When your heart skips a beat or races faster than a sprint, you’re probably feeling the effects of a heart rhythm disorder. These disturbances range from harmless hiccups to life‑threatening emergencies. This guide walks you through every major type, how they show up, and what you can do about them.
Quick Takeaways
- Arrhythmias are any abnormal heart rhythms; they can be too fast, too slow, or irregular.
- Atrial fibrillation is the most common chronic arrhythmia and raises stroke risk.
- Ventricular tachycardia and ventricular fibrillation are medical emergencies.
- Bradycardia often stems from aging or medication but may need a pacemaker.
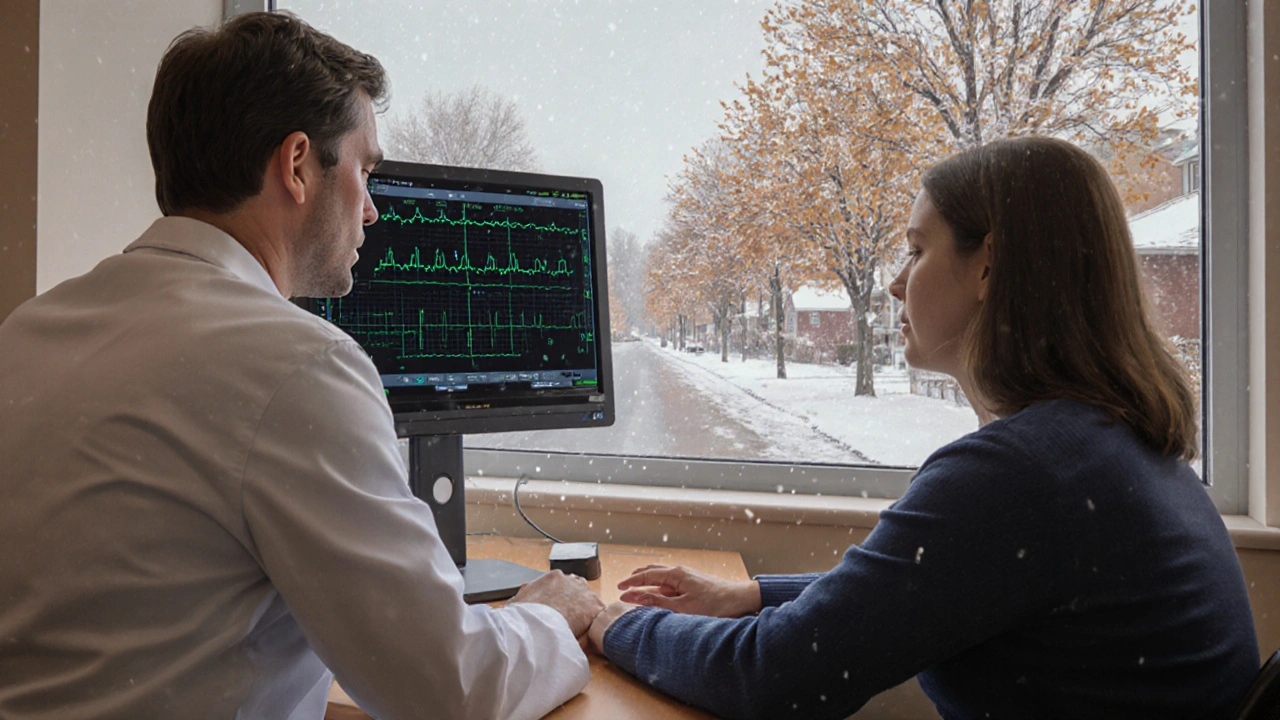
- Diagnosis relies on an Electrocardiogram (ECG) - a quick, painless test that records the heart’s electrical activity.
What Exactly Is an Arrhythmia?
