Fungal Skin Discoloration Risk Calculator
Your Risk Assessment
When you spot a strange patch of color on your arm or foot, the first thought is often a stain or a bruise. But sometimes the culprit is a tiny fungus that’s thriving in the right environment. Fungal skin discoloration is a condition where skin pigments shift because a fungal infection alters melanin production or causes inflammation that looks darker or lighter. Understanding why fungi love certain spots can help you stop the problem before it spreads.
Key Takeaways
- Humidity, warmth, and sweat create the perfect playground for skin‑loving fungi.
- Changes in skin pH, friction from clothing, and UV exposure can tilt the balance toward discoloration.
- Identifying the specific fungus (e.g., Candida albicans vs. Trichophyton rubrum) guides treatment and prevention.
- Simple environmental tweaks - like controlling indoor humidity and choosing breathable fabrics - dramatically lower risk.
- Seek medical advice if patches persist beyond two weeks or are accompanied by itching, scaling, or pain.
Why Environment Matters for Skin Fungi
Fungi are not picky about where they live; they simply need moisture, a food source, and a temperature range that supports growth. Your skin provides all three, but the surrounding environment can push a harmless resident into overdrive, leading to visible discoloration.
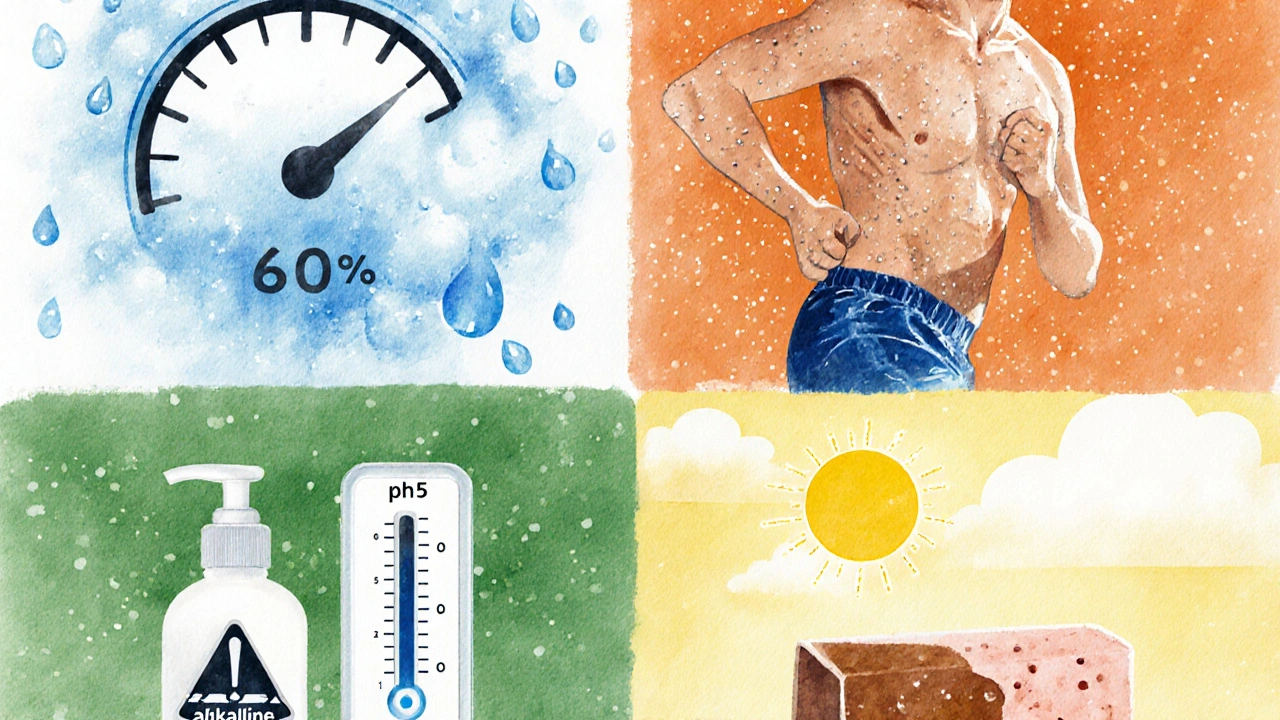
1. Humidity - the silent accelerator
Air that holds more than 60% relative humidity supplies the water fungi need to reproduce. Studies from dermatology clinics in tropical cities show a 40% higher incidence of fungal patches during rainy seasons. When humidity spikes, the outer skin layer (stratum corneum) swells, creating micro‑cracks that let fungi infiltrate deeper layers.
