Walk into almost any pharmacy in Seattle or check your older relatives’ medication lists and you’ll spot an old friend: Lipitor. It’s not just a household name; it’s the best-selling pharmaceutical ever, racking up sales that once outdid Nike and Coca-Cola. Curious why every cardiologist seems quick to recommend it, and what it really does to your body? You’ll hear a lot of chatter—some swear by it, others worry it causes more problems than it solves. But what’s hype, what’s legit science, and what’s just leftover urban legend from chain emails your parents used to forward? Let’s break through the maze and look at Lipitor under the microscope, all the way from its invention to the little annoyances it can bring to your daily life.
How Lipitor Really Works: Under the Hood of Cholesterol Control
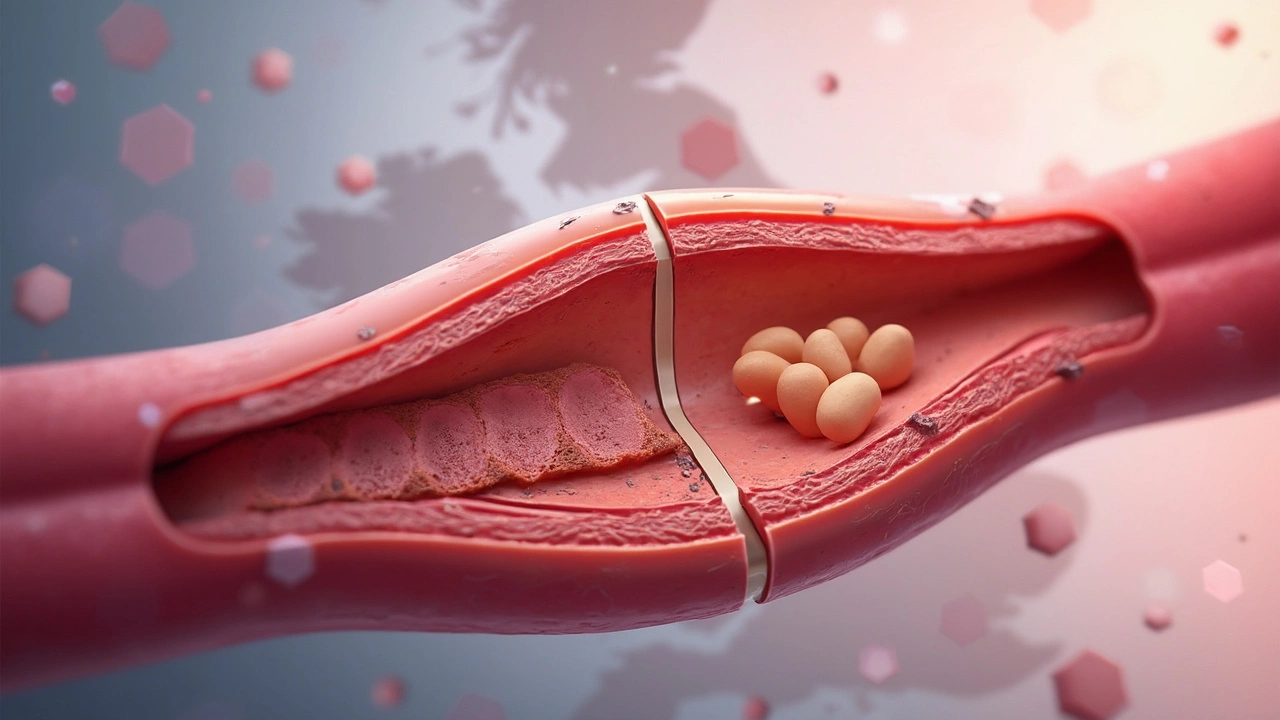
Grab a greasy burger or a crisp salad, and cholesterol follows. It’s not the villain it’s made out to be—your body needs some cholesterol to make hormones and keep cells happy. But too much of the wrong kind and your arteries clog up like old pipes. This is where Lipitor (generic name: atorvastatin) steps in like a professional plumber. It belongs to a group of drugs called statins, which have one main job: stop your liver from making excess cholesterol. Specifically, Lipitor blocks an enzyme called HMG-CoA reductase—a kind of foreman on your liver’s cholesterol assembly line. With Lipitor on the scene, the factory slows down, and the LDL or ‘bad’ cholesterol drops. At the same time, Lipitor gives a nudge to your liver to clear out more cholesterol already floating around in your blood.
