For years, doctors avoided prescribing statins to patients with liver disease. The fear was simple: statins are processed by the liver, so wouldn’t they make things worse? The truth is, that concern was based on outdated thinking. Today, we know statins aren’t just safe for people with chronic liver disease-they may actually help protect the liver while cutting heart attack and stroke risk. If you or someone you know has fatty liver, cirrhosis, or hepatitis and has been told statins are too risky, it’s time to rethink that advice.
How Statins Actually Work
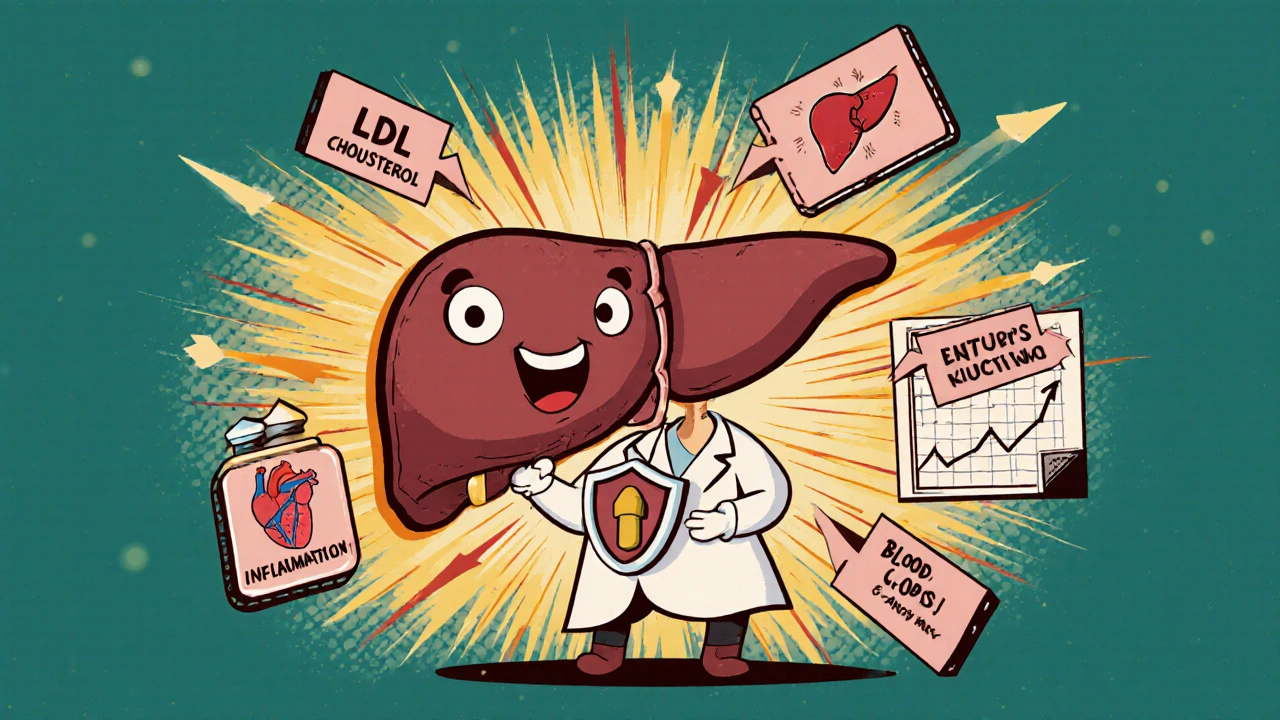
Statins are a class of drugs that lower LDL (bad) cholesterol by blocking an enzyme called HMG-CoA reductase. This enzyme is the main switch your liver flips to make cholesterol. When statins turn it off, your liver pulls more LDL out of your blood to compensate. That’s why high-intensity statins like atorvastatin or rosuvastatin can slash LDL by 50% or more. But that’s not all they do.