2. Temperature - where heat meets skin
Most skin‑loving fungi thrive between 20°C and 30°C (68°F‑86°F). That’s why you often see discoloration on feet after a long day in closed shoes or on the back after a workout. A steady warm environment shortens the fungal life cycle from weeks to days.
3. Sweat - the natural moisturizer that can backfire
When you sweat, you release not just water but also salts, fatty acids, and proteins that become food for fungi. Sweat also lowers surface pH, creating a mildly acidic environment that many yeasts love. Athletes and people who wear tight, non‑breathable clothing are especially vulnerable.
4. Skin pH - the chemical thermostat
Healthy skin typically sits at a pH of 4.5‑5.5, a range that keeps many microbes in check. When pH climbs above 6-often after prolonged exposure to alkaline soaps or detergents - the protective acid mantle weakens, allowing fungi like Malassezia furfur to proliferate and cause a condition known as pityriasis versicolor, which appears as light‑ or dark‑spotted patches.
5. UV Radiation - a double‑edged sword
Sunlight kills many pathogens, but its effect on skin fungi is nuanced. Low‑to‑moderate UV exposure can suppress fungal growth, yet intense UV can damage the skin barrier, making it easier for fungi to invade. Moreover, UV‑induced melanin changes can mask or accentuate discoloration, confusing diagnosis.
6. Clothing material and friction
Synthetic fabrics trap heat and moisture, while tight seams cause friction that disrupts the epidermis. A common scenario: a runner develops a dark, scaly patch on the inner thigh where a polyester shirt rubs against skin. Switching to moisture‑wicking, breathable cotton can reverse the trend.
Common Fungi Behind Skin Discoloration
Not all fungi act the same way. Knowing which organism you’re dealing with helps you pick the right prevention strategy.
| Fungus | Typical Color Change | Preferred Environment | Common Body Sites |
|---|---|---|---|
| Candida albicans | Red to brown patches, sometimes with a raised edge | Warm, moist areas; high sugar levels | Skin folds, under breasts, groin |
| Trichophyton rubrum | Darkened, sometimes cracked plaques | Temperatures 22‑28°C, moderate humidity | Feet (athlete’s foot), nails, elbows |
| Malassezia furfur | Hypopigmented (lighter) or hyperpigmented (darker) macules | Oily skin, high humidity, cool temperatures | Upper trunk, shoulders, back |
Practical Ways to Control Environmental Triggers
Once you know the key players, you can start tweaking your surroundings.
- Manage indoor humidity. Use a dehumidifier to keep levels below 50% during rainy months. A hygrometer is cheap and tells you when the air is too damp.
- Keep skin dry. After showering, pat skin dry, especially in creases. For athletes, bring a quick‑dry towel and change out of sweaty clothes within an hour.
- Choose breathable fabrics. Natural fibers like cotton and bamboo let sweat evaporate. Look for clothes labeled “moisture‑wicking” for workouts.
- Balance skin pH. Use mildly acidic cleansers (pH5‑5.5). Avoid harsh soaps that strip the acid mantle.
- Regulate temperature. In hot climates, use fans or air conditioning. When outdoors, wear loose‑fitting shoes that permit airflow.
- Limit prolonged UV exposure. Apply broad‑spectrum sunscreen (SPF30+) daily, even on cloudy days. Reapply after swimming or heavy sweating.