You probably know someone who’s been prescribed Lipitor after a routine check-up spotted a high LDL. But there are concrete stats behind the prescription pad. Back in the late '90s, the ASCOT-LLA study tracked more than 10,000 people at risk for heart problems. Lipitor lowered their risk of a major heart event by about 36%. And according to the American Heart Association, if you start Lipitor after a heart attack, you cut your chances of a second by up to a third. Those numbers are the reason doctors keep writing that script.
Lipitor doesn’t just lower cholesterol; it also cuts inflammation in your blood vessels, reducing plaque buildup. But don’t expect it to bail you out from daily cheeseburgers—Lipitor works best alongside some mild diet changes and, yeah, the occasional walk that actually breaks a sweat.
Real-Life Lipitor: Side Effects No One Warns You About
The power of Lipitor isn’t magic, and there’s a cost—side effects. While most folks don’t notice a thing, a chunk of users report muscle aches. Not just a post-gym soreness, but a stubborn ache, usually in the thighs or shoulders. It’s called myalgia, and it can happen within weeks of starting Lipitor. The actual numbers? Roughly one in ten people notice mild aches, and less than 1% get hit with serious muscle damage (rhabdomyolysis is the heavy hitter here, but it’s very rare).
Other annoyances on the list include mild headaches, stomach upsets, and the mysterious feeling like your memory is playing tricks on you. The FDA did look into the statin-memory question in 2012. The verdict? Any brain fog seems short-lived and disappears if you stop Lipitor. Still, if you notice weirdness, mention it.
Some people worry about liver damage. Doctors do check your liver enzymes before and during Lipitor—because, for about 1–3% of users, liver numbers can spike. Usually, it’s reversible, and sometimes your body just needs a lower dose.
If you have diabetes or are hanging out on the borderline, statins like Lipitor might push your blood sugar up a notch. A study in JAMA (2012) tracked thousands of people and found a tiny increase in new diabetes cases—about 1 in every 250 people on Lipitor for four years. The heart benefits usually win out, but it's worth knowing if you're already watching your glucose.
Making the Most of Lipitor: Tips and Tricks from Real Users
You’ve got the bottle in your hand, but how do you make Lipitor work for you—and not against you? First off, stick with a consistent schedule. Taking your pill at the same time each evening helps your body keep levels steady—and that’s when your liver likes to pump out cholesterol anyway. No need to fast, but try to pair it with a routine (like brushing your teeth).
If you’re taking other meds, let your doctor know. Grapefruit and Lipitor don’t mix—they can raise the drug’s level in your blood and boost side effects. Even a daily glass of grapefruit juice can make a difference.
Track your own side effects. Write down any weird muscle pains, stomach troubles, or changes in mood or sleep, and bring your list to your doctor. Docs aren’t mind-readers, and most side effects are dose-related. Sometimes, just lowering your dose or switching statins does the trick.
- Hydrate. People who drink more water report fewer muscle aches.
- Try magnesium. Some folks with mild muscle pain say it helps. Ask your doc before adding a supplement to your mix.
- If you forget a dose, just take the next one when you remember, but don't double up.
- Plan for regular blood tests—usually every 3–6 months to track your cholesterol and liver function. Skipping these is a gamble.
And here’s something wild: A lot of people who start Lipitor are hoping to quit it quickly, but studies show that staying on statins long-term is what prevents heart attacks. Think marathon, not sprint. But if you’re struggling, you aren’t locked in for life—be open with your doc about wanting changes.
Lipitor by the Numbers: Stats and What They Really Mean
Nothing cuts through confusion like some hard numbers. So just how common is Lipitor, and what’s its real impact? Check out this quick table for the essentials:
| Category | Lipitor Data |
|---|---|
| First FDA Approval | 1996 |
| Total Prescriptions (U.S., 2023) | Over 90 million |
| Typical LDL Reduction | 35%–60% (depends on dose) |
| Risk Reduction (Heart Attack) | About 36% |
| Most Common Side Effect | Muscle aches (up to 10%) |
| Serious Muscle Damage | Less than 1% |
| Cost (Generic) | $3–$15/month with insurance |
See that LDL drop? People used to wait for these sorts of results from major diet changes alone. Now, Lipitor rewrote the playbook. And while the market is flooded with generics (atorvastatin), it’s still a blockbuster. The best part: costs have plummeted from $100/month in the early 2000s to just a few bucks at most U.S. pharmacies now.