Heart Rhythm Disorderscover any condition where the heart’s electrical system misfires, causing beats that are too fast, too slow, or irregular. In everyday language we call them arrhythmiasa broad umbrella term for abnormal heart rhythms. The heart’s natural pacemaker - the sino‑atrial node - sends out steady signals. When that signal is disrupted, the heart can’t pump efficiently, leading to symptoms like palpitations, dizziness, or shortness of breath.
Major Types of Heart Rhythm Disorders
Below are the most frequently encountered arrhythmias, each with its own pattern and risk level.
Atrial Fibrillation (AFib)
Atrial Fibrillationis an irregular, often rapid heart rhythm originating in the atria, causing blood to pool and increasing stroke risk. It accounts for roughly 1‑2% of the adult population and climbs to 10% in people over 80. Common triggers include high blood pressure, sleep apnea, and excessive alcohol.
Ventricular Tachycardia (VT)
Ventricular Tachycardiais a fast heart rhythm that starts in the ventricles, often a precursor to ventricular fibrillation. Heart rates usually sit between 150‑250bpm. If untreated, VT can quickly devolve into cardiac arrest.
Bradycardia
Bradycardiais a slow heart rate, typically fewer than 60 beats per minute, that may cause fatigue or fainting. It often stems from aging, hypothyroidism, or beta‑blocker therapy. In severe cases, a pacemaker becomes necessary.
Supraventricular Tachycardia (SVT)
Supraventricular Tachycardiacovers a group of fast rhythms that begin above the ventricles, commonly causing sudden palpitations. Episodes can start and stop within seconds, making them startling but usually not fatal.
Premature Ventricular Contractions (PVCs)
Premature Ventricular Contractionsare early beats that arise from the ventricles, often felt as a skipped heartbeat. Isolated PVCs are common and benign, but frequent PVCs may indicate underlying heart disease.
Heart Block
Heart Blockdescribes delayed or blocked electrical signals between the atria and ventricles, classified as first, second, or third degree. Third‑degree (complete) block almost always requires a permanent pacemaker.
Long QT Syndrome
Long QT Syndromeis a genetic condition that prolongs the heart’s repolarization period, raising the risk of torsades de pointes and sudden death. It can be triggered by certain medications or electrolyte imbalances.
How Doctors Diagnose Arrhythmias
The cornerstone test is the Electrocardiogramrecording, which captures the heart’s electrical pattern over a few seconds. Depending on the situation, clinicians may also use:
- Holter monitor - a 24‑48hour wearable ECG.
- Event recorder - patient‑activated device for infrequent episodes.
- Exercise stress test - reveals rhythm changes under exertion.
- Electrophysiology study - invasive mapping to pinpoint abnormal pathways.
Blood tests (electrolytes, thyroid function) help rule out reversible causes, while imaging (echocardiogram, cardiac MRI) assesses structural heart disease that can precipitate arrhythmias.

Treatment Options Across the Spectrum
Therapies match the severity and type of arrhythmia.
Medication
Anti‑arrhythmic drugs (e.g., amiodarone, flecainide) aim to stabilize the electrical system. Rate‑controlling agents (beta‑blockers, calcium channel blockers) are first‑line for AFib and SVT. Anticoagulants (warfarin, DOACs) reduce stroke risk in AFib.
Cardioversion
When a rhythm is fast but organized (like AFib), an electrical shock can reset the heart to normal. Chemical cardioversion uses drugs like ibutilide.
Catheter Ablation
Through a thin catheter, physicians deliver radiofrequency energy to destroy the tissue causing abnormal signals. Ablation success rates exceed 80% for AFib and over 90% for many SVT pathways.
Implantable Devices
Implantable Cardioverter Defibrillator(ICD) monitors heart rhythm and delivers a shock if a life‑threatening rhythm like ventricular tachycardia occurs. Pacemakers handle persistent bradycardia or complete heart block.
Lifestyle & Prevention
Simple changes can lower arrhythmia risk:
- Maintain a healthy weight - obesity raises AFib odds by 50%.
