Kidney Disease Overview
When talking about Kidney Disease, a condition where the kidneys lose their ability to filter waste, balance fluids, and regulate electrolytes. It’s also called renal disease. Hypertension, high blood pressure that often arises as both a cause and a consequence of kidney dysfunction and Urinary Incontinence, the loss of bladder control that can signal worsening kidney health are tightly linked, while Dialysis, the mechanical filtration process used when kidneys can’t clean the blood represents the last‑ditch therapy for many patients. In short, kidney disease often leads to hypertension, hypertension can accelerate renal damage, and both can trigger urinary symptoms that may require dialysis when the kidneys fail.
How Kidney Disease Connects to Everyday Health Concerns
Most people notice kidney disease only after a routine blood test shows elevated creatinine or reduced glomerular filtration rate. The silent nature of the condition means you might first experience fatigue, swollen ankles, or frequent urination. Those signs usually overlap with other common issues. For instance, high blood pressure medications like lisinopril (often discussed in our hypertension guides) can protect the kidneys by lowering the pressure in the tiny filtering units. On the flip side, over‑use of non‑steroidal anti‑inflammatory drugs, a topic we cover in our pain‑management articles, can damage kidney tissue and raise the risk of chronic renal failure.
Urinary symptoms often tell a story before lab values do. Bladder spasms triggered by caffeine, as explained in our caffeine‑bladder article, can increase pressure on the kidneys and worsen protein leakage. Pelvic floor training, another focus of our content, helps strengthen the muscles that support bladder control, reducing the strain on the kidneys and potentially slowing disease progression. When kidney function declines, waste builds up, leading to itching, nausea, and a heightened susceptibility to infections – a point we stress in the antibiotic guides.
When the kidneys can’t keep up, dialysis becomes a lifeline. We break down the two main types – hemodialysis and peritoneal dialysis – in plain language, highlighting the lifestyle adjustments each requires. Understanding when to start dialysis is crucial; early referral can preserve quality of life and give patients more choices about treatment settings. Alongside dialysis, kidney transplant remains the gold standard, but donor availability and immunosuppressive therapy—topics covered in our medication safety posts—add layers of complexity.
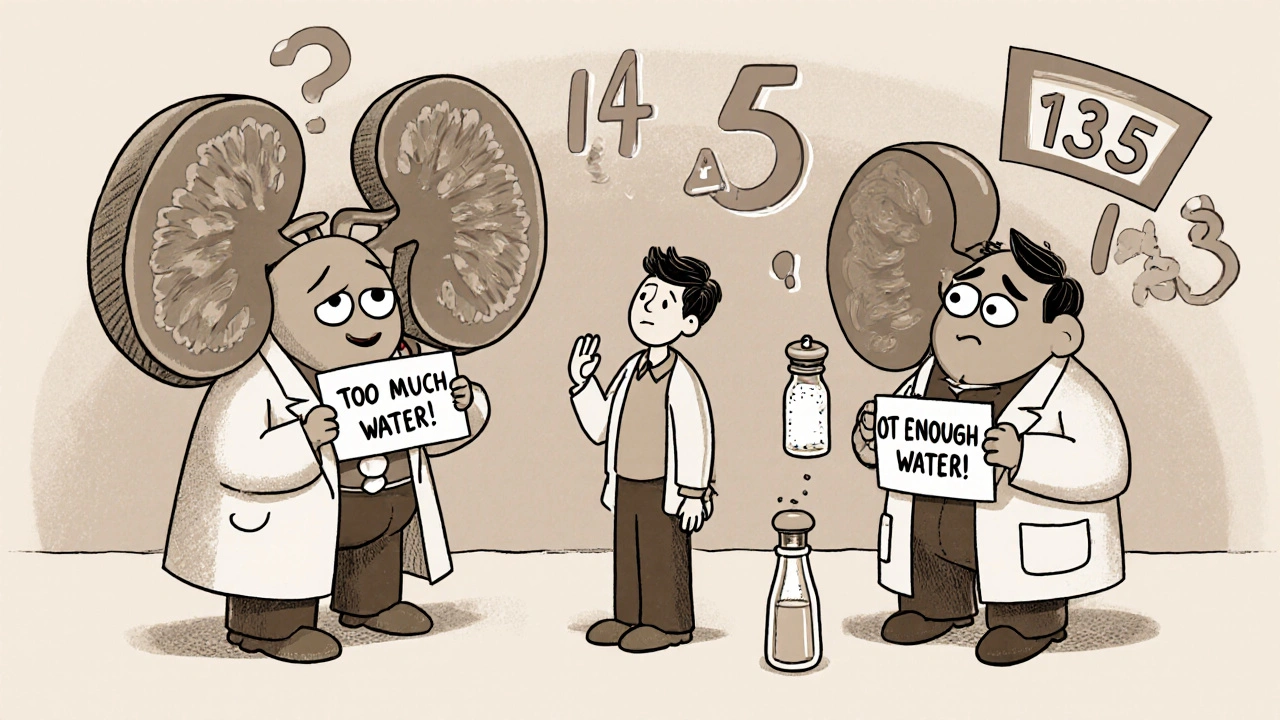
Beyond the medical side, lifestyle plays a huge role. A low‑salt diet, regular aerobic exercise, and staying hydrated (but not over‑hydrated) are simple steps that keep blood pressure down and reduce the workload on the kidneys. Our nutrition articles often mention foods rich in potassium and phosphorus, nutrients that need careful monitoring once kidney disease sets in. Managing diabetes, another major cause of renal failure, is discussed in many of our diabetes‑related guides, emphasizing tight glucose control to protect kidney health.
Putting all these pieces together, this collection of articles gives you a roadmap: from recognizing early warning signs, through managing related conditions like hypertension and urinary incontinence, to navigating advanced therapies such as dialysis and transplant. Below you’ll find practical advice, drug comparisons, and lifestyle tips that together form a comprehensive resource for anyone dealing with kidney disease or looking to prevent it.
Hyponatremia and Hypernatremia in Kidney Disease: What You Need to Know
Hyponatremia and hypernatremia are common, dangerous complications in kidney disease. Learn how fluid balance, diet, and medications affect sodium levels-and what you can do to stay safe.
How High Blood Pressure Triggers Kidney Disease: What You Need to Know
Learn how high blood pressure damages kidneys, spot early signs, and discover lifestyle and medication steps to prevent chronic kidney disease.