The global reach is massive—Lipitor has been prescribed over a billion times worldwide. The world’s trust in this drug isn’t an accident—it’s built on trials like the TNT study (2005), which showed aggressive LDL lowering with Lipitor sharply cut cardiac events, even compared to older statins. Researchers keep tracking people year after year to be sure benefits stick around, and so far Lipitor keeps earning its keep.

Common Myths, Misunderstandings, and What the Science Actually Says
If you search social media, you’ll see a lot of wild claims about statins. Some insist that Lipitor causes memory loss or makes you tired all the time. The reality? Brain fog happens in a minority, but it’s usually reversible. Large studies show no sign that statins lead to dementia. Others say statins zap your energy. About 2%-5% of people might feel a drop in pep, but for most, lifestyle factors matter way more.
Then there’s the worry that Lipitor ruins your muscles. Severe muscle issues are rare. The most at-risk groups? People over 70, those with kidney trouble, or who mix statins with certain other meds (like gemfibrozil or antifungals). If you’re younger and healthy, your risk is low. But stay alert to unexplained pain—your doctor can check a CK enzyme level to be sure.
Another myth: “Once on Lipitor, always on Lipitor.” Not true. If you make major changes—losing weight, cutting saturated fats, picking up real exercise—some people can step down on their dose or even switch to non-statin options. But remember, most adults don’t stick with lifestyle changes forever, which is why statins like Lipitor are the safety net for so many.
Ever heard someone say Lipitor is just a cash grab? The patent did rake in $125 billion for Pfizer, but the evidence base is real. Independent researchers and doctors across the world have done randomized controlled studies—these aren’t just pharma-driven numbers. Real patients, real impact.
- Tip: If you’re the skeptical type, ask for a 'calcium score' coronary scan. Higher scores mean more risk, and show whether you need powerful cholesterol-lowering at all.
- Don’t take blanket advice from celebrities or folks pushing “natural” alternatives. Some supplements—like red yeast rice—actually contain a statin, just unregulated and less predictable.
Last thing: Statins, including lipitor, aren’t quick fixes for a lifetime of greasy meals. But for people with sky-high cholesterol (LDL over 190mg/dL) or a history of heart attacks, they lower the odds of heart trouble in a way nothing else matches right now. Stay curious, stay critical, and always keep your doc in the loop about side effects and goals.


Damon Farnham
Honestly, I've always been skeptical about Lipitor — like, why does everyone just blindly pop these pills without questioning the big pharma machine behind it??? This article is refreshing because it goes beyond the superficial and actually lays down scientific pros and cons. I mean, yes, it lowers cholesterol but at what cost? Side effects are often downplayed or ignored. The truth is people deserve a clearer picture, not just a sales pitch disguised as medical advice!!!
And don't get me started on the hype, it feels like a cult sometimes, everyone praising it like it’s some miracle drug. No mention about the real long-term consequences or alternatives. So yeah, I appreciate the honesty here—finally a guide that does not sugarcoat stuff.
Marsha Saminathan
Oh my goodness, this piece really got me thinking!! It’s like peeling back the glamorized curtain around Lipitor’s fame. You wouldn’t believe the myriad of biochemical tango that this drug performs inside us—truly fascinating and a tad overwhelming. But the real gem here is how it candidly addresses the side effects many are too scared to talk about openly.
I’ve encouraged several of my friends and family who were on statins to read this because knowing what you’re truly putting into your body is empowerment in its purest form. It’s not just cold dosage—it’s your life and vitality at stake!! So, to anyone hesitating, equip yourself comprehensively before making decisions!
Justin Park
Reading through this article, it strikes me how much of our health decisions are influenced by a complex interplay of medical advice, pharmaceutical interests, and personal experience. Lipitor’s continuing dominance in prescriptions clearly indicates its effectiveness, but the nuanced risks can’t be dismissed.
Does anyone else wonder about the philosophical angle of relying so heavily on medication for something like cholesterol, which sometimes can be managed through lifestyle? It raises deeper questions about modern health paradigms and how much we entrust our well-being to scientific interventions versus natural methods. I’d love to hear your thoughts on this tension!