- Limit alcohol and caffeine - binge drinking can trigger AFib episodes.
- Manage stress - meditation reduces sympathetic spikes that provoke SVT.
- Stay active - regular aerobic exercise improves cardiac efficiency.
- Check medications - some antibiotics and antidepressants prolong the QT interval.
Comparison of Common Arrhythmias
| Type | Typical Rate (bpm) | Location of Origin | Urgency | First‑Line Treatment |
|---|---|---|---|---|
| Atrial Fibrillation | 100‑180 (irregular) | Atria | High - stroke risk | Rate control + anticoagulation |
| Ventricular Tachycardia | 150‑250 | Ventricles | Critical - can progress to VF | ICD or urgent cardioversion |
| Bradycardia | <60 | Sino‑atrial node | Variable - symptoms dictate | Pacing if symptomatic |
| Supraventricular Tachycardia | 150‑250 (regular) | Atrioventricular node | Usually non‑life‑threatening | Vagal maneuvers → medications → ablation |
Quick Checklist for Patients
- Notice any new palpitations, dizziness, or fainting.
- Record how long episodes last and any triggers.
- Schedule an ECG if symptoms persist more than a few weeks.
- Discuss anticoagulation if diagnosed with AFib.
- Ask about lifestyle tweaks that could lower recurrence.
Frequently Asked Questions
Can stress really cause a heart rhythm disorder?
Yes. Stress spikes adrenaline, which can trigger SVT or even precipitate AFib in vulnerable individuals. Managing stress with breathing exercises or yoga often reduces episode frequency.
Is a pacemaker only for older adults?
No. While age‑related conduction disease is common, younger patients with congenital heart block or post‑surgical AV node damage also receive pacemakers.
What’s the difference between VT and VF?
Ventricular tachycardia (VT) is a fast, regular rhythm that can still produce some blood flow. Ventricular fibrillation (VF) is chaotic, no organized pumping, and leads to cardiac arrest within seconds if not shocked.
Do PVCs need treatment?
Isolated PVCs are usually harmless. However, if they occur frequent (>10% of beats) or cause symptoms, doctors may investigate underlying disease or consider medication.
How often should someone with AFib get an ECG?
After the initial diagnosis, routine ECGs are done at each cardiology visit (often every 6‑12months) or sooner if symptoms change.

Kasey Krug
The overview is thorough, yet it glosses over the practical nuances of managing atrial fibrillation in everyday patients. A brief mention of rate control is insufficient without discussing beta‑blocker titration protocols. Moreover, the section on lifestyle changes feels like a checklist rather than actionable advice. Overall, the article could benefit from deeper clinical insight.
jake cole
Honestly, this reads like a watered‑down textbook for high‑school biology. The author throws around jargon without explaining why it matters to a layperson. Minimal research effort is evident; the piece rehashes Wikipedia verbatim. It’s an insult to anyone seeking real, applicable guidance.
Natalie Goldswain
Thx for the summary.
Abhishek Vora
PVCs are often dismissed as harmless, yet their frequency can betray underlying myocardial irritation. When premature beats exceed ten percent of total rhythms, clinicians should investigate electrolyte imbalances. A dramatic surge in PVCs may hint at ischemia or structural heart disease. Moreover, patients reporting frequent ‘skipped beats’ deserve careful Holter monitoring. In practice, lifestyle factors such as caffeine excess can amplify PVC occurrence, so moderation is advisable.
