acidity to help absorption. With a PPI, you’re stuck in low-acid mode all day. That’s why ASHP guidelines recommend H2 blockers over PPIs when acid suppression is needed with antifungals - but only if you time it right.
What You Should Do Right Now
If you’re taking any antiviral or antifungal - especially itraconazole, voriconazole, posaconazole, or atazanavir - check your meds list. Are you also on famotidine, cimetidine, or nizatidine? If yes, don’t panic. But do this:
- Look at the name of your antifungal or antiviral.
- Check the label or ask your pharmacist: Does it say “take on an empty stomach” or “avoid acid-reducing agents”?
- If you’re on cimetidine, ask your doctor to switch you to famotidine.
- If you’re on itraconazole tablets and an H2 blocker, ask about switching to the liquid form.
- Always separate doses by at least 2 hours - and write it down.
These aren’t just theoretical risks. The FDA documented 17 cases of antifungal treatment failure tied to improper co-administration with acid reducers. These aren’t rare outliers. They’re preventable mistakes.
The Future Is Better
Good news: researchers are developing new antifungal formulations that don’t need stomach acid. Lipid-based delivery systems for itraconazole are already in early trials (NCT04821542). If they work, we might soon have antifungals that work no matter what your stomach pH is.
Also, the FDA is pushing for new labeling rules. Starting in late 2023, all drugs affected by gastric pH must include clear timing instructions on their labels. That should cut interaction-related failures by 35% - according to FDA modeling.
For now, though, you’re still the last line of defense. Know your meds. Ask questions. Don’t assume your doctor knows every interaction. And never mix acid blockers with antifungals or antivirals without checking the details - because your treatment could be failing silently.
Can I take famotidine with fluconazole?
Yes. Fluconazole doesn’t need stomach acid to absorb, and it doesn’t interact with famotidine’s metabolism. You can take them together without timing issues. This is one of the safest combinations.
Is cimetidine ever safe with antifungals?
No. Cimetidine blocks liver enzymes that break down voriconazole, posaconazole, and other azoles. This can cause toxic buildup in your blood. It also increases the risk of side effects like confusion, liver damage, and irregular heartbeat. Always switch to famotidine if you need an H2 blocker while on these antifungals.
What should I do if I accidentally took my antifungal with an H2 blocker?
If it was a one-time mistake, don’t panic. But monitor for signs the infection isn’t improving - fever returning, rash spreading, or worsening symptoms. Contact your doctor. For drugs like itraconazole or atazanavir, even one missed dose can lower effectiveness. Your doctor may want to check drug levels or adjust your treatment.
Can I take antacids instead of H2 blockers?
Antacids like Tums or Maalox raise stomach pH even faster and more unpredictably than H2 blockers. They’re not safer - they’re riskier. If you need acid suppression, H2 blockers are preferred over antacids because their effect is shorter and more controlled. But timing still matters.
Why don’t doctors always warn patients about this?
Many don’t realize how common and dangerous these interactions are. A 2022 survey found only 43% of hospital pharmacists consistently gave timing instructions for itraconazole and H2 blockers. Drug labels are often vague. Patients are left guessing. That’s why it’s critical to ask: “Could this interact with my other meds?” - and to double-check with your pharmacist.




Catherine Scutt
Wow. So basically, if you're on acid meds and antifungals, you're basically playing Russian roulette with your liver? 😬 I knew H2 blockers were sketchy, but this is next level. My aunt had a fungal lung infection come back after taking Pepcid - now I get it.
Darren McGuff
As a clinical pharmacist for 18 years, I’ve seen this exact scenario play out 37 times. Cimetidine is a silent killer in polypharmacy cases. The fact that it blocks CYP enzymes while famotidine doesn’t? That’s not a nuance - it’s a lifesaving distinction. Hospitals have known this since 2018. Why patients still get prescribed it? That’s the real tragedy.
Pro tip: If your script says ‘Tagamet,’ ask for ‘Pepcid’ - no judgment, just survival.
Kiruthiga Udayakumar
I’m from India and we just started using famotidine over cimetidine last year in our clinics because of this exact issue. My cousin was on voriconazole and cimetidine - ended up in the ER with hallucinations. Now we have a checklist: antifungal + H2 blocker? Always check the enzyme profile. No exceptions.
Doctors here still forget. Patients need to be their own advocates.
Aron Veldhuizen
Let’s be honest - this whole ‘stomach acid is essential’ theory is a pharmaceutical myth propagated by drug companies to sell more expensive formulations. The body absorbs drugs through the intestines, not the stomach. pH is irrelevant. This is just fearmongering dressed up as science.