Statins also reduce inflammation in blood vessels, improve how the lining of arteries functions, and help prevent blood clots. These effects are called pleiotropic-meaning they go beyond just lowering cholesterol. For someone with liver disease, these extra benefits matter. Inflammation and stiff blood vessels are big problems in cirrhosis. Statins help fix both.
Why Statins Are Safe in Liver Disease
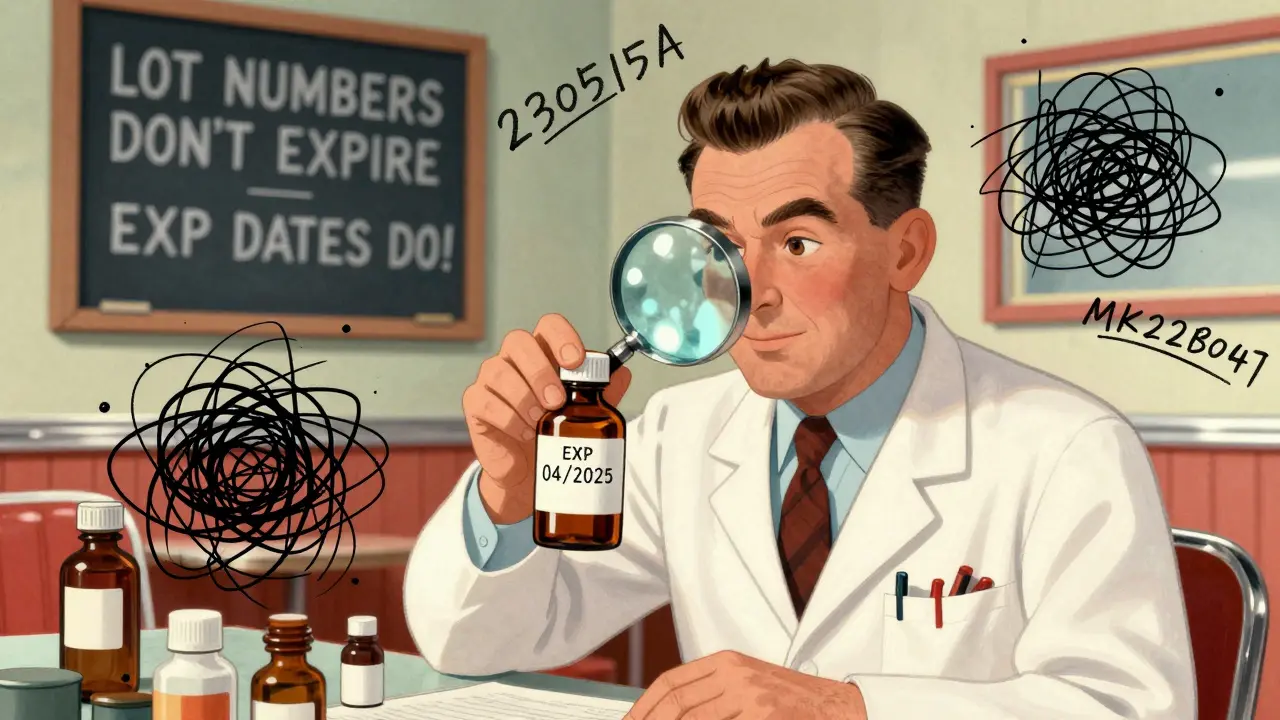
The biggest myth about statins and liver disease is that they cause liver damage. They don’t. In fact, severe liver injury from statins happens in about 1 out of every 100,000 patients per year. That’s rarer than being struck by lightning. Most cases of elevated liver enzymes on statins are mild, temporary, and don’t mean the drug is harming the liver.
Large studies back this up. The JUPITER trial followed 18,000 people on rosuvastatin for two years. The rate of liver-related side effects was the same as in the placebo group. The EXCEL trial with 8,000 patients on lovastatin found zero cases of serious hepatitis. Even in patients with cirrhosis, statins haven’t been shown to worsen liver function.