maurice screti
One cannot help but marvel at the sophisticated symphony that is the cardiac conduction system, an orchestration of electrical impulses that, when perturbed, gives rise to the bewildering array of rhythmopathies detailed herein. The author commendably attempts to encapsulate the breadth of arrhythmic phenomena, yet the exposition suffers from an inadvertent truncation of nuance that would otherwise enrich the reader’s comprehension. For instance, the discussion of atrial fibrillation, while accurate in its enumeration of risk factors, omits the subtleties of substrate remodeling that underlie its progression from paroxysmal to persistent forms. Additionally, the treatment section, though comprehensive in listing therapeutic modalities, fails to differentiate the algorithmic decision‑making that dictates when one might favor catheter ablation over pharmacologic rate control. Consider the case of supraventricular tachycardia: the narrative mentions vagal maneuvers, yet neglects to elaborate on the physiological basis by which increased vagal tone prolongs AV nodal refractory periods. In the realm of ventricular arrhythmias, the juxtaposition of ventricular tachycardia and ventricular fibrillation is apt, yet the reader is left yearning for a more granular discussion of the electro‑mechanical dissociation that distinguishes the two. Moreover, the brief allusion to long QT syndrome could be expanded to include genotype‑phenotype correlations, a topic of paramount importance for clinicians navigating drug‑induced QT prolongation. The lifestyle recommendations, while well‑intentioned, border on the generic; a deeper analysis of how weight reduction quantitatively lowers atrial fibrillation burden would serve a discerning audience. Finally, the tabular comparison, though aesthetically pleasing, lacks a column for mortality risk, a metric that invariably guides therapeutic urgency. In sum, the piece stands as a solid foundation, but it beckons further elaboration to truly honor the complexity of cardiac electrophysiology.
Abigail Adams
While the ambition of the article is laudable, its execution leaves much to be desired from a scholarly perspective. The reliance on bullet points, though reader‑friendly, sacrifices depth that clinicians require for nuanced decision‑making. The section on anticoagulation, for example, fails to address the emerging role of left atrial appendage occlusion in patients contraindicated to DOACs. Furthermore, the omission of recent guideline updates on rhythm versus rate control strategies for atrial fibrillation is a notable oversight. A more rigorous citation of contemporary trials would elevate the credibility of the content.
Belle Koschier
I appreciate the inclusive tone of the guide and the effort to demystify complex concepts for a broad audience. The balanced presentation of both pharmacologic and procedural options reflects a patient‑centered approach. Emphasizing lifestyle modifications alongside medical therapy resonates well with holistic care principles. Overall, the article serves as a useful entry point for individuals seeking to understand their condition.
Allison Song
From a philosophical standpoint, the heart’s rhythm can be viewed as a metaphor for life's unpredictable tempo. The article reminds us that even the most orderly systems are subject to chaotic interludes, much like our personal journeys. Recognizing the interplay between determinism (genetic predisposition) and free will (lifestyle choices) offers a richer appreciation of arrhythmia management. In contemplating these dualities, we honor both science and the human experience.
Joseph Bowman
It’s interesting how the medical community emphasizes monitoring while seemingly ignoring the subtle influences of environmental electromagnetic fields. Some researchers argue that pervasive Wi‑Fi signals could subtly modulate cardiac electrophysiology, an angle often omitted from mainstream discourse. While definitive proof remains elusive, the possibility invites a cautious re‑examination of our daily exposure. Maintaining a skeptical yet open mind ensures we remain vigilant about hidden factors that might affect heart health.
Singh Bhinder
Additional insight reveals that certain over‑the‑counter cold medications contain decongestants known to prolong QT intervals. Patients on existing anti‑arrhythmic drugs should be particularly vigilant when self‑medicating for common ailments. Moreover, electrolyte disturbances, especially hypokalemia, can exacerbate ventricular ectopy, underscoring the importance of routine lab monitoring. Integrating these considerations into patient education can prevent inadvertent arrhythmic triggers.
Kelly Diglio
I commend the comprehensive nature of the piece and would like to add that clear communication between physician and patient is paramount when discussing treatment options. Explaining the risks and benefits of anticoagulation in plain language can empower patients to adhere to therapy. It is also beneficial to provide written summaries of lifestyle recommendations for future reference. Thank you for assembling such an informative resource.