- Maintain good skin barrier. Apply a thin layer of fragrance‑free moisturizer after bathing to restore lipids.
When to Seek Professional Help
If patches persist beyond two weeks, spread despite home measures, or are accompanied by itching, peeling, or pain, it’s time to consult a dermatologist. A simple skin scraping under a microscope can identify the exact fungus. In many cases, topical azoles (e.g., clotrimazole) or oral antifungals are prescribed for faster clearance.
Prevention Checklist
- Check bathroom and locker room floors for moisture; wipe dry before use.
- Rotate shoes; let them air out for at least 24hours after each wear.
- Use antifungal powders in shoes and on sweaty areas.
- Wash workout clothes after each use; avoid leaving them in a gym bag.
- Keep outdoor gear (boots, gloves) clean and dry.
Frequently Asked Questions
Can fungal skin discoloration become permanent?
If the fungus is left untreated for months, it can cause lasting pigment changes or scarring. Early treatment usually restores the original color within weeks.
Do over‑the‑counter creams work for all types of fungal discoloration?
Topical azoles work well for Candida and Trichophyton infections on the skin. However, deeper infections or those caused by Malassezia often need prescription‑strength creams or oral medication.
Is it safe to use home remedies like tea tree oil?
Tea tree oil has antifungal properties, but its concentration matters. Diluting it to 5% with a carrier oil reduces skin irritation. Still, for widespread discoloration, medical treatment is more reliable.
How quickly can I expect improvement after starting treatment?
Most topical treatments show visible lightening within 3‑5 days, but full resolution may take 2‑4 weeks, depending on the fungus and how well environmental factors are controlled.
Are there any lifestyle habits that increase the risk?
Frequent use of tight synthetic shoes, neglecting foot hygiene, staying in humid environments without ventilation, and using heavily alkaline soaps all raise the odds of fungal skin discoloration.
By keeping humidity low, staying cool, and letting skin breathe, you cut off the fungus’s playground. If you notice fungal skin discoloration, check the environment first - it’s often the missing piece in the puzzle.


Lawrence D. Law
The data suggests a direct correlation between indoor humidity and fungal proliferation.
Mary K
Hey there, fellow skin adventurers! 🌈 The world of fungal discoloration is like a hidden rainforest, teeming with mystery and vibrant lessons. Dive into the humidity, sweat, and sun-each a brushstroke on the canvas of our dermal art. Remember, a breathable wardrobe is your ally, and a splash of sunscreen is your magical shield. Keep exploring, stay radiant, and let your skin tell a story of health and color!
Odin Zifer
Everyone ignores the shadowy agenda behind those humidity meters they push on us. It's not just comfort, it's control, a way to stir up fungal spores for profit. The sweat data is a cover story, they want us thinking it's about exercise when it's about surveillance. Stay alert, question the numbers.
Marisa Leighton
Great points on the humidity factor! I’d add that rotating your socks daily can dramatically cut fungal build‑up-think of it as giving your feet a fresh stage each day. Also, consider a quick post‑workout shower; it’s like a curtain call for excess moisture. Keep the optimism flowing, and you’ll see the skin tone brighten in no time!
Brennan Keeler
Look, the riskcalc is a bit oversimplifed-there are more parameters like microclimate and skin microbiota poducts. Also, the jargon about "synthetic fabrics" is vague; we need to differentiate polyester from nylon, they have diffrent breathability. Dont overlook the fact that high humidity can also trigger other skin conditions, not just fungi. The calc should be updated asap!
Chelsea Hackbarth
Did you know that the average person sweats about 1‑2 liters per day? 🤓 Managing that with proper ventilation and quick‑dry fabrics can slash fungal risk by nearly 40% according to recent studies. Just a friendly reminder!
Adam Shooter
The presented algorithm suffers from a lack of statistical rigor; a Bayesian approach would better quantify uncertainty. Moreover, the linear weighting of humidity and sweat fails to capture interaction effects. A multivariate regression could reveal non‑linear dynamics, enhancing predictive fidelity.
