ACE Inhibitor Overview
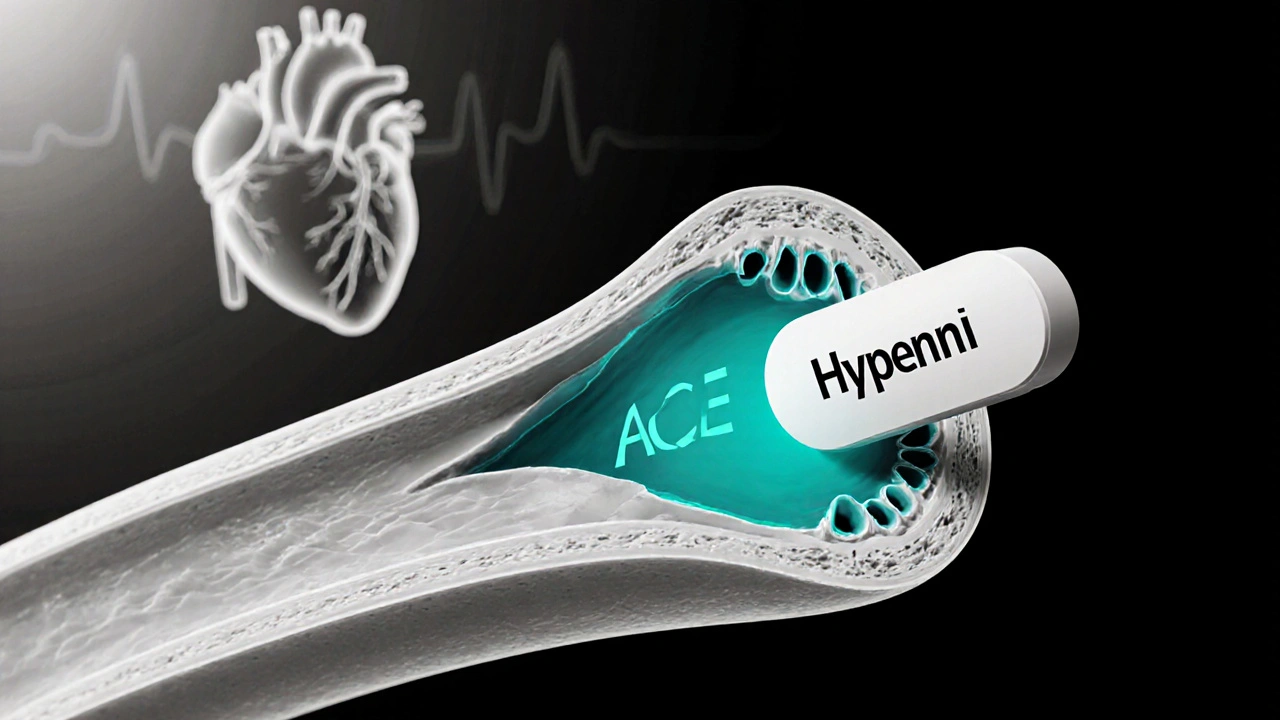
When working with ACE inhibitor, a class of medication that blocks the enzyme converting angiotensin I into angiotensin II, helping to relax blood vessels. Also known as angiotensin‑converting enzyme inhibitor, it plays a central role in managing blood pressure, the force of blood against artery walls, a key vital sign and the broader Renin‑Angiotensin‑Aldosterone System, a hormonal cascade that regulates fluid balance and vascular tone. In plain terms, an ACE inhibitor lowers blood pressure by stopping the body from making a potent constrictor called angiotensin II.
Why ACE Inhibitors Matter for Hypertension
High blood pressure strains the heart and kidneys, paving the way for heart attacks and kidney failure. By blocking the conversion of angiotensin I to angiotensin II, ACE inhibitors widen arteries, making it easier for blood to flow. This simple chemical halt translates into real‑world outcomes: fewer strokes, lower risk of heart enlargement, and slower progression of kidney disease. The RAAS influences blood pressure at every step, so interfering with one key enzyme ripples through the whole system, delivering a steadier, safer pressure level.
Most people first hear about ACE inhibitors through drug names like Ramipril, Lisinopril, or Enalapril. These are the everyday versions you’ll see on pharmacy shelves. They share the same core action but differ in dosing frequency, half‑life, and how they’re cleared from the body. For example, Lisinopril is taken once a day and works well for patients with stable kidney function, while Ramipril may be chosen for its proven benefit in post‑myocardial infarction care. Knowing which one fits your lifestyle can make a big difference in staying consistent with therapy.
Side effects are usually mild, but they deserve a shout‑out. The most common complaint is a dry cough, caused by increased bradykinin levels when the enzyme is blocked. If the cough becomes bothersome, doctors often switch to an ARB, which blocks the same pathway downstream. A rarer but serious risk is high potassium (hyper‑kalemia), especially if you’re already on a potassium‑saving diuretic. Routine blood tests help catch any imbalance early, ensuring the medication stays a help, not a hindrance.
Beyond blood pressure, ACE inhibitors shine in treating heart failure. When the heart can’t pump efficiently, the body ramps up the RAAS, which actually makes the problem worse by tightening vessels and retaining fluid. An ACE inhibitor breaks this loop, lowering the heart’s workload and improving survival rates. Clinical trials repeatedly show reduced hospital visits and longer life expectancy for patients on these drugs. The same logic applies to chronic kidney disease—by easing pressure in the glomeruli, ACE inhibitors slow the loss of filtration capacity and delay the need for dialysis.
Starting an ACE inhibitor usually involves a low dose, then a gradual increase based on blood pressure readings and kidney function tests. Lifestyle tweaks—like cutting back on salty foods, staying active, and limiting alcohol—boost the drug’s effect without extra pills. Patients with diabetes should keep an eye on kidney labs, as the combination of high sugar and RAAS blockade can hide early signs of renal stress. Communication with your healthcare provider is key; they’ll adjust the dose or switch meds if side effects crop up.
Below you’ll find a curated list of articles that dig deeper into topics we’ve just brushed on. Whether you’re curious about how ACE inhibitors compare to other blood pressure drugs, want to understand their role in kidney health, or need practical tips for managing side effects, the posts ahead cover it all. Dive in to get actionable insights and make the most of your medication plan.
Hypernil (Lisinopril) vs Other Hypertension Drugs: Detailed Comparison
A side‑by‑side look at Hypernil (lisinopril) compared with common blood‑pressure meds, covering effectiveness, side effects, dosing and cost.