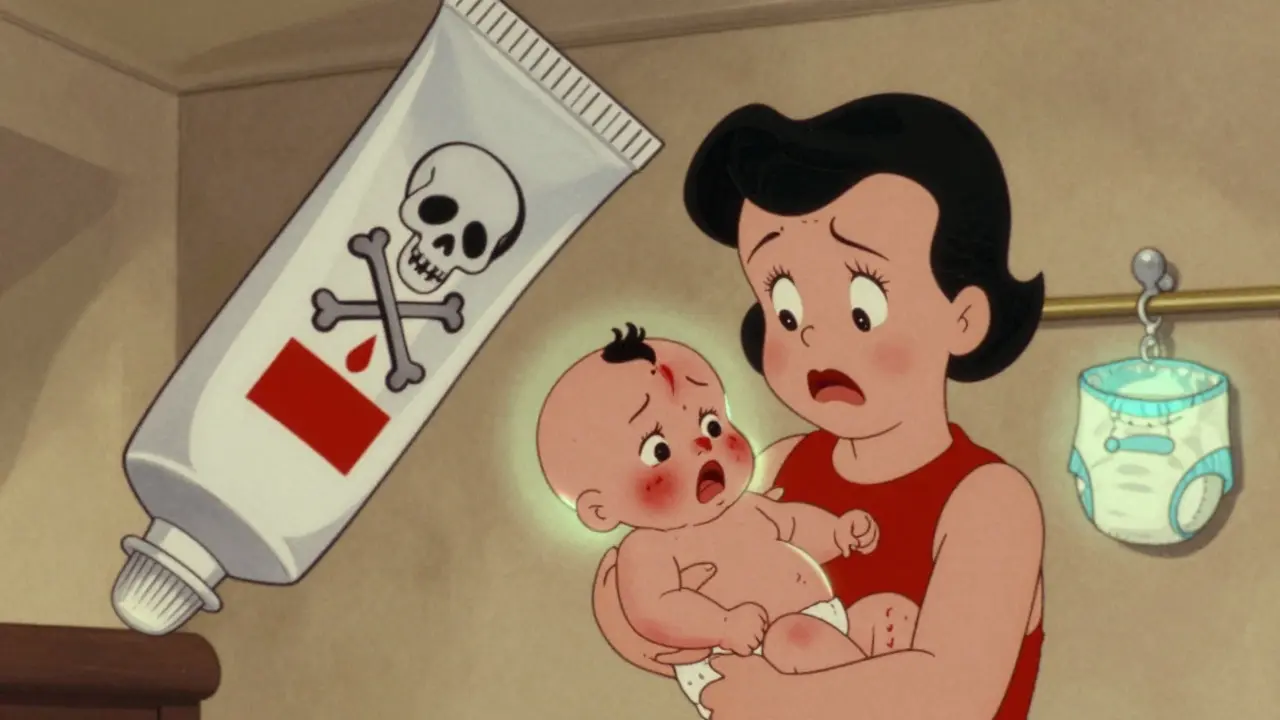
Every parent knows the panic when a baby’s skin turns red, itchy, or sore. You reach for the cream in the cabinet - maybe the one your neighbor swore by, or the leftover tube from last year’s eczema flare-up. But what you think is a quick fix could be risking your child’s health. Topical medications for children aren’t just weaker versions of adult products. They’re a different world entirely - and getting them wrong can lead to serious, even life-threatening, side effects.
Why Children’s Skin Is Different
Children’s skin isn’t just smaller. It’s thinner, more porous, and still developing. Babies under one year old have skin that absorbs topical medicines 3 to 5 times more easily than adults. That’s not a small difference - it’s a medical red flag. The outer layer of their skin, called the stratum corneum, hasn’t fully formed yet. That means creams, gels, and ointments don’t just sit on top. They sink in - fast.And it gets worse if the skin is broken. Eczema, diaper rash, or even a small scratch can turn absorption rates from 3% to over 60%. That’s why applying a strong steroid cream to a patch of inflamed skin isn’t just risky - it’s dangerous. One study showed that a child with widespread eczema absorbing a potent steroid through damaged skin could end up with the same hormonal suppression as someone taking oral prednisone.