Doctors used to check liver tests every few months for patients on statins. That’s no longer recommended by the American Heart Association. Routine monitoring adds cost and anxiety without benefit. If your liver enzymes are only mildly elevated-up to three times the normal level-you can still safely take statins. Only in cases of active liver failure or unexplained, rapidly rising enzymes should you pause the medication.
Cardiovascular Benefits Outweigh Any Risk
People with chronic liver disease have a higher risk of heart disease than the general population. Why? Chronic inflammation, insulin resistance, and metabolic dysfunction that come with fatty liver or cirrhosis also damage blood vessels. Many patients with liver disease die from heart attacks or strokes-not liver failure.
Statins cut that risk. A 2023 study in Gastroenterology Research found that cirrhosis patients on statins had a 22% lower risk of dying from any cause, a 38% lower risk of variceal bleeding, and a 22% lower risk of liver decompensation. Another study in JAMA Network Open showed high-intensity statins reduced all-cause death by 17% in patients with liver disease compared to low-intensity ones.
Even more surprising: statins may help the liver itself. In animal models and small human studies, simvastatin improved blood flow through the liver by relaxing tight blood vessels. One study showed a 14% drop in liver blood pressure within 30 minutes of taking a single dose. That’s huge for people with portal hypertension-a dangerous condition where blood backs up in the liver.
Real Patient Experiences
Patients with liver disease aren’t just statistics. On forums like Reddit’s r/liverdisease and HealthUnlocked, people share what happens when they actually take statins. Of 58 cirrhosis patients on statins, 84% reported no liver-related side effects. Nearly a third said their liver enzyme levels improved after starting statins. One patient wrote: “My ALT dropped from 98 to 42 after six months on atorvastatin. My doctor couldn’t explain it-but I’m not complaining.”
Some patients report better energy, less fatigue, and fewer episodes of swelling in the legs. These aren’t just placebo effects. Improved blood flow and less inflammation can make a real difference in daily life. The most common side effect? Muscle aches. But even that happens in only about 12% of users with liver disease-same as the general population.
Which Statins Are Best for Liver Disease?
Not all statins are made the same. Some are broken down heavily by liver enzymes (CYP3A4), which can be a concern if you’re on other medications. For patients with liver disease, the safest choices are:
- Pravastatin-minimally metabolized by the liver, cleared by kidneys
- Rosuvastatin-mostly unchanged by liver enzymes, low interaction risk
- Pitavastatin-newer, low CYP metabolism, good safety profile
Avoid simvastatin and lovastatin if you’re on many other drugs-they’re broken down by CYP3A4, which can lead to interactions. Also, avoid grapefruit juice. It blocks the same enzyme and can raise statin levels dangerously.
Start low. For most patients with cirrhosis, begin with pravastatin 20 mg or rosuvastatin 5-10 mg. Reassess after 6-8 weeks. If tolerated, you can increase the dose. Even in advanced cirrhosis (Child-Pugh C), low-dose statins are often safe and beneficial.
Why Doctors Still Hesitate
Despite the evidence, many doctors still won’t prescribe statins to patients with liver disease. Why? Because they learned the old rules. Textbooks from the 1990s warned against statins in liver disease. That advice stuck. It takes time for science to change practice. Studies show it takes 18 to 24 months for new guidelines to become routine in clinics.
Another problem: polypharmacy. Patients with cirrhosis often take diuretics, beta-blockers, antibiotics, and supplements. Doctors worry about interactions. But with the right statin-pravastatin or rosuvastatin-those risks are minimal. The bigger risk is doing nothing.
Patients often have to advocate for themselves. One survey found 31% of liver disease patients had to push back when their doctor refused to prescribe statins. If your doctor says, “It’s too risky,” ask: “What’s the evidence behind that?” Point them to the AASLD 2022 guidelines or the 2018 American Heart Association statement. Both say statins are safe and beneficial.