🙂Herman Rochelle
This article is a solid resource for anyone navigating the confusing landscape of cholesterol medications. What I appreciate most is the balanced presentation of Lipitor’s benefits and real side effects. Serious about health means getting informed beyond the ads.
For those concerned about side effects, it’s important to discuss them openly with your healthcare provider — sometimes adjustments can help mitigate those while still gaining the protective benefits. Stay vigilant and proactive about understanding your options!!
Stanley Platt
It is intellectually stimulating to observe the extensive scientific discourse surrounding Lipitor's efficacy juxtaposed with its adverse effects. The article's systematic exploration provides clarity often obfuscated by pharmaceutical marketing strategies. Such transparency is indispensable for patients striving to make informed decisions grounded in evidence.
Furthermore, it is imperative to acknowledge the heterogeneous patient responses, which necessitate personalized discussions with healthcare professionals. The ethical stewardship of prescribing these statins must balance clinical benefit with patient well-being, a topic this article commendably elucidates.
Alice Settineri
Wow, I can't even begin to tell you how many conversations I've overheard at family dinners about how 'miracle' Lipitor is. But the colorful truth is much juicier, right? This article totally peels back the layers beyond that sterile pharma gloss—it's like Lipitor’s real story, unfiltered.
If you're on statins or thinking about it, you owe it to yourself to dig deep like this! Side effects aren’t just minor nuisances, sometimes they hit hard. But knowing that gives you power to catch those warning signs early or to push for alternative options. Seriously, knowledge is your best vibrantly protective shield.
nathaniel stewart
Good read indeed. From what I've seen, Lipitor has saved countless lives by preventing heart attacks and strokes due to high cholesterol. However, sometimes the side effects can be tricky and might discourage some patients. I always suggest consulting your doc about any discomfort because sometimes dosage tweaks make a big difference.
It's great that the article highlights both sides instead of just hyping the positives. Being positive about treatment outcomes while realistic about challenges helps keep expectations grounded. Keep spreading the info that matters!
Pathan Jahidkhan
Lipitor. The much praised knight of cholesterol battlefields. But… is it truly the hero? Or just a well-scripted propaganda piece orchestrated by capitalist markets? This article barely scratches the abyssal depths of such inquiry. Side effects mentioned are the tip of the iceberg, a theatrical distraction from systemic pharmaceutical dominance.
One must question—are we treating symptoms or sedating societal health anxieties? Cholesterol, a misunderstood specter, often demonized to justify endless prescriptions. A dramatic saga of modern medicine indeed. I remain cautious, watching the unfolding pharma theater with a skeptic’s eye.
Dustin Hardage
This article provides a commendable examination of Lipitor’s role in managing cholesterol yet also diligently surveys potential adverse reactions. It is crucial for patients to appreciate that while the drug has transformative benefits, vigilance regarding muscular symptoms, liver enzyme elevations, or cognitive effects is warranted.
Moreover, literature supports lipid-lowering efficacy as a primary therapeutic objective in cardiovascular risk reduction. Thus, a synergistic approach, integrating lifestyle modifications and medication where indicated, offers the optimal strategy for patient outcomes.
Dawson Turcott
LOL, so now Lipitor is this colossal wonder drug, right? But hey, gotta ask: if it’s so perfect, why do we hear horror stories about side effects? Muscle pain, brain fog? Seems like every ‘miracle’ drug is just a double-edged sword wrapped in a fancy little pill. Not knocking it entirely, but this article kind of pulls the wool off the eyes.
Still, I wonder — are the side effects really that bad for everyone, or just a loud minority? Anyone here actually used Lipitor and lived to tell the tale without the drama? Spill the tea!
🤔Katheryn Cochrane
This article attempts to unravel the layered reality surrounding Lipitor but still sounds very tentative about some of the more insidious risks. Serious side effects are often underreported or minimized in clinical settings, and patients end up becoming mere data points in profit-driven models.
While it is important to acknowledge lifesaving benefits, we must remain vigilant about the disproportionately aggressive marketing tactics. People deserve exhaustive transparency, not half-hearted disclosures. In my experience, a lot more caution and personal research is warranted before obliging to statin therapy without question.