What You Should Never Use on Babies
There are three topical products that should stay off your child’s skin until they’re older - and even then, only with a doctor’s direction.- Benzocaine - Found in teething gels, sore throat sprays, and some numbing creams. The FDA banned its use in children under 2 because it can cause methemoglobinemia - a condition where blood can’t carry oxygen properly. Babies can turn blue, struggle to breathe, and go into shock within minutes. There have been over 400 documented cases since 2006. Chilled rubber teethers work better and are completely safe.
- High-potency corticosteroids - Creams like clobetasol, betamethasone, or hydrocortisone 2.5% or higher carry black box warnings for children under 2. These can shut down the body’s natural stress hormone system (HPA axis), leading to fatigue, low blood sugar, and even adrenal crisis. Even a small amount applied over a large area can cause this.
- Dibucaine and lidocaine in large doses - Lidocaine is sometimes used for minor procedures, but only under strict control. Too much - especially with occlusion (plastic wrap or tight bandages) - can cause seizures. The safe limit for a child under 3 is 1.2 grams total in 24 hours. That’s about half a teaspoon. Most parents have no idea how much that is.
How Much Is Too Much? The Fingertip Unit Rule
Parents often use “a pea-sized amount” or “a dab.” Those terms mean nothing. A pea is not a standard unit. That’s why doctors use something called the fingertip unit (FTU).An FTU is the amount of cream squeezed from a standard tube (5mm opening) along the length of an adult’s index finger - from the tip to the first crease. That’s about 0.5 grams. One FTU covers an area of skin about the size of two adult palms.
For a 10kg (22-pound) child, the maximum daily dose of a low-potency steroid like hydrocortisone 1% should be no more than 2 grams total - that’s just four FTUs. Apply it to more than 10% of their body surface area, and you’re crossing into danger territory. Most parents apply way more than this - often because they think “more is better.” It’s not. It’s toxic.

When Occlusion Turns Deadly
You might’ve heard that wrapping a cream in plastic wrap helps it work better. That’s true - but only if you’re a doctor treating a severe condition under supervision. For kids, occlusion (using Tegaderm, Saran Wrap, or even a tight diaper) can increase absorption by 300-500%. That’s not an enhancement - it’s an overdose waiting to happen.One case from a pediatric hospital involved a mother who applied hydrocortisone 1% to her 8-month-old’s eczema and covered it with plastic wrap overnight. The child developed lethargy, poor feeding, and low blood pressure the next day. Blood tests showed adrenal suppression. She didn’t know plastic wrap was making the cream 5 times stronger.
Unless your pediatrician or dermatologist specifically tells you to occlude, don’t do it. Never use plastic wrap, tight bandages, or sealed diapers as a “moisturizing trick.”
Alternatives That Work - Without the Risk
You don’t need strong chemicals to treat common skin problems in children.- For eczema: Use fragrance-free moisturizers like CeraVe or Eucerin twice daily. If it’s not enough, topical calcineurin inhibitors like tacrolimus 0.03% (approved for kids 2+) or pimecrolimus (for 3+ months) are safer than steroids. They don’t suppress hormones. And after 15 years of use, there’s still no proven link to cancer - despite the FDA’s black box warning, which is based on theoretical risk, not real cases.
- For diaper rash: Zinc oxide paste works better than most medicated creams. Let the skin breathe. Change diapers often. Avoid wipes with alcohol or fragrance.
- For teething pain: A cold (not frozen) washcloth or silicone teether is the gold standard. No chemicals. No risk. No hospital visits.