What’s Next for Statins and Liver Disease?
The future looks promising. A major clinical trial called STATIN-CIRRHOSIS (NCT04567891) is currently underway. It’s tracking over 1,000 patients with decompensated cirrhosis to see if statins reduce hospitalizations and death. Results are expected in late 2025. Early data from smaller studies already suggest statins reduce liver-related deaths by nearly 30%.
Market data shows adoption is rising. In 2015, only 12% of statin prescriptions went to patients with liver disease. By 2023, that number jumped to 25%. Hepatologists are prescribing them more often. The European Medicines Agency updated its guidelines in 2021 to explicitly say statins are safe in stable liver disease. The FDA’s warning labels are slowly catching up.
Cost-wise, statins are a bargain. Generic versions like atorvastatin and pravastatin cost less than $10 a month. Compared to the $1,200-$3,500 in annual savings from preventing hospitalizations for liver complications, statins are one of the most cost-effective drugs in medicine.
Final Takeaway
If you have liver disease and need cardiovascular protection, statins are not just safe-they’re one of the best tools you have. They reduce heart attacks, strokes, and even liver complications. They don’t harm the liver. They may help it. And they’re cheap, well-studied, and widely available.
Don’t let outdated fears keep you from a life-saving treatment. Talk to your doctor. Ask for pravastatin or rosuvastatin. Start low. Monitor only if you feel unwell. And remember: the biggest risk isn’t the statin. It’s doing nothing.
Are statins safe if I have cirrhosis?
Yes, statins are safe for most people with cirrhosis, especially if it’s compensated (not actively failing). Studies show they reduce the risk of bleeding, liver failure, and death. Start with low doses like pravastatin 20 mg or rosuvastatin 5-10 mg. Avoid high doses in Child-Pugh C cirrhosis unless closely monitored.
Can statins cause liver damage?
No, statins do not cause progressive liver injury. Severe liver damage from statins is extremely rare-about 1 in 100,000 patients per year. Mild, temporary increases in liver enzymes happen in some people but usually resolve without stopping the medication. Routine liver testing is no longer recommended by major guidelines.
Which statin is best for someone with fatty liver disease?
Rosuvastatin or pravastatin are the top choices. They’re less dependent on liver metabolism, have fewer drug interactions, and are proven safe in non-alcoholic fatty liver disease (NAFLD). Both reduce liver fat and inflammation in studies, not just cholesterol.
Should I get my liver enzymes checked every month on statins?
No. The American Heart Association and American Association for the Study of Liver Diseases no longer recommend routine liver enzyme monitoring for patients on statins. Check them once before starting, then only if you develop symptoms like yellowing skin, dark urine, or severe fatigue.
Do statins help with portal hypertension?
Yes. Research shows statins reduce hepatic vascular resistance by improving blood flow in the liver. In one study, simvastatin lowered liver blood pressure by 14% within 30 minutes. This effect may help prevent dangerous variceal bleeding, a leading cause of death in cirrhosis.
What if my doctor refuses to prescribe statins because of my liver disease?
Ask for the evidence. Cite the 2018 American Heart Association Scientific Statement, the 2021 EASL guidelines, or the 2022 AASLD guidance-all of which support statin use in stable liver disease. If your doctor still refuses, ask for a referral to a hepatologist or cardiologist who specializes in liver disease. You have the right to evidence-based care.





Bruce Bain
So statins don't wreck your liver? Wild. I thought they were just one more pill making things worse. Guess I've been listening to the wrong people.
Dave Pritchard
This is exactly the kind of info people need to hear. So many folks with fatty liver are scared to take anything, but statins might actually be helping them more than they know. Keep spreading this.
deepak kumar
In India, we see so many patients with NAFLD who are told to avoid statins. This post is a game-changer. Pravastatin 20mg is my go-to now. No liver spikes, better lipid numbers. Simple science, not fear.