Shanmughasundhar Sengeni
Dude, the whole thing feels half‑baked. They throw in "UV exposure" like it’s a side dish, but forget that UVA penetrates deeper and can mess with skin flora. Also, who’s even using synthetic fibers in 2024? People know cotton is king. Just saying.
ankush kumar
Alright, let me break this down step by step, because the nuances matter. First, indoor humidity isn’t just a number on a slider; it reflects the macro‑environmental equilibrium that governs fungal spore viability. When humidity climbs above 70%, the moisture gradient across the epidermis becomes favorable for dermatophyte proliferation, essentially creating a micro‑habitat akin to a tropical rainforest right on your skin. Second, sweat exposure, while often dismissed as a trivial byproduct of activity, actually introduces a cocktail of electrolytes and lipids that serve as a nutrient source for the fungi, accelerating colonization. Third, clothing choice plays a pivotal role: natural fibers like cotton allow for capillary action, drawing sweat away and facilitating evaporation, whereas synthetic blends trap moisture, turning your shirt into a humid incubator. Fourth, ultraviolet exposure introduces both protective and detrimental effects-the UVB component can reduce fungal load, but UVA can penetrate deeper, potentially compromising the skin’s barrier function and indirectly encouraging fungal colonization. Fifth, the interaction between these variables is not merely additive; there is a synergistic effect where high humidity combined with prolonged sweat exposure and synthetic clothing exponentially raises risk, far beyond the sum of individual contributions. Sixth, personal habits such as showering frequency, use of antimicrobial soaps, and post‑exercise drying routines can modulate this risk curve significantly. Seventh, geographic considerations matter: regions with naturally high ambient humidity will exacerbate indoor conditions unless dehumidifiers are employed. Eighth, the calculator’s scoring system, while helpful, could benefit from weighting adjustments based on recent epidemiological data showing a shift in fungal species prevalence. Ninth, individuals with compromised immune systems or underlying dermatological conditions should treat even low‑risk scores with caution, as their susceptibility is inherently higher. Tenth, the psychological impact of skin discoloration should not be overlooked-self‑esteem can be affected, leading to a feedback loop where stress may further impair skin immunity. Eleventh, lifestyle interventions such as regular exercise (which promotes circulation) and a balanced diet rich in antioxidants can bolster skin resilience. Twelfth, it’s advisable to incorporate routine skin examinations, especially after periods of high humidity, to catch early signs of fungal overgrowth. Thirteenth, the use of breathable footwear and moisture‑wicking socks is crucial for foot health, as the plantar surface is a common site for fungal infections. Fourteenth, remember that the environment is dynamic; periodic reassessment of your risk profile is essential as seasons change. And finally, while tools like this calculator are valuable, they are supplements-not substitutes-for professional medical advice when concerning skin changes arise.
Fae Wings
Wow, that was an insightful dive! 🌟 I can totally picture the skin as a tiny ecosystem, each factor shaping its story. It’s amazing how something as simple as a shirt material can make such a difference. Thanks for the thorough breakdown!
Anupama Pasricha
I appreciate the comprehensive view; it’s clear that humidity, sweat, and fabric interact in a complex matrix. Maintaining balanced indoor conditions and opting for breathable fabrics can help mitigate fungal risks.
Bryce Charette
Great summary above! Just a quick tip: keep an eye on spelling in your logs-accurate records help track patterns over time.
Christina Burkhardt
For anyone looking to implement these suggestions, start with a simple humidity monitor and a laundry routine that favors natural fibers. Small steps lead to big improvements.
liam martin
Ah, the drama of skin tone-our very own chiaroscuro! Yet beneath the theatrics lies a simple truth: moisture reigns supreme.
Ria Ayu
Think of the skin as a canvas, and the environment as the artist’s palette; each hue tells a story of balance or excess.