Storage and Accidental Poisoning
The biggest risk isn’t misuse - it’s access. According to the American Association of Poison Control Centers, 78% of children under 5 who accidentally ingest topical medications do so because the product was left out after use. A parent applies cream, sets the tube down, and walks away. A toddler grabs it. Within minutes, they’ve swallowed a dangerous dose.That’s why child-resistant packaging matters. The CPSC required it for products with more than 0.5 mg of lidocaine or dibucaine back in 1994 - but enforcement is patchy. Many over-the-counter lidocaine gels still come in non-child-resistant tubes. Always check. Always store creams in a locked cabinet, not on the bathroom counter.
What to Do If Something Goes Wrong
If your child shows any of these signs after using a topical product:- Blue or gray skin (especially lips or fingernails)
- Unusual drowsiness or difficulty waking up
- Fast or shallow breathing
- Seizures or muscle twitching
Call 911 or go to the ER immediately. For benzocaine toxicity, the antidote is methylene blue - but it must be given intravenously in a hospital. Don’t wait. Don’t call poison control and wait for a callback. Time matters.
What’s Changing in 2026
The FDA is rolling out new labeling rules for all topical medications sold in the U.S. Starting in 2026, every tube or jar must clearly state:- Minimum age for use
- Maximum daily dose in grams
- Maximum body surface area allowed
- Duration limit (e.g., “Do not use longer than 7 days”)
Also, new formulations are coming. Nanoparticle-based creams are in late-stage trials and reduce absorption by up to 80% while keeping effectiveness. These could be game-changers for kids with chronic skin conditions.
But until then, the safest rule is simple: Use the weakest product that works. Apply the smallest amount possible. Never cover it. Keep it locked up. And when in doubt - skip it. Your child’s skin doesn’t need a chemical solution. It needs care, not control.
Can I use hydrocortisone cream on my 6-month-old?
Yes, but only hydrocortisone 0.5% or 1%, and only for a small area (like a few spots of eczema). Never use it on large areas or for more than 3-5 days in a row. Apply no more than 1-2 fingertip units per day. Avoid using it on the face unless your doctor says so. Stronger versions (2.5% or higher) are not safe for babies under 2.
Is benzocaine really that dangerous for teething?
Yes. Benzocaine can cause methemoglobinemia in babies, which stops oxygen from reaching the body’s tissues. Symptoms appear within 15-30 minutes: pale or blue skin, trouble breathing, confusion, fatigue. Even one application can trigger it. There are zero safe doses for children under 2. Chilled teething rings work just as well - and without any risk.
How do I know if I’m using too much cream?
Use the fingertip unit (FTU) method: squeeze a strip of cream from the tube along your index finger, from tip to first crease. That’s one FTU - enough to cover two adult palms. For a baby, one or two FTUs total per day is usually enough. If you’re using more than that, or applying it to more than 10% of their body (like both legs and back), you’re likely overdoing it.
Can I use my child’s eczema cream on myself?
Not unless your doctor says so. Pediatric creams are formulated to be weaker and safer for thin, sensitive skin. Using a child’s hydrocortisone 1% cream on your own eczema might not be strong enough. Conversely, using your adult-strength steroid on your child could cause serious side effects. Always use the product prescribed for the person it’s meant for.
What should I do if my child swallows some cream?
Call Poison Control at 1-800-222-1222 immediately - even if your child seems fine. Don’t wait for symptoms. If the cream contains lidocaine, dibucaine, or benzocaine, go to the ER right away. These can cause seizures or oxygen deprivation within minutes. Bring the tube with you so medical staff can identify the ingredients.






Alfred Schmidt
STOP. Just STOP. You think your neighbor’s ‘magic cream’ is safe? My cousin’s kid ended up in the ICU because someone slapped hydrocortisone 2.5% on a diaper rash and wrapped it in plastic wrap like it was a damn burrito. The kid went into adrenal crisis. No joke. No warning labels. Just a panicked mom and a tube labeled ‘for adults only’ sitting on the counter. This isn’t ‘be careful’-this is a public health disaster waiting to happen. And yes, I’m yelling. Because people still think ‘it’s just a cream.’ IT’S NOT.