Duncan Prowel
The evidence presented here is methodologically robust and aligns with contemporary meta-analyses from the Journal of Hepatology and the European Association for the Study of the Liver. The pleiotropic effects of statins-particularly their modulation of endothelial nitric oxide synthase and reduction in hepatic stellate cell activation-provide a biologically plausible mechanism for their hepatoprotective properties in compensated cirrhosis. It is regrettable that clinical inertia persists despite Level 1 evidence.
Jonathan Gabriel
Wow. So the medical establishment finally caught up… 20 years late. I mean, I read a 2008 paper that said the same thing, but nooo, let’s keep telling people ‘your liver’s too weak’ while they die of heart attacks. Classic. Also, why is simvastatin still on the market if it’s basically a time bomb for people on meds? Pharma’s lazy, and doctors are scared to change. Sad.
benedict nwokedi
Statins are a corporate scam disguised as medicine… Big Pharma doesn’t want you to know that liver disease is caused by GMOs and 5G… and that statins are just a distraction so you keep paying for pills while your real problem-government toxins-goes unaddressed. Also, they’re linked to Alzheimer’s. Read the FDA’s hidden reports.
Timothy Uchechukwu
Why are white doctors prescribing statins to Africans? We have our own ways to heal. Our grandmothers used bitter leaf and neem. Why are we copying Western medicine that kills more than it helps? This is cultural imperialism wrapped in a lab coat.
Ancel Fortuin
They say statins are safe… but what about the 1 in 100,000? That’s still a human being. And who’s to say that ‘mild’ enzyme rise isn’t the start of something worse? They’ve lied about everything else-aspartame, vaccines, cholesterol-why should I trust them now? I’m not taking it. I’d rather die with my liver intact than live with a pill in my body.
Hannah Blower
It’s fascinating how the medical community clings to outdated dogma like it’s scripture. But let’s be honest-this isn’t about science. It’s about liability. Doctors don’t want to be sued if someone’s ALT rises 20 points. So they play it safe… by dooming their patients to heart attacks. Pathetic. And don’t get me started on how they still think ‘routine monitoring’ is meaningful. You’re not monitoring for safety-you’re monitoring for cover.
Gregory Gonzalez
How quaint. The ‘low-dose statin’ solution for cirrhosis. As if a $5 pill can undo decades of poor lifestyle choices and metabolic decay. The real tragedy isn’t the statin refusal-it’s the fact that we’ve turned medical care into a transactional, pill-pushing circus while ignoring root causes. You can’t statin your way out of a soda addiction.
Ronald Stenger
Statins are a Trojan horse. First they say they’re safe for the liver. Then they say they help the liver. Next thing you know, they’re pushing them for ‘anti-aging’ and ‘brain health.’ This is how they get you hooked. They want you dependent. Don’t be fooled. The liver doesn’t need help-it needs rest. And statins? They’re just another stressor dressed up like a hero.
Samkelo Bodwana
I’ve been reading this whole thing and honestly, I’m torn. On one hand, the data is incredibly compelling-statins reducing portal pressure, lowering death rates, even improving enzymes in some cases. But on the other hand, I’ve seen patients with decompensated cirrhosis who developed rhabdo after starting even low-dose rosuvastatin. It’s not that the science is wrong-it’s that medicine isn’t one-size-fits-all. We need to stop treating guidelines like gospel and start treating each patient like a unique human being with a unique liver, a unique drug history, a unique life. Maybe the answer isn’t ‘should we give statins?’ but ‘who, when, and how?’
Don Angel
Thanks for this. I’ve been telling my doc for months to prescribe me pravastatin. He said ‘too risky.’ I showed him the AASLD guidelines. He still hesitated. I’m not mad-I’m just… disappointed. I’m starting tomorrow. No more fear. Just facts. And a little hope.