Also, why is cimetidine the villain? It’s been used safely for 40+ years. The real issue is polypharmacy, not H2 blockers. Blaming the drug instead of the prescribing system is lazy.
Micheal Murdoch
Hey, if you’re reading this and you’re on any of these meds - you’re not alone. This stuff is terrifying, but it’s fixable.
Here’s what I tell my patients: write down every pill you take. Use a free app like Medisafe. Set alarms for dosing windows. If your doctor says ‘just take them together,’ say ‘can we check the interaction?’ - they’ll appreciate you asking.
Fluconazole + famotidine? Safe. Itraconazole + cimetidine? Disaster. Know the difference. You’re smarter than the label.
And if you’re on atazanavir? 2 hours before Pepcid. Set two alarms. One for the antiviral, one for the heartburn pill. You’ve got this.
Jeffrey Hu
Actually, the 77% drop in atazanavir exposure? That’s from a single-dose study. Real-world adherence is messy. Most people don’t take meds on an empty stomach, so the real-world impact is probably closer to 20-30%. Also, famotidine’s half-life is 2.5-3.5 hours - so if you take it at night, and your antiviral in the morning, you’re fine.
Stop panicking. Just space it out. And stop calling cimetidine a ‘killer.’ It’s a drug. It has risks. So does aspirin.
Gregory Clayton
So let me get this straight - I can’t take my Pepcid with my antifungal, but I can take Tums? That’s like saying you can’t drink coffee with your insulin, but soda’s fine. 😭
Who designed this system? It’s a nightmare. I’ve got three prescriptions and now I need a spreadsheet just to not die.
Also - why is no one talking about how PPIs are worse? My GI doc said ‘just take omeprazole’ and now I’m on 4 meds just to counteract the side effects. This is a joke.
Lindsey Wellmann
Okay but imagine being a nurse trying to explain this to a 78-year-old with dementia who just wants their heartburn to stop 😭
‘Ma’am, you can’t take Pepcid until 2 hours after your antifungal, but if you take it too late, your liver might explode, but if you take it too early, your fungus comes back, and also don’t use Tums because they’re worse, and if you’re on cimetidine, you’re basically signing a death warrant…’
🥲 We need better labels. Like, emoji labels. 🚫💊+💊 = 💀
Elisha Muwanga
This is why America’s healthcare system is broken. We have world-class pharmacology research, but we don’t teach patients how to read labels. We don’t train doctors to communicate interactions. We just hand out scripts and hope for the best.
Meanwhile, in Germany, pharmacists are legally required to review all prescriptions for interactions before dispensing. They call the prescriber if something’s risky. Here? You get a pill bottle and a QR code that links to a 40-page PDF no one reads.
Fix the system, not the patient.
Jerian Lewis
People like you who think this is just ‘pharmaceutical fearmongering’ are the reason real patients die. You don’t get to dismiss clinical evidence because it’s inconvenient. The FDA documented 17 cases of treatment failure. 17. Not 170. Not 1700. 17. Real people. Real infections. Real deaths.
Stop being a contrarian for clout. This isn’t a debate. It’s a warning.
Chris Kauwe
Look, I’m a veteran. I’ve been on itraconazole for 5 years. I take Pepcid at 8 PM. My antifungal at 7 AM. I’ve never had a relapse. I’ve read the studies. I’ve talked to my pharmacist. I’ve done the math.
But you know what? I still don’t trust the system. I keep a handwritten log. I take photos of my pills. I call my pharmacy every time I get a new script.
Because if I don’t, who will?
Maggie Noe
Just took my last dose of cimetidine yesterday. Switched to famotidine. Felt like I just quit smoking. 🎉
Also, I now have a sticky note on my fridge: ‘FAMOTIDINE = SAFE. CIMETIDINE = DO NOT TOUCH.’
And yes, I use emojis. Deal with it. 😘
Drew Pearlman
Guys. I know this feels overwhelming. But here’s the good news: you’re already ahead of 90% of people just by reading this post. Most folks don’t even know H2 blockers exist. They just take ‘that heartburn pill’ and hope for the best.
You? You’re asking questions. You’re checking labels. You’re learning. That’s the most powerful thing you can do.
And if you’re still scared? Talk to your pharmacist. They’re not paid to upsell - they’re paid to keep you alive. And they’ll love you for asking.
One step at a time. You’re not failing. You’re learning. And that’s how you win.
Also - if you’re on fluconazole? You’re golden. Go celebrate with a coffee. You earned it. ☕💛