Sam Davies
Oh, delightful. Another treatise on the perils of pediatric dermatology, written with the emotional precision of a WHO pamphlet. Truly, the pinnacle of modern parenting wisdom: ‘Use less.’ How revolutionary. Next, we’ll learn that fire is hot and water is wet. Also, ‘fingertip unit’? That’s not a unit-it’s a middle-class British doctor’s attempt to sound scientific while ignoring that most parents are just trying to get their kid to stop screaming at 3 a.m. with a cold washcloth and sheer desperation.
Christian Basel
There’s a pharmacokinetic disconnect here. Pediatric stratum corneum permeability is hyperallometric relative to body surface area-to-mass ratios, which explains why topical absorption escalates non-linearly in infants under 12mo. Add occlusion, and you’re looking at AUC saturation thresholds that exceed pediatric LD50 thresholds for corticosteroids. The real issue? Parental risk perception is logarithmically misaligned with actual pharmacological risk. Also, ‘pea-sized’ is a cognitive bias. FTU is the only valid metric. Case closed.
Alex Smith
Let’s be real-this post is basically a public service announcement disguised as a blog. And honestly? It’s about time. I used to think ‘more cream = faster healing’ until my nephew turned purple after I used benzocaine gel on his gums. Turned out, he was in methemoglobinemia. We got lucky-he made it. But now? I keep all meds locked up. I use FTUs. I use cold washcloths. And I tell every new parent I know: if it doesn’t come with a pediatric dosing chart, don’t touch it. You’re not being overcautious-you’re being responsible.
Roshan Joy
This is so important! 🙏 I’m from India and we use so many home remedies-turmeric paste, neem oil, even toothpaste on rashes. I had no idea some creams could be deadly for babies. I’ll start using FTU now and keep everything locked. Thank you for writing this. My niece is 7 months old and I was about to use that hydrocortisone from my drawer… now I won’t. 💙
Adewumi Gbotemi
Wow. I never knew. In Nigeria, we use a lot of herbal creams and sometimes adult medicines on babies because we think ‘it’s just a little’. This post made me stop and think. My baby has eczema. I will go to the doctor now and ask about the right cream. No more guessing. Thank you.
Matthew Miller
So let me get this straight: you’re telling me parents are dumb enough to use adult steroids on babies, wrap them in plastic, and then wonder why their kid collapses? This isn’t a ‘guide’-it’s a catalog of human stupidity. If you can’t follow basic medical advice, why are you a parent? The FDA should ban these products entirely and make every parent take a 3-hour course before they’re allowed to buy anything over the counter. This isn’t parenting. It’s Russian roulette with a tube of cream.
Madhav Malhotra
Love this post! As an Indian dad, I’ve seen so many relatives use ‘strong’ creams on kids because ‘it worked for me’. But kids aren’t mini-adults. I showed this to my mom and she actually listened-which is rare. Now we use only CeraVe and zinc oxide. And no more plastic wrap on diaper rashes. Simple, safe, and works. 😊
Priya Patel
I’m crying. Not because I’m sad-because I DID THIS. My daughter was 9 months old. I had leftover hydrocortisone 2.5% from my own eczema. I used it on her arms for a week because they were so red. She got so sleepy. I thought she was just tired. Turns out, her cortisol levels were tanking. We went to the ER. She’s fine now, but I’ve never felt so guilty in my life. I didn’t know. But now I do. Thank you for writing this. I’m sharing it with EVERYONE.
Jennifer Littler
FTU is the only valid metric. Period. I’m a nurse and I’ve seen too many kids admitted for iatrogenic adrenal suppression from ‘just a little cream’. The real tragedy? Most parents aren’t negligent-they’re misinformed. And the labeling on OTC products is a joke. I’ve held tubes with no age restrictions, no dosage info, no warnings. This isn’t about fear-mongering. It’s about standardization. If the FDA’s 2026 rules actually enforce clear dosing, we might finally see a drop in pediatric toxicities. Until then? Lock it up. Measure it. Don’t guess.